Torsion of the testicle (TT) is one of the urological emergencies requiring immediate surgical intervention due to the risk of losing the organ. Nevertheless, there are reports of potential benefits of scrotoscopy in the diagnosis of TT [1]. Typical symptoms include severe and sudden pain in the scrotal area, scrotal swelling, testicular rotation, and negative Prehn’s sign [2]. TT is caused by a torsion of the spermatic cord resulting in ischemia and subsequent necrosis of the testicle. An additional predisposing factor is a bell clapper deformity [3, 4]. Furthermore, there are some anatomical differences between the two testicles. The left testicle has a longer left testicular vein running into the left renal vein instead of directly into the inferior vena cava, as it is in the right testicle [5]. According to the literature, the time from first symptoms onset to successful surgery varies between 4 and 8 hours [6]. Therefore, the most important role is played by the timing of the patient’s presentation to the hospital and the correct medical diagnosis in order to maximize the chances of preserving the affected testicle [7]. Furthermore, to decrease the risk of reduced fertility [8, 9].
It is estimated that TT most commonly occurs in infancy and teenage years, and rarely affects men over the age of 40 [10]. Nevertheless, all men, regardless of age, are at risk for TT. In the differential diagnosis, an excellent tool for confirming TT is a color Doppler ultrasound of the scrotum using a linear transducer, with a sensitivity approximately 91% and a specificity approximately 89% [11–15]. In cases of delayed arrival at the hospital, the ischemic testicle cannot be salvaged, so orchidectomy is performed. Orchidopexy, which involves immobilizing the testicle in the scrotum, is a therapeutic solution before irreversible necrotic changes occur. This study aimed to confirm proven correlations and analyze existing testicular torsion cases based on local clinical material in order to reduce the time to diagnosis and accelerate surgical intervention in future patients.
We retrospectively examined 32 cases of testicular torsion in adult men between Dec. 1, 2019, and Dec. 3, 2024, who were surgically treated in the urology department. Data was obtained from the hospital information system. Inclusion criteria included patients with a diagnosis of N44 code for testicular torsion according to the ICD-10 classification. Exclusion criteria included patients who, despite the diagnosis of testicular torsion, did not require surgery. All patients were informed about and consented to the surgical procedures. Data included the patient’s age, time of arrival at the hospital, and performance of surgery, medical history, physical examination, ultrasound findings, type and side of surgery, and histopathological examination (HPE) after the orchidectomy. The study’s limitations are: it was a single-center study, patients were diagnosed and operated on by several different urologists, and data extracted from medical histories did not always include all potential TT symptoms.
The Shapiro-Wilk test was used to determine the normality of the distribution. For homogeneity of population variance, Levene’s test was used. For homogeneity of variance, the ANOVA for independent groups test was used. For heterogeneity of variance, the ANOVA for independent groups with the F* adjustment test was used. The McNemar test was used to examine differences in the frequency of a particular type of surgery and the side of the testis operated on. A Spearman Correlation test was used to see if age affected the time a patient reported to TRIAGE. To examine whether patients undergoing orchidectomy or orchidopexy significantly differed in the time the procedure was performed, the ANOVA for independent groups with the F* adjustment test was used. To examine whether the populations of patients undergoing a particular surgery significantly differ in the prevalence of given symptoms, the chi2 test or Fisher’s exact test was performed.
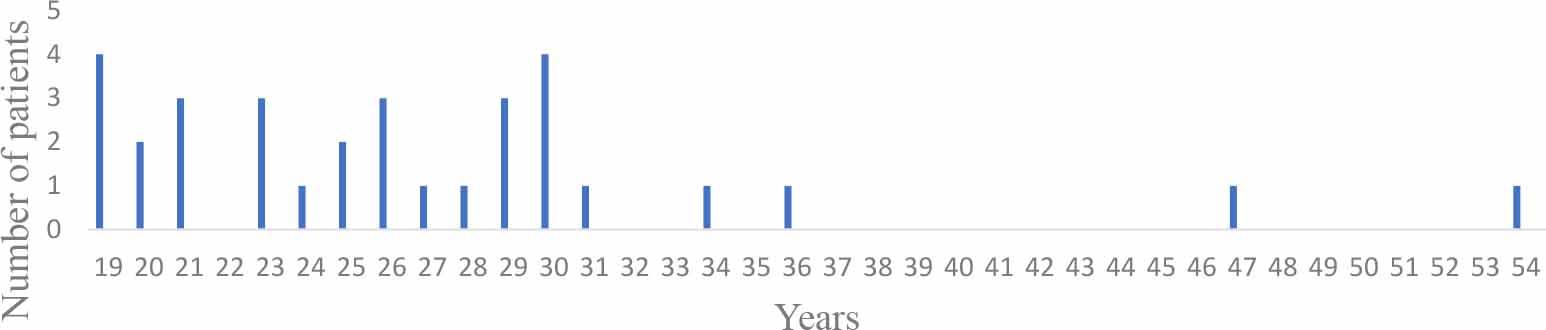
Age of patients.
The median age of patients was 26 years (19-54). The median time from symptom onset to ED presentation was 13 hours and 10 minutes (1-480 hours). The median time from arrival at TRIAGE to surgery was 3 hours and 5 minutes (0.83-29 hours). Comparing the timing metrics, the median time to TRIAGE in patients undergoing orchidopexy was 2 hours 30 minutes (1-48 hours) – Figure 2, while for those undergoing orchidectomy, it was 48 hours (2-480 hours) from symptom onset. Additionally, the median time from TRIAGE to orchidopexy was 1h 30 mins (0.83-4 hours). The median time from TRIAGE to orchidectomy was 4h 15mins (2-29 hours). The three most common physical examination findings were: no blood flow on color Doppler in the torsed testicle (96.9%), scrotal pain (87.5%), and testicular swelling (43.8%). Of the 32 cases of TT, orchidectomy was performed in 19 patients (59.4%), and orchidopexy in 13 men (40.6%). Age had no impact on the type of surgery performed (p=0.197). Furthermore, there were no statistically significant differences in the frequency of orchidectomy or orchidopexy (p=0.38). However, the patient’s age was moderately positively correlated with the time to report to TRIAGE (p=0.016; Spearman’s R=0.42). Older men presented significantly later to the hospital. Only 50.0% of patients were surgically treated within the recommended time window for salvaging an ischemic testicle - Figure 3. The latest successful orchidopexy was performed 6 hours and 45 minutes after symptom onset. Orchidopexy patients reported significantly earlier to TRIAGE from symptom onset than orchidectomy patients (p=0.017). Orchidopexy patients had significantly shorter times from TRIAGE to surgery than orchidectomy patients (p=0.026). Therefore, the total time from symptom onset to the surgery was significantly longer in orchidectomy patients (p=0.013). In addition, the right testicle was more commonly involved in torsion (n=24, 75%, p=0.008). There were no significant differences between the type of surgery and the incidence of testicular edema (p=0.82). There were no significant differences between the type of surgery and the incidence of testicular pain (p=0.17). There were no significant differences between the type of surgery and the incidence of testicular enlargement (p=0.069). There were no significant differences between the type of surgery and the absence of blood flow on color Doppler in the affected testicle (p=0.48). Nonetheless, an echogenically heterogeneous testis was significantly more common among orchidectomy patients (p=0.001). Histopathological examination following orchidectomy revealed 13 (68.4%) cases of hemorrhagic necrosis of the testis and/or epididymis and/or spermatic cord with concomitant purulent inflammation in three (15.8%) patients. Additionally, four (21.1%) cases of testicular and/or epididymal and/or spermatic cord hematoma, one case of testicular and epididymal abscess (5.3%), and one case of mature and immature teratoma pT1, yolk sac tumor (5.3%).
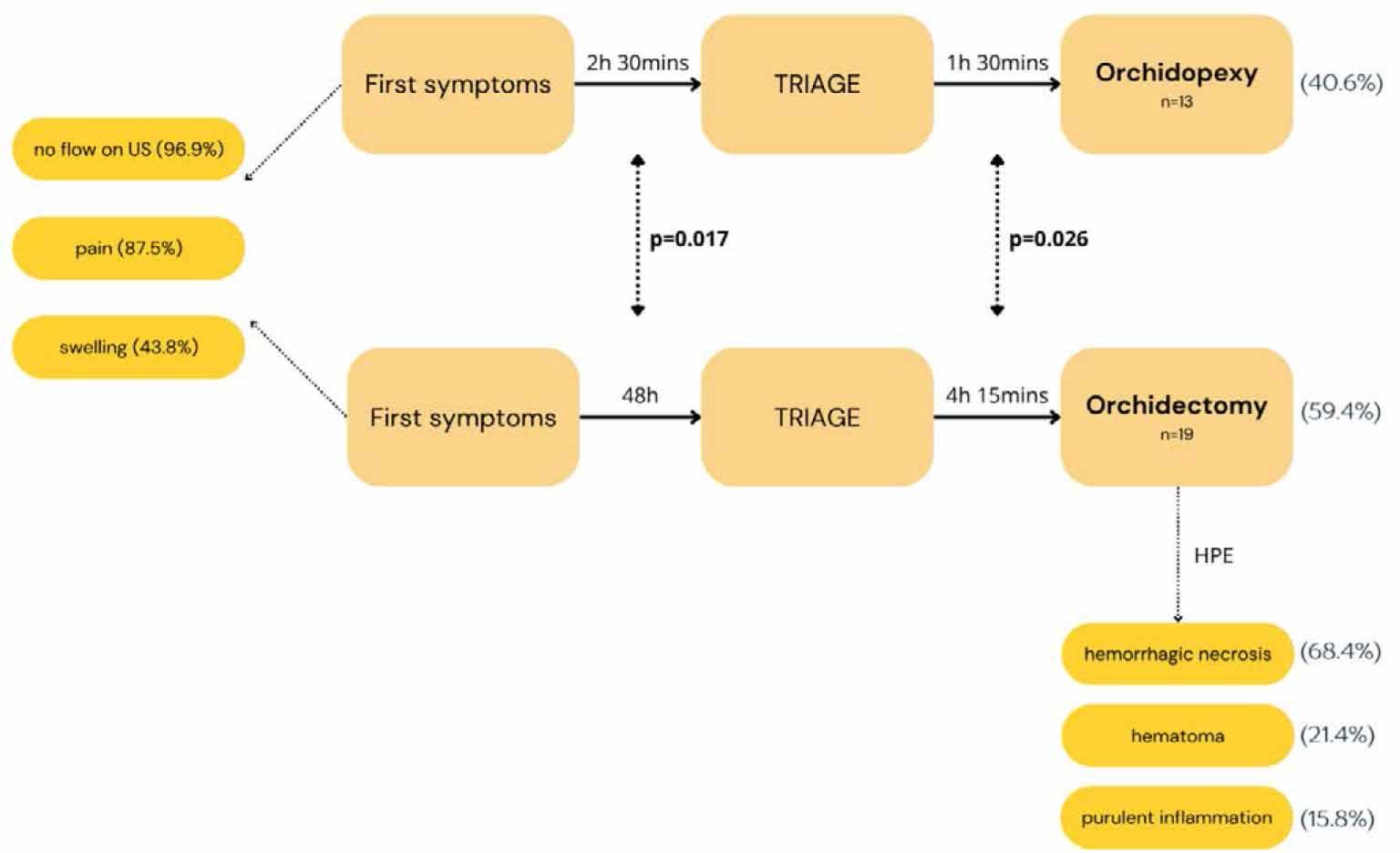
Diagnostic pathway with the most common symptoms and histopathological results.
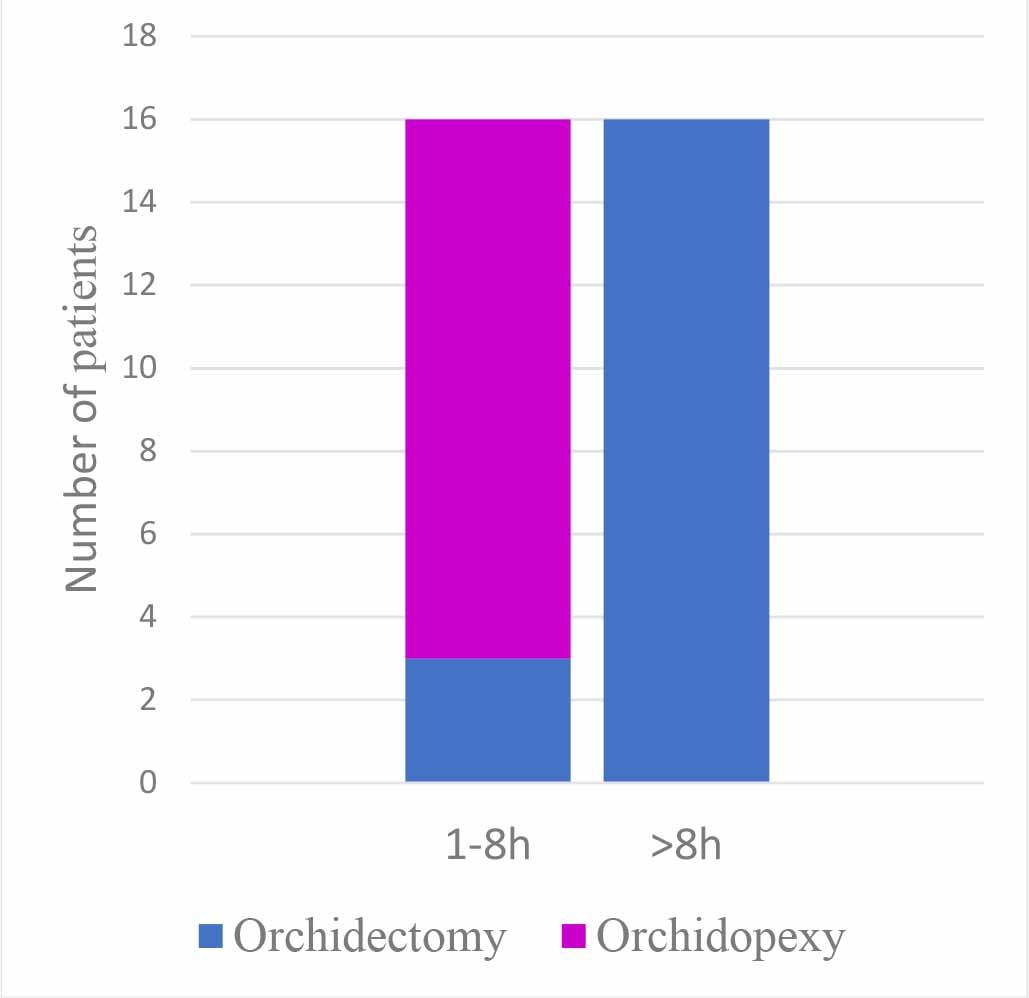
Percentage of patients surgically treated in the first 8 hours after the onset of first symptoms.
Our manuscript addresses an important clinical issue. Adult patients with TT are encountered both in emergency departments and outpatient clinics, and due to their age, the diagnosis of testicular torsion may be delayed. This study indicates that TT is not a condition that occurs only in a specific age group. The median age was 26 years old however, TT was also diagnosed in a person aged 54. Of the 16 patients who underwent surgery within 8 hours of the symptom onset, only 18.8% had to have an orchidectomy. The median arrival time of 13h and 10 mins is far too long. This emphasizes the crucial importance of timely presentation for successful treatment [6]. In our study, the percentage of saved testicles was 40.6%. This is comparable to the work of Cummings J. et al. [16] in which the percentage was 41% in men aged 21-34. The same work also analyzed presentation time and, as in our study, observed that older age was associated with later presentation to the hospital. The latest orchidopexy was performed after 6h 45 minutes. Rampaul M. et al. [17] report information about the salvaged testicle after 6 hours. Nevertheless, the percentage of orchidopexy was much lower than ours (40.6%), amounting to 27.3%. The median duration of symptoms in orchidectomy patients was also lower at 42 hours compared to ours at 48 hours. In a publication describing 89 cases of testicular torsion, orchidectomy was needed for 18% of patients [18]. This is a much better result correlated to our population, where the orchidectomy rate was 59.4%. Moreover, the loss of a testicle is associated not only with health consequences as well as psychological ones. The study by Skoogh J. et al. [19] on orchidectomy patients showed that testicular loss is associated with feelings of shame and embarrassment, especially among those who were not offered a prosthesis. Therefore, it is so important to raise public awareness about the potential dangers of pain in the intimate area. Considering that the available literature indicates an insufficient level of knowledge regarding TT among adults [20, 21]. In our study, torsion of the right testicle accounted for 75% of all cases. An interesting result seeing that available publications suggest a higher incidence of torsion in the left testicle [22]. Nonetheless, it still leaves space for further investigation [23, 24]. Other authors also report that symptoms concomitant with TT may be vomiting, diarrhea, or dysuria [24, 25]. In our analysis, we did not observe the occurrence of the above symptoms. In our research, no color Doppler blood flow in TT occurred in 96.9% of patients, confirming the excellent utility of this test in TT diagnosis [10–14]. However, it should not be underestimated that there are cases of intermittent TT that may have normal color-Doppler flow during the examination [26].
In summary, the average time to ED presentation prevents testicular salvage in half of the patients. Therefore, it is essential to raise patient awareness of the alarming signs of suspected TT, particularly among older men, to avoid irreversible consequences. In addition, continuous improvement in the training of medical personnel is needed to reduce the time to diagnosis and accelerate surgical intervention when necessary. We strongly recommend that any suspected TT, regardless of age, warrants immediate ultrasound examination of the testicles with assessment of blood flow. Symptoms that aid diagnosis include sudden, severe pain and swelling of the scrotum. In addition, medical staff should always obtain detailed information about when the first symptoms appeared. It would also be beneficial to add testicular torsion in adults as a critical condition in urology curricula in medical schools.