Gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NENs) are rare neoplasms that occur sporadically or are inherited. These tumors can also be associated with hereditary syndromes[1]. One example of this is multiple endocrine neoplasia type 1 (MEN 1), a hereditary disorder characterized by a predisposition to tumors predominantly within the parathyroid glands, pituitary gland, and endopancreatic endocrine cells [2].
MEN 1 diagnosis can be established based on the coexistence of “(…) two or more primary MEN 1-associated endocrine tumors (i.e. parathyroid adenoma, enteropancreatic tumor, and pituitary adenoma)”[2]. In the context of familial MEN 1, the presence of just one of the primary MEN 1 tumors and a first – degree relative with confirmed MEN 1 syndrome is sufficient to establish the diagnosis. The third diagnostic criterion involves genetic testing and the identification of a pathogenic mutation in the MEN1 gene [2].
Studies have shown that people with MEN 1 syndrome have a significantly lower life expectancy in comparison to the general population, with a difference of 15 years [3]. This stark contrast in life expectancy underscores the urgent need for effective diagnosis and treatment. The leading cause of death in patients with this syndrome is the expansion of malignant NETs, primarily pancreatoduodenal tumors [2]. Determining the tumors’ location and the extent of spread is crucial for selecting the appropriate therapeutic strategy [4]. Timely diagnosis of MEN 1 syndrome facilitates early detection of NETs, enables implementation of appropriate therapy, and consequently reduces morbidity [5].
This case involved a patient in whom the right choice of imaging studies enabled rapid diagnosis of MEN 1 syndrome and thus expedited the implementation of precise surgical treatment. This underscored the value of well-sequenced imaging in the diagnostic pathway.
A 45-year-old man was referred for the evaluation of a suspicious lesion in the pancreaticoduodenal region. The patient reported symptoms of gastroesophageal reflux and diarrhea, with up to twelve loose stools per day for approximately two years. In addition, he complained of periodic redness of the face and upper chest, which resolved spontaneously after an hour.
The diagnostic pathway began with a [18F]FDG PET/CT scan in March 2024. This [18F] FDG PET/CT study revealed several nodular lesions in the duodenal area of unknown character, with slightly increased marker uptake. To differentiate, an MRI was ordered based on suspected GIST. Additionally, there was unevenly increased uptake of [18F] FDG in the stomach, suggesting the coexistence of inflammatory and functional lesions.
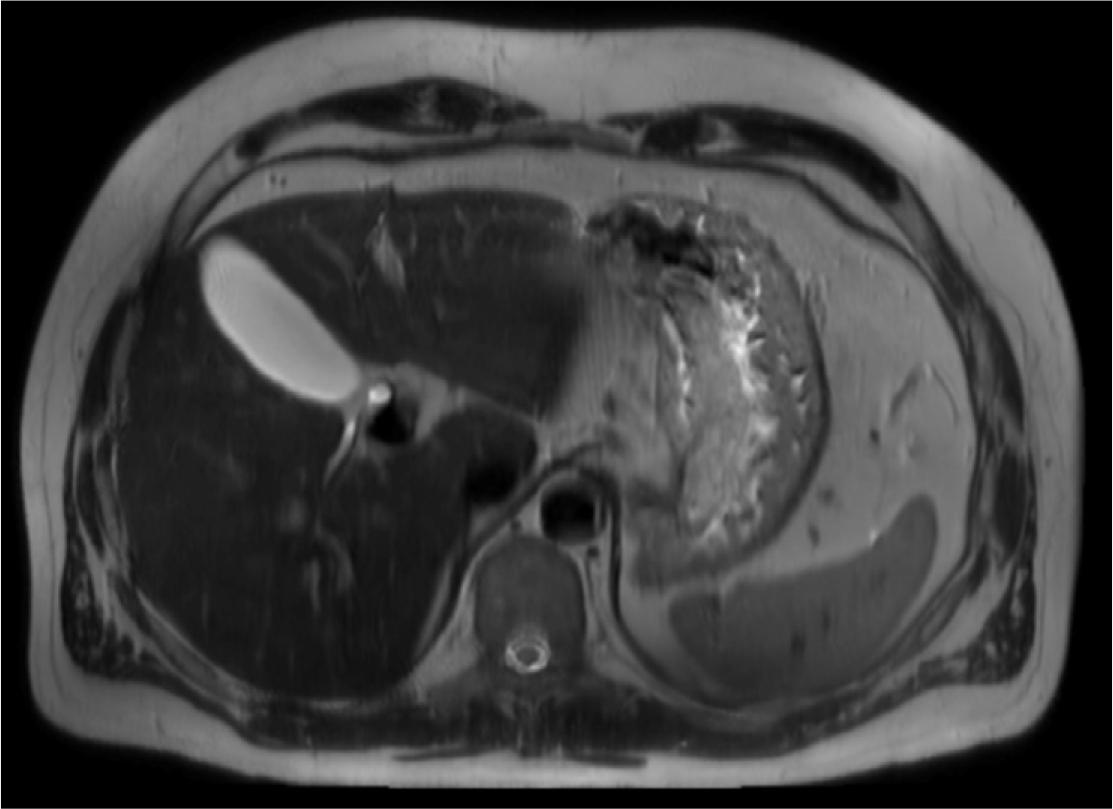
MRI, T2-weighted, axial view – Abdominal cross-sectional T2-weighted MR image demonstrates a large, thickened, edematous gastric wall along the lesser curvature, with preserved rugal folds. This image is atypical for gastric cancer and raises differential diagnoses such as lymphoma, hypertrophic gastritis, or Zollinger-Ellison syndrome.
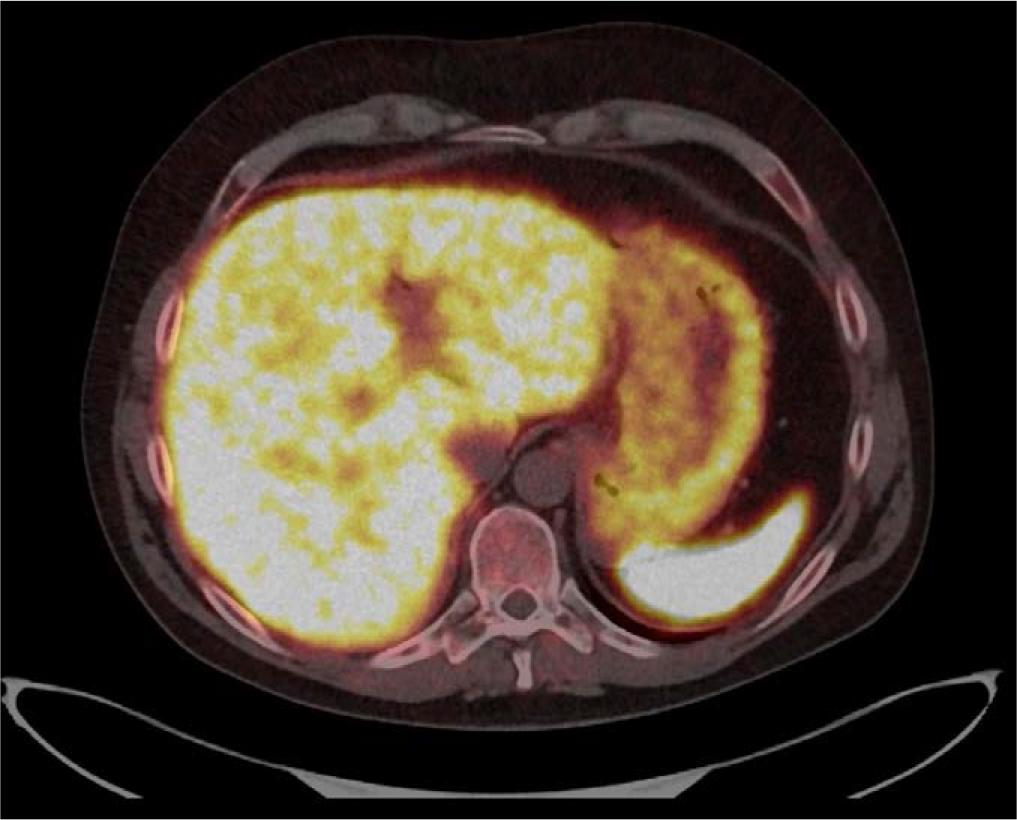
Axial fused [68Ga]Ga-DOTA-TATE PET/CT image at the level of the upper abdomen. Moderately increased radiotracer uptake is visible along the lesser curvature of the stomach near the cardiac orifice. This area corresponds to the gastric wall thickening visualized previously in the MRI, where a 106 × 34 mm lesion was seen. Although the uptake is not significantly intense, its location aligns with the previously identified abnormality. At the time of the MRI, differential diagnoses included gastric lymphoma, hypertrophic gastritis, and Zollinger-Ellison syndrome.
In August 2024, an abdominal MRI with MRCP was performed for further assessment. Two separate abnormalities were revealed. The first was a 106 × 34 mm abnormal widespread mass of thickened, edematous wall along the lesser curvature near the cardiac orifice of the stomach, with retained rugal folds. However, this image was not representative of typical gastric cancer infiltration. This image was nonspecific and required histopathological verification. Differential diagnoses included gastric lymphoma, hypertrophic gastritis, and Zollinger-Ellison syndrome.
The second finding was a solid, well-circumscribed lesion measuring 25 × 22 mm between the pancreas’ uncinate process and the transverse duodenum’s anterior wall. The image of the proliferative lesion was atypical for the classic form of pancreatic cancer. A neuroendocrine tumor was considered most likely, although a gastrointestinal stromal tumor (GIST) was also considered a possibility.

[68Ga]Ga-DOTA-TATE PET/CT, axial plane-Fused PET/CT axial image showing increased somatostatin receptor expression in a well-defined lesion localized between the duodenum and the uncinate process of the pancreas, later confirmed as a neuroendocrine neoplasm. Additional focal uptake is visible in regional lymph nodes, suggesting possible metastases.
Additionally, multiple enlarged lymph nodes were observed between the pancreatic head and duodenum and near the inferior mesenteric artery. These were all described as potential metastases.
In September 2024, the patient underwent somatostatin receptor scintigraphy with [99mTc] Tc-Tectrotide SPECT/CT, which confirmed pathologically high expression of somatostatin receptors (Krenning score 4) both in a nodule located between the lower part of the duodenum and uncinate process of the pancreas and within two regional lymph nodes, indicating a proliferative process in the area.
A supplementary endocrine workup was initiated to further evaluate the possibility of MEN 1 syndrome. In October 2024, [99mTc]MIBI scintigraphy of the thyroid and parathyroids showed a typically located thyroid gland with an even accumulation of radiolabel, with no apparent focal abnormalities of radiolabel uptake. However, it revealed increased accumulation of the radiotracer inferior and posterior to the lower pole of the right thyroid lobe, which suggested a hyperactive parathyroid. Two adjacent lesions were not able to be separated and thus properly assessed. These findings were ultimately considered indicative of parathyroid adenoma. Additional biochemical and hormonal tests were performed to confirm the diagnosis of primary hyperparathyroidism. They also revealed significantly elevated levels of chromogranin A, the most frequently used nonspecific marker for NENs [6].
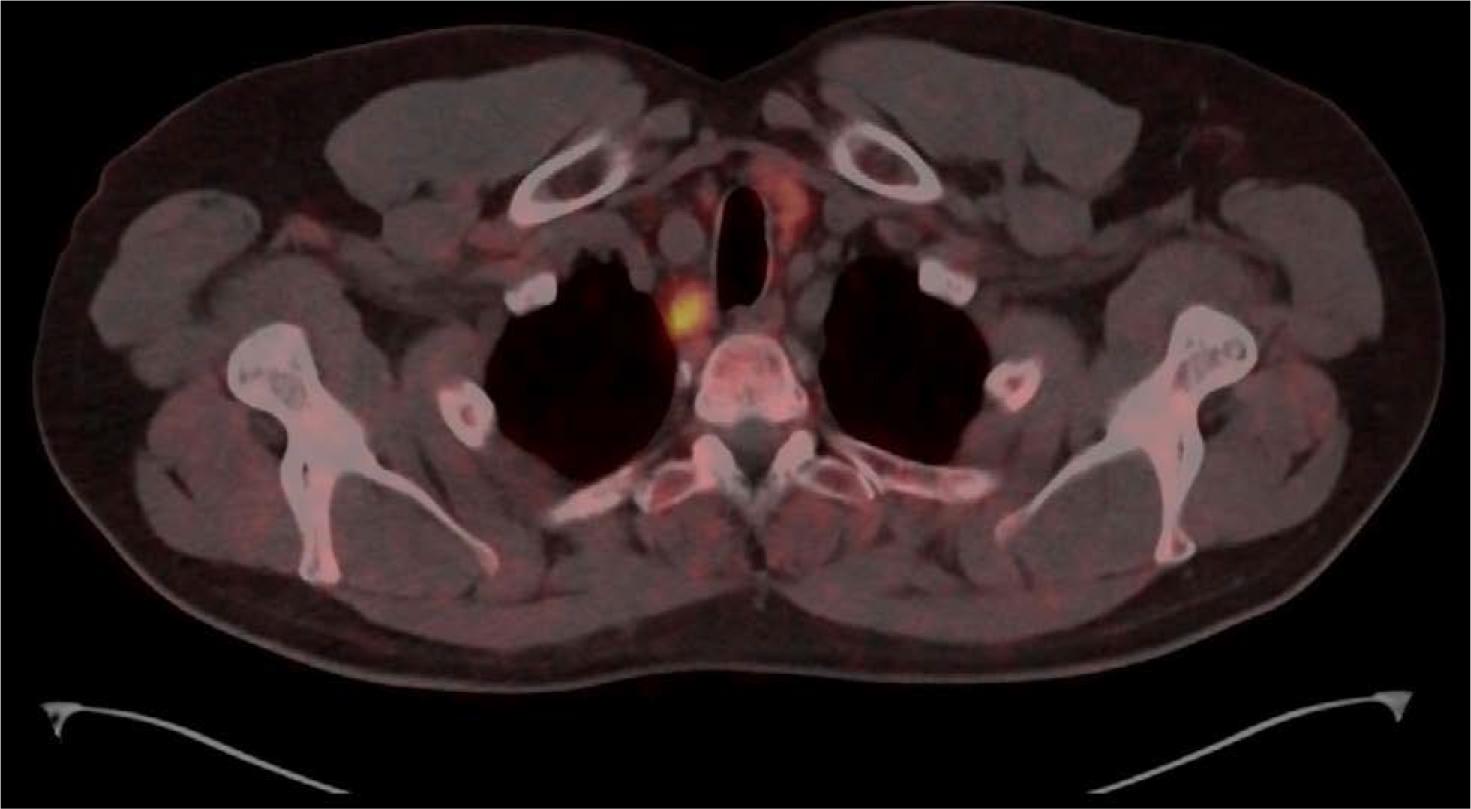
[68Ga]Ga-DOTA-TATE PET/CT, axial plane-increased focal uptake below the lower pole of the right thyroid lobe, which corresponds with a hyperactive parathyroid or parathyroid adenoma. Additionally, mild uptake was observed within two foci in the lower pole of the left thyroid lobe, which required further differentiation between an additional hyperactive parathyroid and a focal lesion in the thyroid.
Shortly after, [68Ga]Ga-DOTA-TATE PET/CT was performed. The scan ultimately confirmed increased somatostatin receptor expression in the previously visualized pancreaticoduodenal lesions, specifically in the pancreas, near the head of the pancreas, and tangentially to the wall in the duodenum, which was consistent with a previously suspected neuroendocrine tumor. In soft tissues, increased expression of somatostatin receptors was visualized in the form of a hyperactive parathyroid located inferiorly and dorsally from the lower pole of the right thyroid lobe and within two foci in the area of the lower pole of the left thyroid lobe, which required further assessment to differentiate between a hyperactive parathyroid and focal lesion in the thyroid.
In addition, mild uptake was noted in the pituitary gland, which raised the suspicion of a macroadenoma.
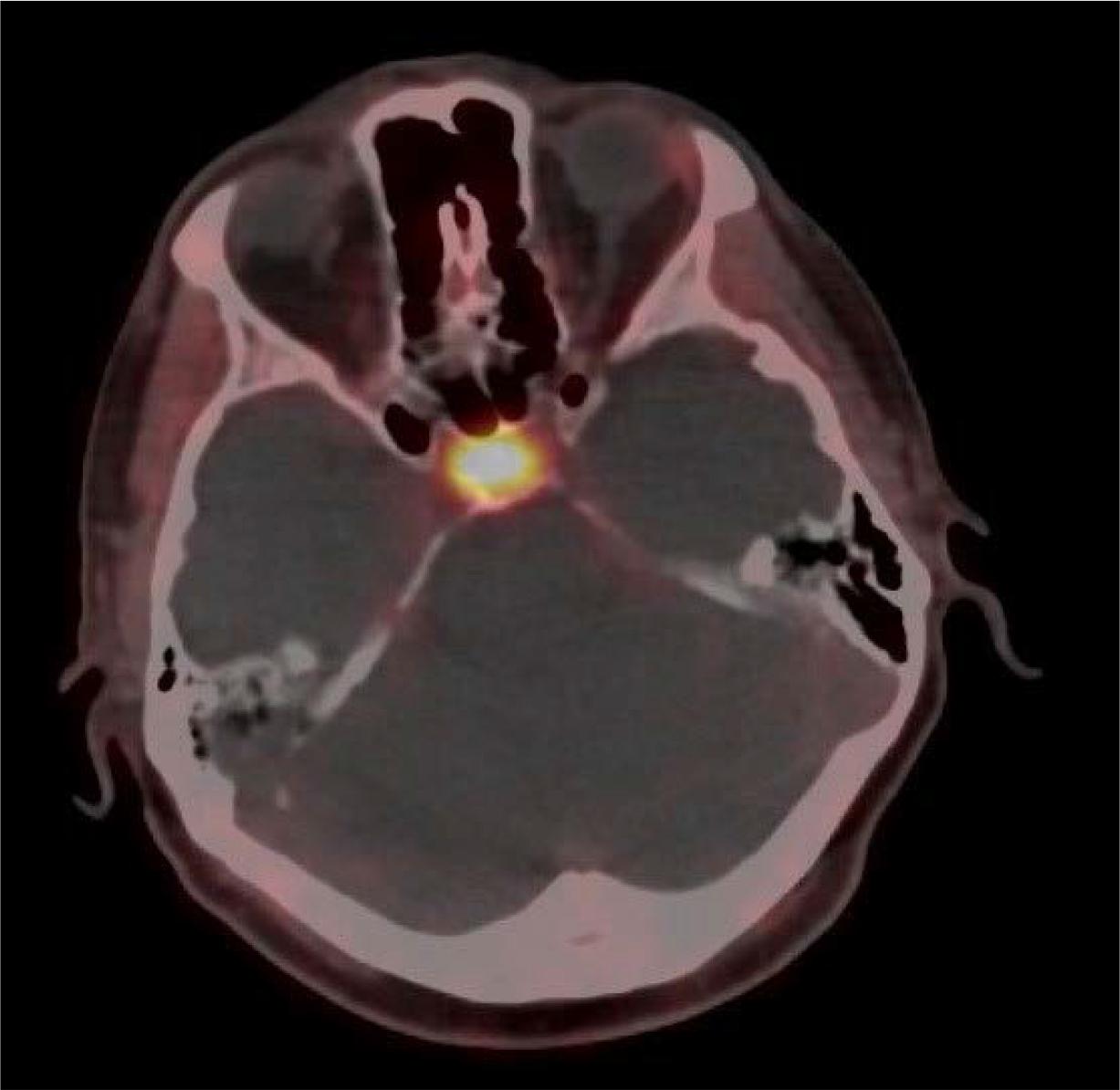
[68Ga]Ga-DOTA-TATE PET/CT, axial plane-increased uptake in the pituitary gland, correlating with MRI findings of a suspected macroadenoma, in line with MEN 1 syndrome.
Based on the results of [68Ga]Ga-DOTA-TATE PET/CT, the patient was referred for total pancreatectomy, splenectomy, and subtotal gastrectomy performed in November 2024.
Histopathological analysis confirmed the diagnosis of a well-differentiated neuroendocrine neoplasm of the pancreatic duodenal region, with a Ki-67 index of 1-2%.
Postoperatively, the patient required insulin therapy, treatment of newly diagnosed hypertension, and further evaluation of a previously suspected pituitary macroadenoma.
Laboratory tests revealed a substantially elevated PTH level of 129,0 pg/ml [reference range: 15,0-65,0 pg/ml]. The total serum calcium level was mildly elevated at 11,4 mg/dl [reference range: 8,6-10,2 mg/dl], suggesting primary hyperparathyroidism as a clinically diagnosed MEN 1 syndrome component.
Diagnosing neuroendocrine neoplasms requires a multimodal approach, incorporating advanced imaging techniques, specific biochemical markers, and histopathological confirmation [6].
Current guidelines suggest that „(…) in the imaging diagnostics of NETs, the most sensitive method is with the use of radiolabelled somatostatin analogues” [6].
This paper focused primarily on the application of Somatostatin Receptor Imaging (SRI) using [68Ga]Ga-DOTA-TATE PET/CT to confirm the diagnosis of neuroendocrine neoplasms (NENs) and facilitate optimal surgical management.
The [68Ga]Ga-DOTA-TATE PET/CT scan played a pivotal role in the diagnostic process, confirming the presence of a pancreatic NET with suspected lymph node metastases, underscoring its status as the recommended method of imaging in the diagnostic algorithms for NETs (excluding adrenal pheochromocytoma)[6]. Additionally, it made it possible to visualize lesions resembling parathyroid adenomas, which were excised accurately.
This case exemplified how carefully selected advanced imaging technique could provide a detailed picture of the nature and extent of endocrine tumors in Multiple Endocrine Neoplasia type 1 Syndrome.
Due to the unavailability of image data from other imaging studies ([18F]FDG PET/CT, SPECT/CT, etc.), all figures in this article are derived from the [68Ga]Ga-DOTA-TATE PET/CT and MRI. They serve as illustrative material representing findings also described in other imaging examinations.