The pancreas plays an important role in the normal exocrine function of the GI tract and contributes to the human’s endocrine well‑being via release of specific hormones. Unfortunately, the pancreas is also host to a wide variety of neoplastic and non‑neoplastic disorders. Developmental anomalies, acute and chronic inflammation, and a vast array of solid and cystic pancreatic tumors are some of the entities that may involve the pancreas. Although it is well known that imaging plays a pivotal role in the detection and characterization of pancreatic diseases, many technical, perceptional, and knowledge‑based pitfalls may be encountered during the interpretation of pancreatic imaging studies. Therefore, in this presentation, I am to highlight some of the pearls and perils the radiologist should be aware of.
Mimics of pancreatic diseases are usually caused by developmental variants and anomalies [1]. They are very commonly encountered in clinical practice, and the key is to differentiate these “non‑touch” entities from true pancreatic conditions. Familiarity with the different groups of normal variants, such as aberrant ductal configurations, gland size and width variations, pseudomasses (fetal lobulations), and intrapancreatic ectopic tissue will undoubtedly improve diagnostic capabilities.
The reason radiologists miscall (misdiagnose) pancreatic abnormalities is generally multifactorial and may be induced by lack of knowledge, inadequate technique, or inaccurate interpretation. Probably, the most challenging task is to accurately differentiate pancreatic ductal adenocarcinoma (PDAC) from less ominous pancreatic conditions, such as uneven lipomatosis, focal autoimmune pancreatitis, and other inflammatory pseudomasses (Figures 1 and 2) [2–4]. Moreover, accurate determination of PDAC (un)‑resectability, extremely important for each individual patient, may prove to be a difficult task in the absence of knowledge of recent guidelines and subtle methods of spread. Finally, especially because of their marked incidence on cross‑sectional imaging studies, inaccurate characterization of focal cystic pancreatic lesions (FCPL) may lead to inadvertent management. Familiarity with the key imaging differentiating features of those lesions is therefore essential [5].
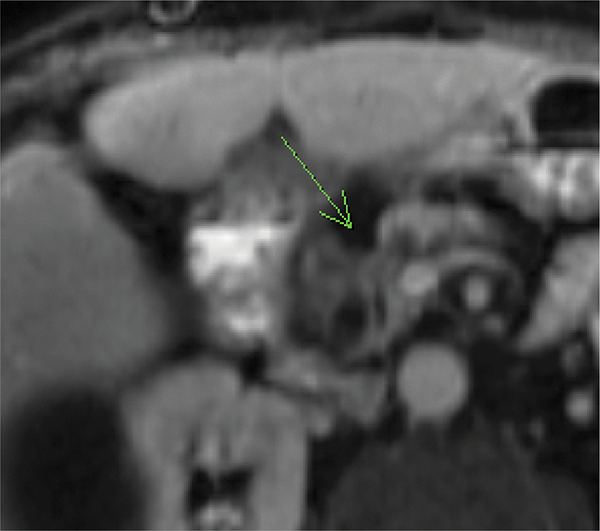
Figure 1
Axial fat‑suppressed contrast‑enhanced T1‑WI shows an ill‑defined hypovascular pancreatic head mass (arrow) with dilatation of the CBD and pancreatic duct. The suspected diagnosis was PDAC.

Figure 2
Coronal oblique thick‑slab MRCP image shows 2 MRCP signs that suggest the mass may be inflammatory in nature rather than neoplastic: (a) the “duct penetrating sign” (the pancreatic duct runs through the mass and is not interrupted), and (b) the “attraction sign” (the common bile duct is bent at a 90° angle and attracted to the mass). The final diagnosis was indeed inflammatory pseudomass.
Generally, true misses in imaging can be classified as perceptual (the lesion is there but we don’t see it), technical (the lesion is there but technical errors render it invisible), or communication related (the lesion is detected but not reported). In the pancreas, the most common misses include: failed detection of small (resectable) PDAC or malignant intraductal pancreatic mucinous neoplasm (IPMN); failed detection of hypervascular pancreatic neoplasms [6]; failed detection of early chronic pancreatitis [7]; and failed detection of vascular complications in acute pancreatitis.
In conclusion, pancreatic pitfalls are everywhere, also in your practice! Therefore, familiarity with the many perils that may negate an inaccurate diagnosis, and specific pearls may that lead you to the correct diagnosis, is of utmost importance. Finally, as a radiologist, always be aware what a suboptimal technique, an inadequate approach, lack of knowledge and missing subtle findings may mean for your patients with pancreatic abnormalities.
Competing Interests
The author has no competing interests to declare.
