Introduction
Hospital avoidance programs are growing in popularity worldwide and although the nature of these programs vary greatly, they frequently place an emphasis on primary care enhancements, particular for groups at high-risk of acute deterioration. Technical developments in communication and paradigm shifts with respect to patient centred care encourages hospital avoidance programmes to be multidisciplinary and span multiple modalities including face-to-face, hospital-at-home and telemedicine [1]. Despite their popularity, these programs have had varying success [23].
In Australia, there have been several federal and state government integrated care strategies with similarly mixed levels of success in reducing hospital utilisation. Recent examples include the federal Diabetes Care Project [4], Health Care Homes trial [56], the Australian Gold Coast Integrated Care programme [7] and the New South Wales (NSW) Chronic Disease Management program [8]. A recent systematic review of 14 studies of hospital avoidance programs found that resource availability, compatibility and fit of the innovation and engagement of interprofessional teams were the strongest determinants of successful implementation [1].
Australian healthcare providers report high levels of demand over the winter period both in hospitals and community settings with both infants and the elderly at particularly heightened risk [9]. Traditionally, hospitals plan for a surge in demand by reducing elective admissions and opening additional beds [10]. In parallel with increasing acute care capacity in the hospital sector, there is a need for greater investment in primary care sector capacity and integration between the two. Despite universal health coverage, Australia experiences substantial fragmentation between primary care and the specialist and hospital sectors. This is particularly a problem for people with chronic and complex care needs. The “Winter Strategy” was an integrated care model designed to more effectively address the needs of patients with chronic and complex conditions in the northern region of NSW, Australia. It sought to address health system fragmentation by bringing together support services from both primary care and hospital sectors which are funded through different sources in Australia’s federal system. Specific aims of the program were to: (1) support general practices to reduce the likelihood of their highest risk patients from being hospitalised and to keep these patients well in winter; and (2) for those who are admitted to hospital to reduce the length of stay in hospital and re-admission rates through improved processes for integration and collaboration of care between hospital, community and primary care during the winter months.
In this paper we present an evaluation of the Winter Strategy in its first 2 years of implementation (2017 and 2018) with follow up from 2017–2020, focussing on both implementation and impact outcomes. Evaluation aims include: (1) evaluation of the implementation of the Winter Strategy program; (2) assessment of both participant and practitioner experiences before and after the Winter Strategy; and (3) change in hospital utilisation and emergency presentation rates from enrolment to 12 months after program participation.
Methods
Setting
The northern NSW region covers over 20,732 km2 and around 290,271 (2016 Census) people and there are pockets of high socioeconomic disadvantage particularly in the more rural and remote areas. It has an ageing population with over 20% over 65 years compared with 15.7% for the Australian population and by 2036 it is projected to exceed 30% [11]. Chronic health conditions are the leading cause of illness, disability and death in the North Coast region. Over 62% of adults reported having a long-term health condition, nearly 13% higher than the overall rate reported nation wide rate [12].
Population/patient selection
Enrolment occurred over two periods coinciding to the winter months of 2017 and 2018. Both cohorts were followed up until December 2019. Eligible patients were adult general practice patients (18 years or over) with chronic and/or complex health problems who were thought likely to benefit from a focus on proactive care and monitoring including: optimised self-management; improved access to necessary support services; and improved collaboration with community and hospital services. Patient selection was based on perceived need and likelihood of benefit by the treating general practitioner. Patients were ineligible for the program if they were enrolled in a coordinated veteran’s care program or palliative care programs.
Practices were offered a number of guiding notes and tools that they could use to help refine their patient selection. This included the HARP risk assessment tool [13] and tips for using patient database queries to identify patients at high risk of hospitalisation. In addition to these tools, general practice teams were asked to use their overall knowledge of their patients to select those most likely to benefit from the program. Co-design workshops indicated the clinician led selection process was important for clinician engagement.
Co-design of the strategy
The Winter Strategy was a collaboration between the NSW state government funded Northern NSW Local Health District (NNSWLHD), the federal government funded Primary Health Network known as Healthy North Coast, and private general practices. It sought to support change at multiple levels, including shared governance across lead organisations, financing of clinical care, cross sector collaborations, clinical team building, improving scope and quality of clinician’s roles and patient activation and agency.
The co-design involved a workshop in early 2017 and again in 2018 to determine the project’s aims and objectives. In 2017, workshops were convened comprising over 50 stakeholders including consumers and representatives from NNSWLHD, Healthy North Coast, General Practice staff, Aboriginal Community Controlled Health Services and ambulance services. From these workshops, strategies and interventions were identified and then prioritised to constitute the core components of the program. Details were then refined by combined working parties. In 2018, learnings from the 2017 implementation were drawn on, and another co-design review workshop was held in early 2018 with health professionals from NNSWLHD and the primary care sector for ongoing refinements to the program.
Strategy components
The main components of the program logic included:
Winter watch lists in which specific patients were targeted for self-care promotion, sick day action plans (patient-initiated management and treatment) and regular follow up by general practice teams.
Automated admission and discharge notifications to the general practitioner; and
A chronic disease management service (nursing, allied health assistance, access to a care facilitator and health coaching) provided by the local health district in collaboration with the general practitioner.
General practices were provided a practice facilitation guide and checklists in the preparation phase. All participating teams were remunerated to cover additional practice nurse time needed to deliver additional care and undertake program preparation not funded through Medicare. NNSW LHD Chronic Disease Management Nurses were encouraged to meet face to face with general practice teams in their area. In most general practice teams, a nurse and practice manager were nominated as the team leads. Step by step implementation suggestions were provided for each phase of the program. Support from the executive of the NNSWLHD ensured the hospital IT systems were modified to support automated notification of the GP when a Winter Strategy patient entered the hospital and automated notification to the Chronic Disease Management team when the hospital presented to Emergency and/or was admitted to hospital.
Outcomes
Outcomes focussed on the quadruple aim of improved patient experience, clinician experience, health outcomes and cost efficiency [1415].
Patient experience – Winter Strategy patients were asked questions across six domains (access, timeliness, care coordination, comprehensive care, self-management confidence and patient activation). Surveys were provided to patients by the general practices prior to commencing the Winter Strategy and at the end of the program. The pre-survey included 13 questions. The follow up survey was modified based on responses at baseline. Questions with very high overall scores were removed as they were not considered sensitive to change and new questions were added. The final survey administered contained 15 questions, eight of which were common to the baseline survey (see supplementary material for the two survey tools). The eight paired questions were used for reporting program impact.
Clinician experience – Surveys were administered to participating health professionals assessing their level of satisfaction in caring for chronic/complex patients, collaboration across public and private provider groups, general practitioner involvement in admission/in-patient progress and hospital discharge processes, being able to arrange appropriate services for patients, and feeling confident their patients receive good care.
Health outcomes and cost efficiency – A retrospectively created control group was developed and matched on past hospital data to examine the impact of the Winter Strategy on hospitalisation usage, including emergency presentations, and hospital related costs. Outcomes of interest included the change in the rate of potentially preventable hospitalisations [16] (Supplementary Table 1) before and 12 months after implementation of the Winter Strategy, all cause hospital admissions, emergency department presentations and length of hospital stay. Cost efficiency was assessed using hospitalisation related National Weighted Activity Units (NWAUs) – a measure of the relative complexity and treatment costs for each patient separation (admitted), presentation (emergency department) or encounter (outpatient). Potentially preventable hospitalisations relate to vaccine-preventable, chronic and acute conditions with further definitions available in the supplementary material. Potentially preventable hospitalisations is a list constructed according to the Australian Institute of Health and Welfare, National healthcare agreement. Although other validated measures exist in the international literature, the national standard definitions were used in this study for comparison with other nationwide initiatives.
Data sources
Patient registration data was collected when a patient entered the program. This data included demographic and comorbidity information, health care status, the presence of chronic and/or mental health conditions and the number of medications currently prescribed. Analysis of hospitalisation patterns over time was performed using routinely collected and registry data available from the local health district. This data included: (i) the admitted patient data collection (APDC) which covers hospital service utilisation information covering dates, diagnosis, procedures and length of stay; (ii) the emergency department data collection (EDDC) which covers patient presentation information including date and time of arrival, means of arrival, triage category, emergency category and major diagnosis and; (iii) Non-admitted patient data (NAP) including service type and date received which encompasses hospital outpatient clinics, community based clinician and in home services. All data sources were linked to the patient registration data. In hospital deaths were identified using the APDC data.
Matched cohort
Propensity score matching [17] was used to obtain a matched control for a comparison between those who received the intervention with a similar group of patients not receiving the program. Multivariable logistic regression was used to create the propensity model for program participation. The models included demographic and clinical variables as well as service utilisation rates preceding the period of exposure. Matching was performed in a one-to-two ratio with the intervention group matched to two control participants. A greedy matching algorithm of nearest neighbour was used to select the intervention/control pair that minimised the logit of the propensity score. Matching was performed without replacement and with exact matching for categorical values indicating the frequency of potentially preventable hospitalisations and unplanned hospitalisations (0, 1 or 2+ hospitalisations) in the 3 months, 3 to 6 months and 6 to 12 months leading up to the intervention.
Statistical analysis
Paired before and after patient experience and clinician surveys were analysed using Wilcoxon Signed Rank test. Question responses including “don’t know” and “not applicable” were removed from the analysis. Difference in difference analysis was performed to assess hospital utilisation changes over time and were presented as rates per 100 people per month. Longitudinal analysis of hospital utilisation was conducted between 2013 and 2019, incorporating a 5-year look back period from the initial 2017 program. Curves associated with rates and means were smoothed using locally estimated scatterplot smoothing regression [18]. Standard deviations and proportions were calculated where appropriate.
Health and cost efficiency outcomes were assessed as an average over the first 12 months after baseline enrolment date. For participants in the 2017 Winter Strategy program a further 24 month comparison between baseline and 24 months was assessed to understand further longitudinal trends.
Visualisation of the hospitalisation trends was used to assess the assumption of parallel trends in the time preceding the intervention. This assumption is required for a difference-in-difference analysis. A Generalised Estimating Equation (GEE) negative binomial regression model was used for the difference-in-difference model clustered by person and was adjusted by sex, marital status, year of birth and SEIFA assuming a compound symmetry correlation structure. Regression modelling was performed in SAS version 9.4 with curve sketching in R [19] using dplyr [20], tidyverse [21], gridExtra [22].
Ethics
The study was approved by the North Coast NSW Human Research Ethics Committee (2018/ETH00360).
Results
Implementation
Sick day action plans
In qualitative interviews (September 2018), most practices (80%) said they were using the provided templates to implement sick day action plans. In particular, the asthma, COPD, heart failure and chest pain plans were popular. The chronic kidney disease plan needed further explanation and the diabetes plans were not considered helpful. Barriers to adoption included: (i) size of the print for patients with low vision; and (ii) complexity for patients with low health and general literacy. Simple pictorial plans with basic instructions were considered more useful.
Admission discharge notification
Practice staff were asked whether admission discharge notifications (ADNs) were being received and whether they were useful. Staff from all 16 practices responded (majority practice nurses) and of these eight said they received the ADNs and of those seven said they were useful. Seven practices said they were either not receiving them or were not aware of receiving them.
Multidisciplinary care
In 2017, 30 general practices registered to participate with 24 practices participating in the entire program and six practices withdrawing from the program as it progressed. Reasons for withdrawal in 2017 were mainly related to short preparation and implementation time frames creating unacceptable distraction in the practice, insufficient time to make changes to practice systems, increased burden associated with employing additional nursing staff to engage with and register patients. In 2018, 24 general practices participated (9 of these continuing from 2017) and there were no withdrawals from the program.
Nurse training and support – A total of 28 nurses from eleven 2018 practices attended health coaching training. Region-wide nurse network meetings were held and included topics such as health literacy, wound management, use of Sick Day Action Plans for chronic conditions, Older Persons’ Health Assessments and how to access My Aged Care. Presentations were provided by NNSWLHD and Healthy North Coast staff with specialised knowledge in their fields.
Use of allied health and practice nurse services – Supplementary allied health funding was used more frequently in 2018 than in 2017 but uptake was low overall. Only six practices requested funding for these services. A total of 57 sessions of allied health were provided at a total cost of $5411. The majority of these sessions were physiotherapy to address pain and mobility issues. One practice used funding to establish a cardiopulmonary group employing an exercise physiologist, diabetes educator, dietician, and social worker to run group sessions. Only two practices requested reimbursement for Practice Nurse home visits.
Remuneration to general practices – Payments to general practice aimed to cover the additional work of preparing their team roles and providing care not covered by Medicare. In 2017 this was $225.70 per enrolled patient which equates to approximately 6 hours of practice nurse time. In 2018 the payments were slightly more ($287 per patient) and divided into payments for planning, enrolling and service delivery phases to encourage timely practice team preparation.
Learnings between 2017 and 2018 implementation – The co-design approach was able to integrate feedback and experience from the 2017 implementation experience to guide refinements for the 2018 implementations. Greater support was provided to clinicians in identifying potential participants. Compared to 2017 where there were attempts to use risk stratification tools and more systemised criteria for eligibility, in 2018 GPs were allowed wider discretion in selection of patients in 2018. Changes were also made in the way program information was provided and the lead-time given to practices prior to the intervention.
Participant characteristics
In total the Winter Strategy serviced 1244 patients. The 2017 Winter Strategy (WS17) program included 650 participants with data from 24 GP practices. Registration took place between 31st May 2017 and 6th August 2017. The 2018 Winter Strategy (WS18) program included 786 patients from 24 practices where registration lasted from 1st April 2018 to 8th June 2018. A total of 192 patients participated in the program in both 2017 and 2018.
Demographic characteristics were obtained at registration (Table 1). For the 192 people participating in both years, the data obtained at their initial registration is included. Overall, there were some notable differences in characteristics between the three samples, particularly in terms of comorbid conditions and demographic characteristics (higher proportion with disability or aged pension in 2018 vs 2017). Further, sick day action plans were more heavily promoted in 2018 which is reflected in the higher uptake observed in that year.
Table 1
Participant characteristics.
| CHARACTERISTICS | WINTER COHORT 2017 (N = 458) | WINTER COHORT 2018 (N = 594) | BOTH WINTER 2017 & 2018 (N = 192)1 | ALL PARTICIPANTS (N = 1244) |
|---|---|---|---|---|
| Age – Mean (SD) | 74.9 (13.18) | 73.9 (11.60) | 76.0 (12.15) | 74.6 (12.30) |
| Sex (% Female) | 255 (55.7%) | 339 (57.1%) | 101 (52.6%) | 695 (55.9%) |
| Current Smoker | 46 (10.0%) | 27 (4.5%) | 14 (7.3%) | 87 (7.0%) |
| Disability or aged pension | 233 (50.9%) | 459 (77.3%) | 105 (54.7%) | 797 (64.1%) |
| Health card holder | 38 (8.3%) | 90 (15.2%) | 29 (15.1%) | 157 (12.6%) |
| Comorbidities | ||||
| Congestive Cardiac Failure | 71 (15.5%) | 44 (7.4%) | 29 (15.1%) | 144 (11.6%) |
| COPD3 | 152 (33.2%) | 154 (25.9%) | 94 (49.0%) | 400 (32.2%) |
| Ischemic Heart Disease | 169 (36.9%) | 104 (17.5%) | 60 (31.3%) | 333 (26.8%) |
| Diabetes | 156 (34.1%) | 140 (23.6%) | 62 (32.3%) | 358 (28.8%) |
| Chronic Kidney Disease | 51 (11.1%) | 54 (9.1%) | 37 (19.3%) | 142 (11.4%) |
| Asthma | 98 (21.4%) | 133 (22.4%) | 42 (21.9%) | 273 (21.9%) |
| Number of Comorbidities | ||||
| No comorbidities | 92 (20.1%) | 3 (0.5%) | 37 (19.3%) | 132 (10.6%) |
| 1 comorbidity | 267 (58.3%) | 299 (50.3%) | 102 (53.1%) | 668 (53.7%) |
| 2 comorbidities | 87 (19.0%) | 223 (37.5%) | 45 (23.4%) | 355 (28.5%) |
| 3 or more comorbidities | 12 (2.6%) | 69 (11.6%) | 8 (4.2%) | 89 (7.2%) |
| Mental Health | ||||
| Depression or anxiety | 114 (24.9%) | 142 (23.9%) | 40 (20.8%) | 296 (23.8%) |
| Active alcohol and/or other drug use issues | 15 (3.3%) | 12 (2.0%) | 2 (1.0%) | 29 (2.3%) |
| Other mental health conditions | 38 (8.3%) | 27 (4.5%) | 7 (3.6%) | 72 (5.8%) |
| Other | ||||
| Medications – Prescribed more than 5 medications | 333 (72.7%) | 439 (73.9%) | 130 (67.7%) | 902 (72.5%) |
| Care Plan – Reviewed in the last 6 months | 298 (65.1%) | 461 (77.6%) | 165 (85.9%)2 | 892 (71.7%) |
| Sick day action plan | 47 (10.3%) | 178 (30.0%) | 43 (22.4%)2 | 242 (19.5%) |
[i] Notes:
1. Baseline demographic characteristics taken from 2017 enrolment information.
2. Care plans and sick day plan statistics taken from 2018 enrolment information for this cohort.
3. Chronic Obstructive Pulmonary Disease.
Patient Experience
Survey results were only available for participants in WS18 program. Pre- and post-surveys were available for 608 (77.3% response rate) (Figure 1). Paired analysis of eight common questions indicated that there were statistically significant improvements for all questions except “I understood how each person in my healthcare team could help me”.
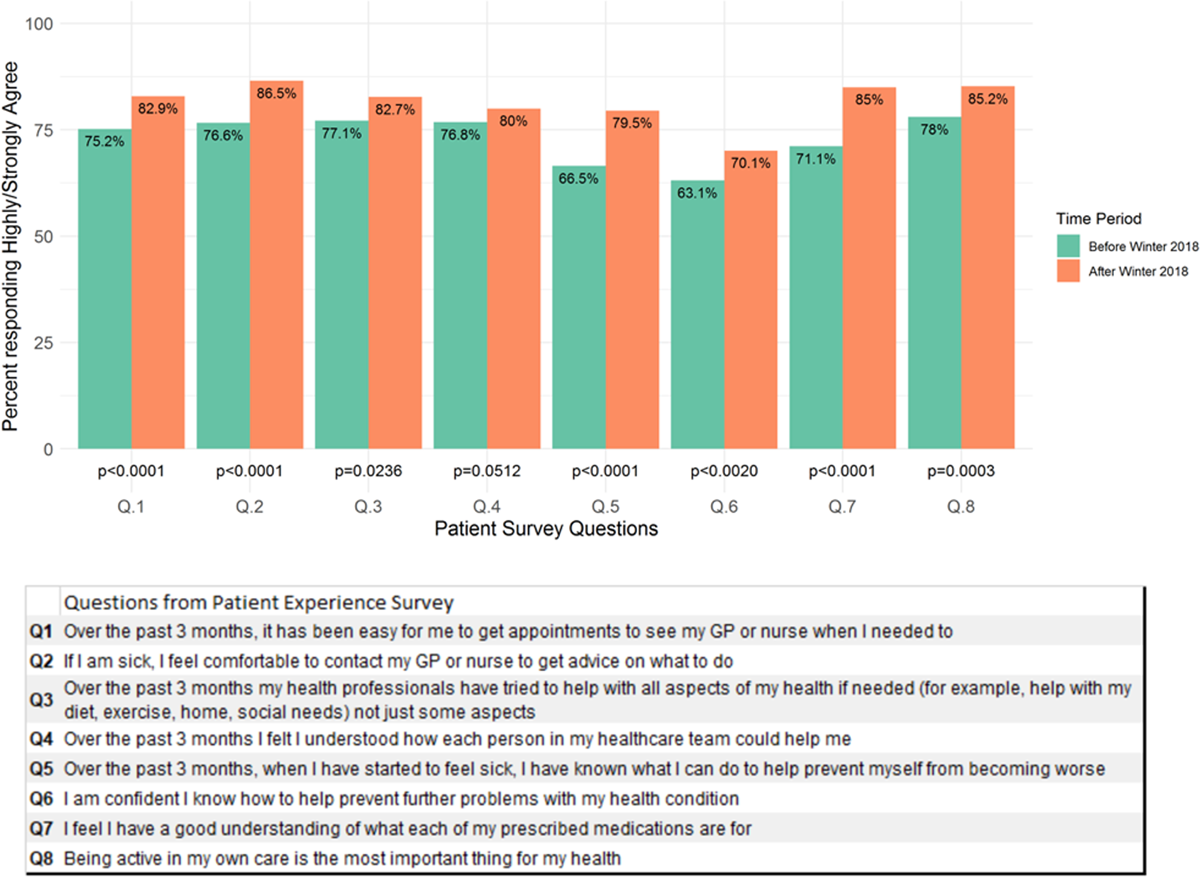
Figure 1
Patient experience survey responses (n = 608) before and after participation in the Winter Strategy in 2018.
In the post-survey 68.7% reported that appointment access to their GP team had improved and 69.8% felt more comfortable to seek advice from their general practice team. Self-management increased with 90.6% reporting having a sick day action plan, and 61.4 % reporting they had used it. In total 71.3%, reported improvement in their health care team trying to help with all aspects of their health needs and 73% felt their understanding of how each person in their health care team could help them had improved. There was no difference between sexes for those responding ‘highly/strongly agree’ to any of the questions in either the pre-surveys or post-surveys.
Clinician Experience
Although the exact number of participating clinicians is difficult to ascertain due to staff turnover and variable participation at each practice, it is estimated that a total of 159 primary care health professionals participated in the program (93 GPs, 47 Practice Nurses and 19 Practice Managers). Clinician experience surveys were sent to these health professionals prior to the intervention and again at its conclusion. The pre-intervention survey was completed by 131 staff (82% response rate), and 123 staff (77% response rate) completed the post-survey with 78 staff (49%) completing both pre and post surveys. The health professional mix of respondents was broadly representative of the eligible sample – 65% and 61% of responders for the pre and post survey respectively were GPs, 31% and 35% respectively were practice nurses, with unknown health professional comprising the remainder.
Paired clinician experience survey data showed improvements for all questions covering general practice and hospital communication and collaboration – 79% considered sick day action plans safe and effective, and 75% reported that WS18 triggered more thorough and systematic care planning than they were usually able to provide to their patients (Figure 2).
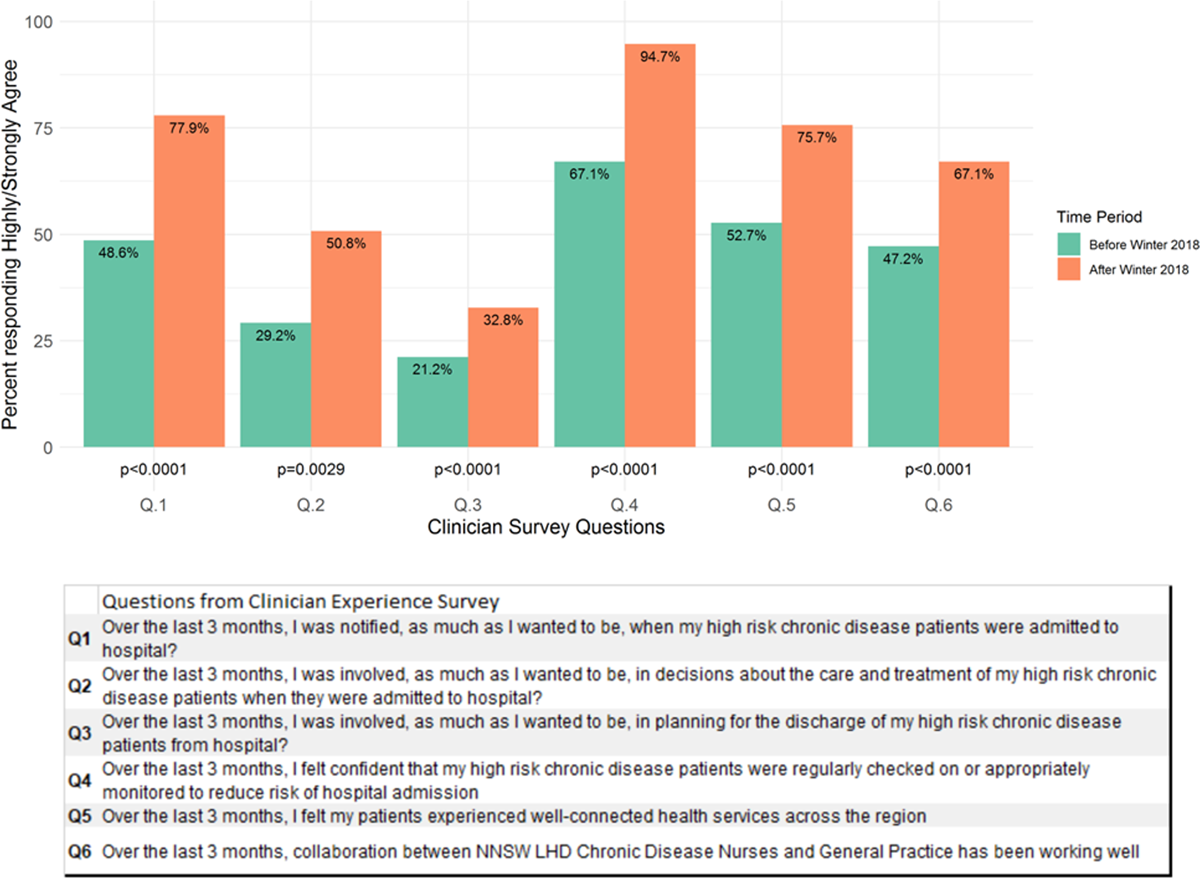
Figure 2
Clinician experience responses (n = 78) before and after participating in the Winter Strategy in 2018.
Hospital utilisation outcomes
The 1244 Winter Strategy cohort were frequent users of the NSW health services in the 5 years prior to program participation. Over the period of available data, 94% of this group of people had at least one entry in the NSW health administrative datasets and 63% of participants had an entry in all three datasets (Figure 3). Hospital utilisation statistics indicate that participants in the program were at high risk of hospitalisation with over 40% being admitted to hospital in the 12 months prior to participation and over 40% presenting at an ED. In each of the cohorts the proportion of unplanned hospitalisations far exceeded the number of planned admissions.
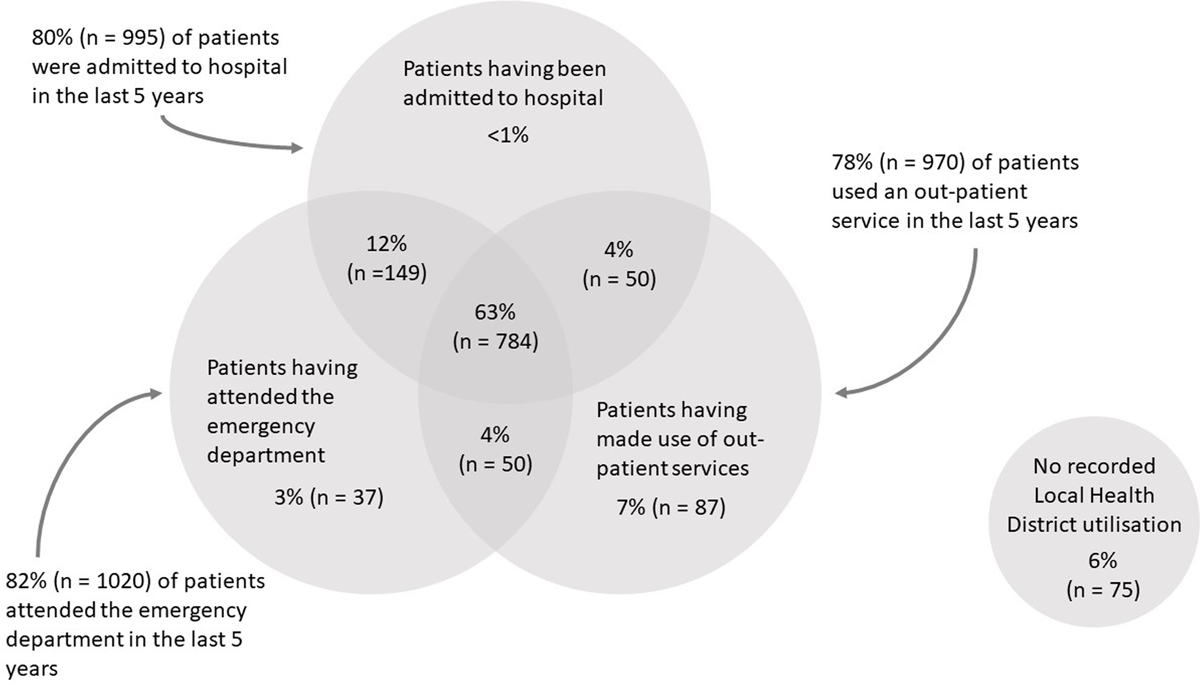
Figure 3
Winter Strategy participants’ use of health services within 5 years prior to enrolment (n = 1244).
Demographics and historical health service utilisation were used to identify the comparison cohort. Variables included sex, marital status, year of birth, a measure of social advantage, number of avoidable hospitalisations in the time leading up to the intervention, emergency presentations in the previous 12 months including semi-urgent and non-urgent presentations. The matching restrictions reduced the size of the winter sample to 1163 due to exclusion of extreme cases (n = 6) and those without any record in any NSW health administrative datasets (n = 75, 6% – Figure 3). Remaining participants were matched to 2319 controls. Supplementary Figure 1 provides details of the standardised mean difference (SMD) between controls and winter participants for the covariates used for analysis both before and after matching.
The rate of potentially preventable hospitalisations per 100 people per month for the Winter and the comparison cohort varied over time (Figure 4). The pre-intervention data showed reasonable evidence of parallel trends between the two groups, however in the interval between 2 years to 12 months pre-intervention, the utilisation rates for the comparison cohort were markedly lower. In the 12 months pre-utilisation there was a bi-modal peak in utilisation at 12 months prior to the intervention and then again at the time of the intervention in both cohorts, however it is more pronounced in the Winter Strategy cohort. After the intervention there was a decrease in the hospitalisation rates in both groups.
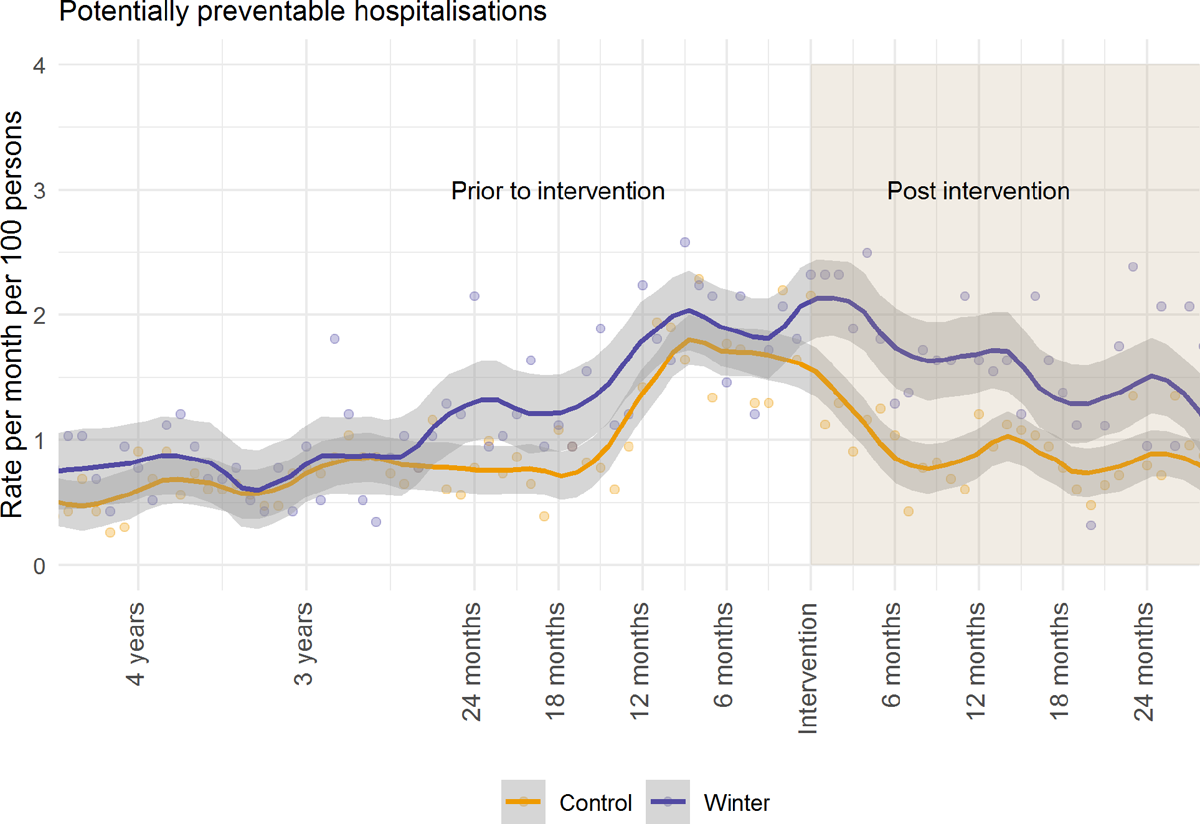
Figure 4
Potentially preventable hospitalisation rate (per 100 people per month) before and after the intervention, for all Winter Strategy participants.
Supplementary Figure 2 provides a breakdown of potentially preventable hospitalisations by ICD code. It demonstrates a greater number of respiratory-related codes both before and after intervention in the Winter Strategy cohort relative to the comparison cohort.
Table 2 provides the adjusted difference in difference analysis between the Winter and comparison cohorts in the 12 months pre and post intervention period for all utilisation measures. Potentially preventable bed days and low urgency emergency department presentations had similar declines in utilisation for both cohorts. The magnitude of decline was greater in the comparison cohort for all cause hospitalisations, unplanned hospitalisations, potentially preventable hospitalisations, emergency use and total NWAU when compared with the Winter cohort. Although all hospitalisations decreased at a greater rate for the comparison cohort compared to the Winter Strategy cohort, the main driver for this difference was related to the reduction in unplanned hospitalisation (Comparison Cohort: –31.1 95% CI –31.51 to –30.60, Winter Strategy Cohort –4.6 95% CI –4.64 to –4.58).
Table 2
Hospitalisation utilisation rate per 100 people per month between Winter and comparison cohorts.
| OUTCOME (RATE PER 100 PEOPLE) | MEAN DIFFERENCE (PRE-POST INTERVENTION) 95% CI | ADJUSTED* DIFFERENCE IN DIFFERENCE ESTIMATE | p-VALUE | |
|---|---|---|---|---|
| WINTER COHORT | COMPARISON COHORT | |||
| Potentially preventable hospitalisations | –0.9 (–0.91, –0.89) | –10.0 (–10.13, –9.94) | 1.67 (1.21, 2.27) | 0.0018 |
| All cause hospitalisations | –3.4 (–3.55, –3.48) | –34.1 (–34.14, –34.06) | 1.52 (1.31, 1.79) | <0.0001 |
| Unplanned hospitalisations | –3.1 (–3.11, –3.09) | –29.3 (–29.25, –29.4) | 1.62 (1.31, 1.94) | <0.0001 |
| Planned hospitalisations | –0.4 (–0.41, –0.39) | –4.7 (–4.71, –4.67) | 1.31 (1.00, 1.94) | 0.047 |
| Total emergency department presentations (total) | –15.4 (–15.66, –15.14) | –37.8 (–37.90, –37.75) | 1.26 (1.04, 1.52) | 0.018 |
| Semi urgent and non-urgent emergency department presentations | –6.2 (–6.44, –5.94) | –9.1 (–9.11, –9.08) | 1.16 (0.87, 1.54) | 0.32 |
| Potentially preventable bed days | 7.8 (7.47, 8.13) | –55.7 (–55.91, –55.49) | 1.53 (0.94, 2.48) | 0.09 |
| Total NWAU | –10.6 (–10.61, –10.52) | –52.9 (–52.83, –52.94) | 1.43 (1.13, 1.81) | 0.0028 |
[i] * Adjusted for sex, marital status, year of birth and SEIFA; generalised estimating equation with the log link function, negative binomial distribution, and compound symmetry correlation structure.
458 participants from the Winter Strategy 2017 had 24 months follow up data. An adjusted difference in difference analysis for 24 months post intervention showed reconciliation for the rates of potentially preventable bed days between the two cohorts by 24 months (p value = 0.49), as well as the number of planned hospitalisations (p value = 0.34) and total NWAUs (p value = 0.07). The magnitude of decline continued to be greater in the comparison cohort for all cause hospitalisations, unplanned hospitalisations, potentially preventable hospitalisations and emergency use (Supplementary material Table 2).
Matching analyses using different criteria were performed as a sensitivity analysis. Matching criteria included complete matching of all characteristics, matching based on comorbidities and matching based on a combination of comorbidity and service utilisations. Overall it was difficult to generate similar pre-intervention utilisation trends in the two cohorts. Strengths and limitations of each of the sensitivity matches are outlined in the supplementary material.
Discussion
In this study, we evaluated the implementation and outcomes of an integrated strategy to more effectively address the needs of patients with chronic and complex conditions in Northern NSW, Australia during the winter months of 2017 and 2018. The participants enrolled demonstrated a high rate of comorbid health conditions and most people (94%) had utilised some hospital services in the preceding 5 years before the intervention commenced. Approximately two thirds of the selected cohort had been admitted to hospital at least once over this period. The strategy was associated with pre-post improvements in provider and patient experience, however there was no reduction in hospital utilisation or cost efficiencies.
The large improvements in primary care clinician experiences are noteworthy, particularly in domains relating to increased confidence in care coordination and care for patients at high risk of deterioration. Favourable clinician experience is necessary for sustainability and as a foundation for further health system integration [23]. Clinicians are often required to do additional work to improve the integration of the health system, which is often not remunerated. The motivation for change in clinician behaviour therefore falls to professional satisfaction.
Improved patient experience is an important outcome, directly linked to the quadruple aim [14]. Participant experience of the Winter Strategy increased after the program for all eight common questions, spanning access to comfort with and understanding of health professionals. This is essential as patient experience from a representative sample of Australians aged over 15 years found that Northern NSW had the highest rate of hospital admission in the country in 2018–2019 (17.5% of adults surveyed, national average 13.0%) and for several patient experience measures, the region was in the lowest performing quartile, 32.0% reported not being able to access their preferred GP; 23.8% felt they waited longer than acceptable to see a GP; 18.7% saw three or more health professionals for the same condition [24]. Consequently, the improvements in experience for Winter Strategy participants are potentially addressing important unmet needs in the region.
A core element to the program logic was strengthening the primary healthcare sector and improving the interface between hospital, specialty, and primary health care. Drawing on Valentijn’s conceptual framework on the integrative functions of primary care, the Winter Strategy sought to influence several of these including: (1) system integration (alignment of rules and policies within a system); (2) organisational integration (enabling the coordination of services across different organisations); (3) professional integration (enabling professionals to coordinate services across various disciplines); (4) clinical integration (care service coordination); (5) functional integration (provision of back-office and support functions); and (6) normative integration (promotion of shared mission and work values) [25]. The favourable clinician experience suggests the strategy addressed some of these functions. However, several barriers to optimal integration were also observed, especially with respect to practice nurse involvement, these included: ADNs not working or not disseminated, insufficient time especially when discharging complex clients, negative impact on existing (CDM) workload especially with additional roles including health coaching, engagement of GPs was variable despite consistent engagement of practice nurses, general practice resource constraints to allow nurses to fully engage in the service enhancements, and challenges with adopting and sustaining allied health service support. Another major implementation barrier was the limited engagement of allied health professionals. The much higher degree of engagement with practice nurses and the relatively sparse engagement with external allied health providers suggests that it is difficult to coordinate a multidisciplinary team when providers are operating in distinct organisations. Although there are existing funding models in Australia for GP referral to allied health services for chronic disease management, these are often underutilised and when they are used are limited to five services per calendar year which may be insufficient for people with complex care needs [26]. These challenges of cultivating a team based approach align with a recent systematic review in which resource availability and interprofessional team engagement were prominent determinants of successful implementation (1). Sustained and progressive integration requires interprofessional and intersectoral relationships of trust and collaboration. These take time to develop, and in a background heath system culture of non-integration, sustained work is required to maintain trust and collaboration.
The lack of demonstrable impact of the Winter Strategy on hospital utilisation has been observed with other integrated care projects [27282930]. We make three observations in relation to this finding: (1) The marked increased in utilisation patterns in both the Winter Strategy and comparison groups (especially for respiratory conditions) could be related to season specific effects – the 2017 winter influenza notification rates were extremely high across NSW [31] and then reduced substantially in 2018 [32]; (2) the Winter Strategy itself led to a higher detection of health issues leading to more hospital utilisation; some patients were encouraged to go to hospital if they were experiencing a deterioration in their health such as chest pain; and GPs may have recommended referring patients to hospital more often due to a higher level of monitoring in the community; and (3) GPs may have selected patients with characteristics that were not used in the matching algorithm, such as social determinants and other vulnerability factors known to the GPs. These factors may have resulted in a differential regression to the mean between the two groups with larger reductions in hospital utilisation in the comparison cohort compared to the Winter Strategy cohort. Feedback from participating clinicians indicated that the practice’s experience in identifying, delivering and coordinating care for these patients incorporated additional factors, such as health behaviours and social determinants of health not available in routine datasets. [3334]. Expanded datasets with inclusion of key variables such as primary care utilisation, medication use, mental health and social determinants of health could address this.
In addition to potential unobserved confounding in developing a matched comparison group, other study limitations include: (1) despite high response rates, use of pre-post self-reported data for patient and clinician experience may not be a reliable measure; (2) lack of access to process measures around general practice utilisation, medication usage and diagnostic tests limits our ability to fully appraise changes in care patterns in the primary care sector; (3) patients in the Winter Strategy and the control group may have utilised health care in other jurisdictions beyond the geographic catchment of this study and this may lead to an underestimate of true utilisation rates; and (4) patients who have been identified by a practitioner as being unsuitable for the program may have been identified as matched controls in the comparison cohort, however due to the number of potential matched controls, selecting these patients was unlikely.
The selection of the comparator cohort is a crucial limitation for the Winter Strategy. A randomised control trial would have allowed for balance over a range of important covariates including clinical and demographic characteristics and health care provision. However, the strategy presenting in this study was designed through a collaboration between a Primary Health Network and the Local Health District (responsible for public specialists and hospital services), as such a randomised controlled trial was not an acceptable implementation model to meet their service provision needs and contractual obligations. Balancing the need for research rigour and the sensitivities of service providers, this study represents an innovative approach in Australia that has important lessons for other health systems experiencing similar fragmentation challenges.
Conclusion
The Northern NSW Winter Strategy sought to increase patient self-management and the capacity and capability of general practice and hospital services to respond proactively to at-risk patients and improve the integration of care. The Winter Strategy was associated with improvements in patient and clinician experience measures but was not associated with reduced hospital utilisation.
Additional Files
The additional files for this article can be found as follows:
SF5
Supplementary Tables 1 to 3 and Supplementary Figures 1 and 2. DOI: https://doi.org/10.5334/ijic.6549.s2
Reviewers
Paresh Dawda, Adjunct Professor, University of Canberra and Adjunct Associate Professor, UNSW and Principal, Prestantia Health, Australia.
Richard Lewanczuk, (Senior Medical Director – Health System Integration), Alberta Health Services, Alberta, Canada.
Funding Information
This work was funded by the Agency for Clinical Innovation. The funder had no role in any aspects of the study. BA is supported by an NHMRC Emerging Leadership Grant (GNT2010055).
Competing Interests
The authors have no competing interests to declare.
