Table 1
Characteristics of the six case management programs.
| CHARACTERISTIC | CASE | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| Population of hospital service zone in 2017 (n) | 78 824 | 67 264 | 22 554 | 52 855 | 25 615 | 31 500 |
| Area of the hospital service zone (km2) [29] | ||||||
| CRM | 1 126 | 2 781 | 36 770 | 17 799 | ||
| City-center | 156 | 216 | 262 | 196 | 296 | 153 |
| Population density (resident/km2) | ||||||
| CRM | 0.6 | 18.6 | 0.7 | 1.8 | ||
| Main city | 384.4 | 253.9 | 75.9 | 237.2 | 50.3 | 71.3 |
| Year of CMP creation | 2009 | 2012 | 2013 | 2012 | 2015 | 2013 |
| Case manager | Nurse-social worker dyad | Social worker | Nurse | First: nurse-social worker dyad Later: only a nurse | Social worker | First: nurse-social worker dyad Later: only a nurse |
| ISP access modality for healthcare providers (other than case manager) | No access | Hard copy folder (n = 1) in the ED | Hard copy (n = 1) in the ED | Digital folders (n = 3) | Digital (n = 1) folder in the ED | Digital (n = 1) and hard copy (n = 1) folders in the ED |
[i] CMP: case management program; CRM: County regional municipality; ED: Emergency department; ISP: Individual service plan.
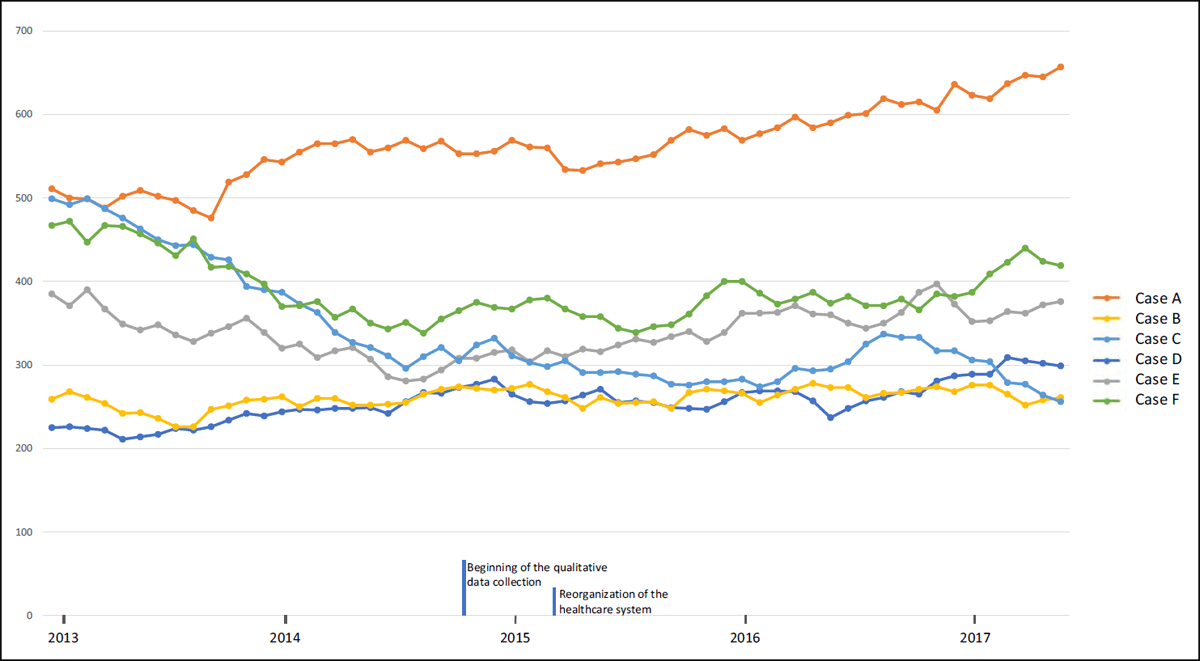
Figure 1
Number of ED frequent users* for each hospital.
* FU: 6 ED visits or more in the previous year.
Table 2
Case management program (CMP) implementation in each setting: case stories.
| CASE | DESCRIPTION |
|---|---|
| A | Located in the largest urban centre of the region, this CMP began as a committee of health and social care providers, from various hospital departments, and dedicated to the case management approach with their respective clientele. Then, an official CMP was launched to serve a larger volume of patients. It was led by a nurse-social worker dyad who identified frequent ED users in real-time, thereby ensuring timely patient management. Due to the considerable number of health and social services organizations and providers in this area, interpersonal connections and knowledge between the local actors were difficult to achieve. The care was thus siloed rather than integrated and coordinated. The reorganization of the Quebec healthcare system in 2015 had major impacts on health and social services in general, and on the CMP in particular, including staff turnover at the intermediate and senior management levels and a general climate of insecurity regarding the program sustainability. Due to the reorganization and despite the senior manager’s wish to maintain all CMP activities, the CMP was stopped in November 2015. In May 2018 (the end of the qualitative data collection phase), it had still not been rebooted. The quantitative data indicate a decrease of ED frequent users at the beginning of the program, while a continuous increase in the number of ED frequent users began when the CMP stopped. |
| B | Based in the second largest urban hospital in the region, the CMP served a population with a high prevalence of mental health disorders and social problems. The case manager was a social worker who was not only responsible for coordinating patient care, but who also worked with patients to reduce their high use of care services. Over the course of this study, there was a high turnover of case managers and this seemed to influence the engagement and openness of patients and providers towards the CMP. Moreover, changing leadership among the case managers resulted in mixed program effects over the years. The reorganization of the healthcare system generated staff turnover and shortage as well as lack of other resources (e.g. physical place to work). Consequently, providers were dissatisfied with the CMP implementation and, ultimately, became reluctant to accept any new initiative from senior managers or health authorities, including the CMP. However, with the support of senior managers, the CMP was maintained. The number of ED frequent users remained stable over the study duration. |
| C | The CMP was in a small rural area close to an urban centre; thus, benefiting from geographic proximity between patients and providers. Given that the case manager worked near the family physicians in the clinics, information circulated fluidly, and patient follow up was rapid. Many patients of this CMP were elderly or had chronic pulmonary disease. The case manager was an experienced nurse who was well known by patients and providers before the CMP implementation because this person had been working in the area for many years. Moreover, since becoming the case manager of this CMP in 2013 when it began, this person had worked hard to make herself even more known among the CMP stakeholders and to build relationships with providers. Given these relationships of trust, the initial resistance to the CMP was reduced. Additionally, because the case manager met with patients and ED personnel frequently, follow up was more rapid and efficient. Finally, due to the strong support from senior manager, the case manager had a lot of autonomy, and was thus able to adapt to the needs of patients and providers. Over the course of the case study, the CMP did not change very much. In fact, the potential negative effects of the reorganization of the Quebec healthcare system on the CMP were mitigated by the stability of the case manager and the management team. The number of ED frequent users decreased steadily during the study period. |
| D | The hospital deploying this CMP serves a small territory facilitating inter-professional and inter-organizational collaboration, particularly between family physicians and the case manager. At the beginning of the program in 2012, an emergency nurse identified frequent users who were referred to family physicians. Three years later, in 2015, a part-time case manager was hired, but in a nearby clinic, not in the hospital. To improve coordination, two teams, each composed of a part-time dedicated nurse, a nursing assistant and a family assistant were created in two neighbouring localities near the hospital. However, the lack of support and unclear guidance from managers, and the demobilization of health and social providers due to the reorganization of healthcare system in 2015, led to the replacement of these teams by the part-time case manager from another area, which had to coordinate a much larger territory (see case F). Despite the many challenges this case manager faced (e.g. remote coordination, lack of time, creation of links with managers and health and social providers), and due to her expertise, this person was able effectively lead the CMP. The number of ED frequent users remained fairly stable over the study duration. |
| E | Liaison nurses assigned to this CMP included organizations that had pre-existing partnerships and a strong potential for collaboration in CMP, namely the hospital’s ED and mental health department, and the service area’s family medicine groups and local community health centre. In March 2015, just after its implementation, the CMP was interrupted due to the reorganization of the health and social services system. Thanks to the initiative of senior and intermediate managers, the CMP activities were temporarily resumed at the end of 2016, but stopped for a second time in the summer of 2017 due to persistent management and clinical staff’s instability. Given this short time frame (six months), the new nurse case manager was unable to create and consolidate collaboration among all CMP organizations. In March 2018, a new part-time social worker case manager was assigned to the CMP. In December 2018 (about the end of the qualitative data collection period), this case manager had still not received a training. The number of ED frequent users remained fairly stable for the duration of this study. |
| F | The CMP began in 2013, initially with a dyad composed of a nurse and a social worker. During the first year, human resources turnover in the hospital resulted in program interruptions. Following the reorganization of healthcare services in 2015, only the nurse stayed part-time as the case manager and focussed for the most part on elderly patients. The geographic proximity and leadership of this person helped to nurture partnerships with ED social workers, physicians and family medicine groups. For example, the case manager established a formal referral structure that linked family physicians, nurses, patients, and himself. By the end of the data collection, the case manager had finally been assigned full time to implement and execute the CMP in cases D, E and F. There were now enough human resources to deploy the CMP and consolidate existing partnerships. The number of ED frequent users decreased over the study period. |
Table 3
Structural, environmental, and organizational characteristics influencing integrated care, self-management and health services use for each case.
| CATEGORIES EMERGING CHARACTERISTICS | OUTCOMES | |||||
|---|---|---|---|---|---|---|
| CASE A | CASE B | CASE C | CASE D | CASE E | CASE F | |
| Structural and environmental-level factor | ||||||
| (+) Proximity between providers | ↑patient support (1.1) | ↑ communications between healthcare professionals (1.2) ↑ healthcare transition (1.6) | ↑ communications between healthcare professionals (1.2) ↑ healthcare transition (smaller ↑ for remote services) (1.6) | ↑ collaboration with medical teams leading to ↑ comprehensive care and ↑ understanding of patient needs (1.1) ↑ communication between case manager, managers and healthcare professionals (1.2) | ||
| Organizational-level factor | ||||||
| (–) Staff turnover and healthcare teams’ instability | ↓continuity of care (1.6) | ↓ case manager follow-up with healthcare professionals (1.2) | ↓ continuity of care and ↑ repetition of patient medical history (1.6) | ↓ consistency of patient support (1.1) ↓ patient information (1.2) ↓ continuity of care (1.6) | ||
| (+/–) Information access/No information access | ↑response to patient needs (1.1) ↓ inadequate use of healthcare services given emergency nurses’ access to ISP* (3) | ↓ assessment of patient situation (1.3) ↓ continuity of care between hospital and clinics (1.6) ↓ continuity of care when ISP not accessible to all healthcare professionals (1.6) | ↑ response to patient needs (1.1) ↑ communication between case manager, ED physicians, and liaison and mental health nurses (1.2) | ↑ health care transitions (1.6) | ||
| (+) Manager support | ↑ service access for patients with most complex needs (1.1) ↑ service trajectories (1.6) ↓ use of health and social care services (3) | ↑ case manager legitimacy and autonomy → new trajectories of care and ↑ continuity of care (1.6) ↓ use of healthcare services (3) | ||||
[i] ISP: Individualized services plan.
Table 4
Practitioner and patient characteristics influencing integrated care, self-management and health services use for each case.
| CATEGORIES EMERGING CHARACTERISTICS | OUTCOMES | |||||
|---|---|---|---|---|---|---|
| CASE A | CASE B | CASE C | CASE D | CASE E | CASE F | |
| Practitioner-level factor | ||||||
| (+) Case manager leadership (skills, attitudes and personal qualities, previous experience, networking) | ↑ access to other healthcare providers; leads to better follow-up and ↓ healthcare use (3) | ↑ patient-centred care and ↑ access to adapted services (1.1) ↑ continuity of care (1.6) ↓ ED visits (because new CTs (3) | ||||
| (+) Provider engagement | ↑ collaboration, communication and exchange of patient’s information between local community health centre and the hospital (1.2) | |||||
| (+) Inter-professional collaboration | ↑ follow-up and a ↑ response to patient needs (1.1) | ↑ sharing and discussion on patient information (1.2) ↓ healthcare use (3) | ↑ access to clear and concise patient information (1.3) ↑ continuity of care and care planning (1.5, 1.6) ↑ consultations with other healthcare professional (patient doesn’t need to repeatedly see doctor for referrals) (3) | ↑ knowledge of patient’s overall situation (1.1) ↑ communication between healthcare professionals (1.2) ↑ patient knowledge of care plan (1.3) ↓ patient repeating their medical history (1.6) ↑ patient appropriate use of resources (3) | ||
| Patient-level factor | ||||||
| (+) Anxious patient | ↑ patient confidence (given reassurance from case manager) (2) ↓ ED visits (3) | |||||
| (+) Patient with self-management skills | ↑ patient proactivity in their health and healthy lifestyle choices (2) ↓ ED visits (3) | ↑ patient proactivity in their care and healthy lifestyle choices (2) ↓ ED visits (3) | ||||
[i] CT: care trajectory; ED: emergency department.
Table 5
Characteristics of the innovation (the CMP) influencing integrated care, self-management and health services use for each case.
| CATEGORIES EMERGING CHARACTERISTICS | OUTCOMES | |||||
|---|---|---|---|---|---|---|
| CASE A | CASE B | CASE C | CASE D | CASE E | CASE F | |
| Innovation-level factor | ||||||
| (+) Individualized service plan (ISP) | ↑ patient support and follow-up (1.1) ↑ patient involvement in their care (1.4) ↑ access to care (1.6) | ↑ care planning (1.5) | ↑ inter-professional communication (1.2) | ↑ inter-professional collaboration, proximity and knowledge among healthcare professionals, which ↑ communication (1.2), information sharing and discussion (1.3) and healthcare transitions (1.6) | ↑ healthcare professionals’ knowledge of the ISP (1.3) | |
| (+) Consideration of patient and family needs | ↑ patient adherence to the program (1.1) ↓ healthcare use (3) | ↑ case manager’s information access (1.3) ↑ patient participation in shared decision-making (1.4) | ↑ patient-provider relationship of trust, thus ↑ response to patient needs (1.1) and self-management support (2) | ↑ patient’s involvement in shared decision-making (1.4) | ||
| (+) Self-management support approach | ↑ patient confidence, which leads to decreases their health services use (3) | ↑ case manager and patient relationship of trust, thus ↑ communication (1.2) | ||||
| (+/–) Relatives’ participation in decision-making/relatives support | ↑ knowledge of patient needs and situation, thus ↑ patient follow-up (1.1) ↑ bidirectional information sharing (1.2, 1.3) | ↑ knowledge of patient needs and situation (1.1) ↑ patient and relatives’ awareness of the care plan (1.3) | ↑ patient adherence to ISP (1.5) ↓ hospitalization when relatives take patient to ED (3) | ↑ response to patient needs (if very complex needs) (1.1) ↓ services use (3) ↑ use of care plan (1.5) by patients with low literacy (due to self-management support) (2) | ||
| (+/–) Case manager access to information | ↑ relevance of response to patient needs (1.1) ↑ ISP efficiency (1.5) | ↑ inter-professional communication (1.2) | ↑ continuity of care (1.6) | |||
[i] ISP: Individualized services plan.
