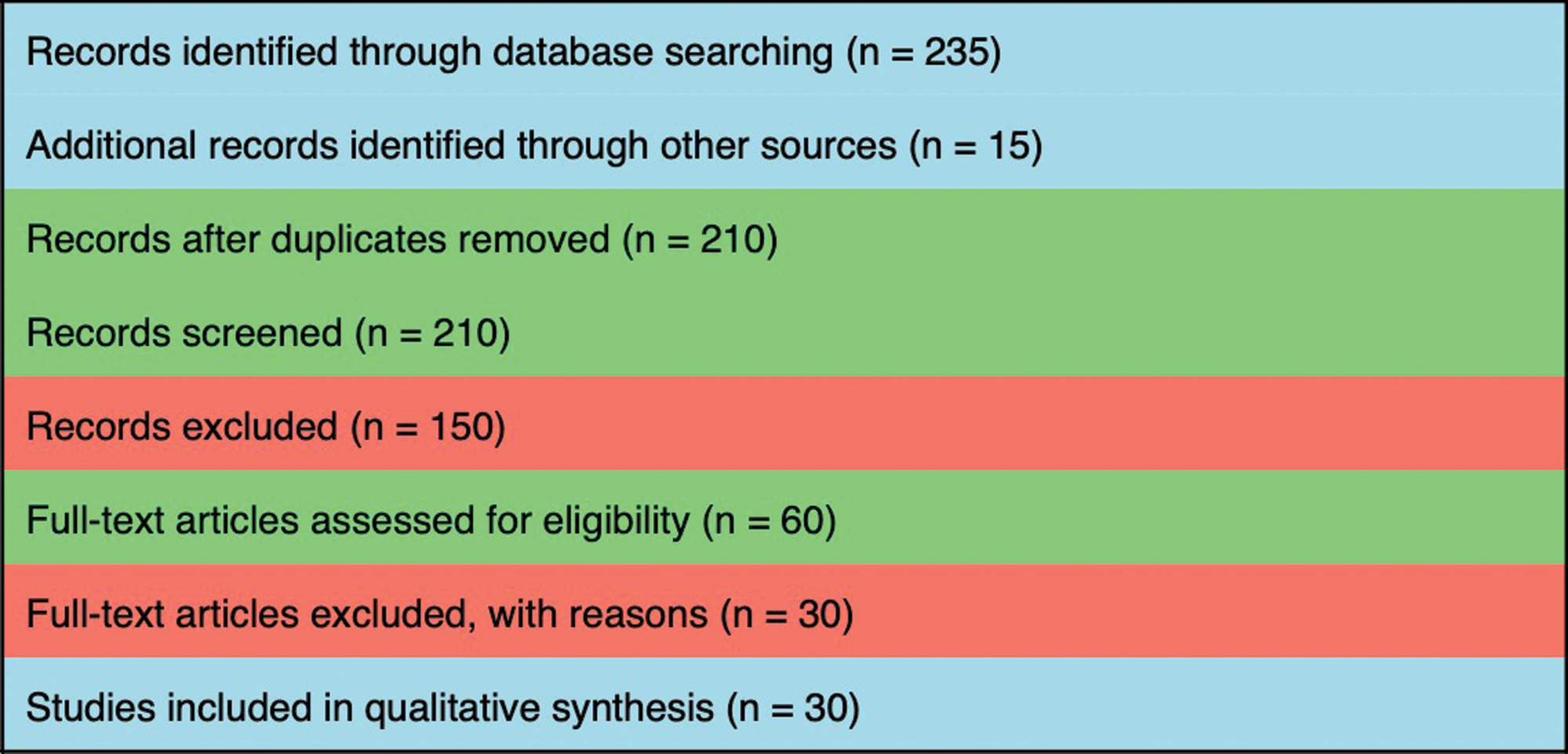
Figure 1
PRISMA flow diagram.
Table 1
Tabular representation of the recent most studies on microplastics.
| AUTHOR (YEAR) | STUDY TYPE | MODEL/POPULATION | MAIN FINDINGS |
|---|---|---|---|
| Paul MB et al. [10] | Narrative review | Literature (oral uptake focus) | Comprehensive review of oral uptake, fate, and potential toxicity of micro‑/nanoplastics (MNPs); highlights major knowledge gaps regarding exposure, biodistribution, and effects after oral uptake. |
| Mahmud F et al. [15] | Narrative review | In vitro and in vivo studies aggregated | Summarizes molecular/cellular effects of MNPs: induction of reactive oxygen species (ROS), inflammation, and senescence markers across cell lines and animal models; links MNP exposure to inflammatory and aging pathways. |
| Yang ZS et al. [16] | In vivo experimental | Mice, single oral exposure to MNPs | Demonstrated rapid absorption and distribution of NPs/MPs to blood and tissues (including adipose, nervous, and reproductive); shows size‑dependent biodistribution and tissue invasion after oral exposure. |
| Zeng G. et al. [17] | Experimental (cellular + animal) | Caco‑2 and mouse intestinal models | Polystyrene microplastics induced oxidative stress and intestinal barrier dysfunction via ROS → NF‑κB / NLRP3 / IL‑1β / MLCK pathway; antioxidants and inhibitors attenuated effects. (Mechanistic evidence for ROS → barrier dysfunction.) |
| “Impact of Micro‑ and Nanoplastics on Human Health” (review, 2020 PMC) | Narrative review | Broad literature synthesis | Reviews multiple organ/system effects of MNPs; summarizes mechanisms (oxidative stress, inflammation), and highlights the lack of human epidemiological evidence for many endpoints. Provides useful background for systemic consequences of oral exposure. |
| Polystyrene MPs — recent mechanistic papers (2024–2025) | Experimental studies | Cell and animal models | Multiple recent studies show PS‑MPs promote oxidative stress, mitophagy alterations, and epithelial barrier dysfunction; antioxidant interventions reduce injury in some models (Collective mechanistic support for ROS → tissue dysfunction.) |
| Reviews connecting MNPs ↔ oral uptake & toxicity (2020–2023) | Reviews/perspective articles | Aggregated literature | Several recent reviews converge on the oral route as an important exposure path; emphasizes oral cavity as both a portal and a local exposure site; calls for targeted oral/gingival studies. |
| “Beyond microplastics — submicron plastics” (SpringerOpen, 2022) | Perspective/review | Literature | Discusses (sub)micron plastics, analytical challenges, and the relevance of small particles to tissue penetration—important context for particle size relevance to gingival penetration. |
| Polystyrene MP studies showing inflammatory signaling (various 2023–2024) | In vitro/in vivo mechanistic | Cell lines, rodents | Convergent evidence shows that PS microplastics trigger NF‑κB signaling and NLRP3 inflammasome activation in epithelial and immune cells—a plausible route to chronic inflammation. |
| Systematic/narrative syntheses of MNP immunotoxicity (2022–2024) | Systematic and narrative reviews | Aggregated experimental studies | Reviews indicate consistent induction of oxidative stress and inflammatory mediators by MNPs, but note limited data on oral mucosa and periodontal immune responses specifically—a major evidence gap. |
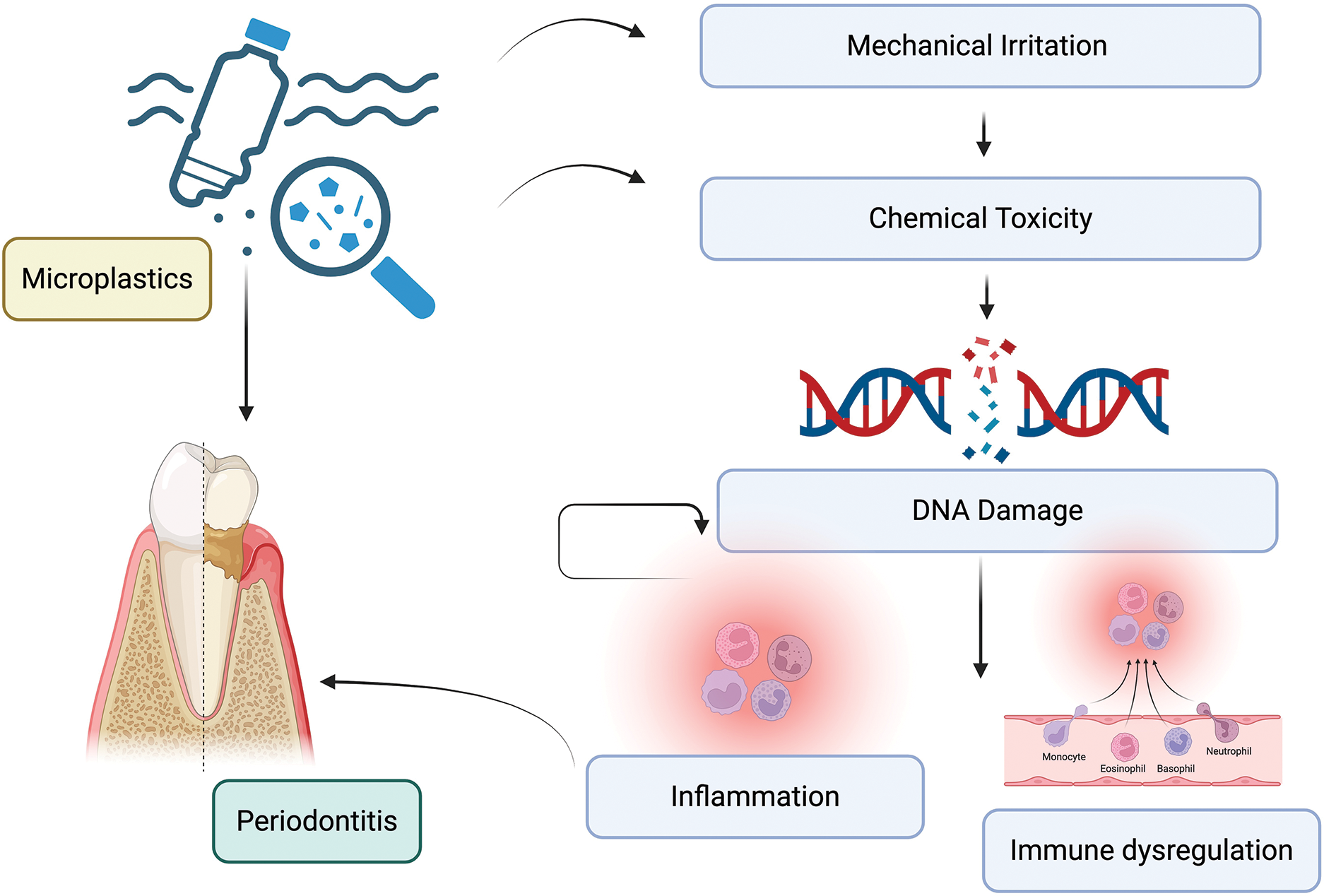
Figure 2
Mechanisms of action of microplastics on periodontium.
