1. Introduction
Antimicrobial stewardship (AMS) involves systematic actions aimed at improving patient outcomes, limiting adverse events, and curbing the emergence and spread of antimicrobial resistance (AMR) [1]. In the Council Recommendation of the European Centre for Disease Prevention and Control (ECDC) to face antimicrobial resistance, an EU target on total antibiotic consumption to be reached by 2030 is set with a One Health approach. However, antimicrobial consumption (AMC) data of 2022 were worrying, with half of the ECDC member states, including Italy, having AMC values above the EU mean consumption rate in 2019 and even higher AMC rates in 2022—unlike from Finland, the Netherlands, and Sweden, which had already reached their recommended target AMC level for 2030 in 2022 [2]. Since 2015, when the 68th World Health Assembly (WHA) approved the Global Action Plan (GAP) on Antimicrobial Resistance (AMR), the World Health Organization (WHO) invited countries to formally commit themselves to addressing AMR [3]. To face this challenge a multifaceted strategy is needed, with a diversified approach including improvements in clinical practice, a proper use of antimicrobial agents, and strategies to increase the knowledge of AMR [4].
As largely demonstrated in the literature, implementing national strategies to limit AMR can be challenging and time-consuming without a multidisciplinary approach. However, AMS predominantly remains a domain of doctors and pharmacists [5]. In this regard, nurses, who play a pivotal role in patient management, have been shown to impact clinical outcomes significantly [6]. Being involved in every phase of patient care, from admission to discharge, together with doctors and other healthcare professionals, nurses are often the first line of defense [7], with a potential key role in reducing the spread of colonization and infections by managing an appropriate antimicrobial strategy [8].
Furthermore, as self-medication and patient expectations from medicaments are some of the leading causes of AMR [9], nurses would play a crucial role in patient education [6], guiding them toward a more conscious use of antimicrobial agents [10].
In this regard, as stated by Hamdy et al. in 2019 [11], nurses have the possibility to identify and bridge communication gaps between doctors and patients or their families, explaining the use and risks of antimicrobials. Additionally, nurses feel often capable of acquiring knowledge about antimicrobial use, becoming passionate and proactive about antimicrobial use, expressing a strong desire to enhance their knowledge, and being motivated to have a role in AMS, although perceiving a lack of educational focus on antimicrobials within nursing practice [12]. In this regard, it has been found globally that nurses feel inadequately prepared to participate in antimicrobial stewardship due to a lack of education and supportive hospital culture [13]. In this aspect, the AMR EDUCare project highlights a lack of implementation of the educational aspects of national action plans on AMR with a disparity in the availability of AMR education among healthcare workers, including nurses, in many European countries, including Italy [14]. This has lead to a lack of recognition of their position in the management of AMR [15], which tends to focus on physician- and pharmacist-led stewardship interventions. Additionally, AMR educational programs rarely target nurses, and this oversight is relevant, as a lack of understanding of AMS principles and a lack of knowledge of proper antimicrobial use may affect prevention and control strategies. Recent studies have highlighted that the spread of antibiotic resistance was higher in settings where there was a limited awareness and knowledge regarding the use of antibiotics [16]. By adhering to educational strategies, guidelines, and protocols, healthcare professionals can effectively reduce the risk of AMR and improve patient outcomes through better disinfection and antimicrobial stewardship practices. Educational programs on AMR for healthcare professionals can be delivered through training programs, workshops and seminars with interactive sessions (including case studies, role-playing, and group discussions [17]), as well as through refresher courses following IDSA (Infectious Diseases Society of America) and WHO guidelines and good clinical practice protocols for disinfection and AMS, focusing on practical aspects such as practice protocols for disinfection and the five moments of hand hygiene [18].
These findings underscore the distance yet to be covered to enhance local and national AMR containment efforts by improving the KAP of nursing staff.
The present study aims to explore the determinants of nurses’ KAP regarding AMR in an Italian multicenter study, offering insights for tailored interventions to prevent the emergence and spread of drug-resistant pathogens.
2. Materials and Methods
2.1 Study design, setting, and population
This is a cross-sectional, multicenter survey conducted from 21 October 2022 to 12 June 2023. An anonymous online questionnaire was administered to Italian nurses, nursing students, and other healthcare professionals, regardless of the setting or region in which they were working. For recruitment, we employed convenience sampling, and no exclusion criteria were applied in this study. The study followed STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for observational studies [19]. Data were collected and managed using the REDCap mobile app electronic data capture tool hosted at Catholic University of the Sacred Heart, Rome.
2.2 Questionnaire structure
Data were collected by administering a structured questionnaire consisting of 58 close-ended questions divided into 3 parts. The first section gathered personal information (e.g., age, sex, education), the second part evaluated AMR awareness, and the third part focused on attitudes and practices.
2.3 Study endpoints
The primary endpoint of this study was to assess the KAP scores related to AMR among nursing students, nurses, and other healthcare professionals. Secondary endpoints included evaluating the association between demographic and professional characteristics (e.g., gender, geographical location, and source of AMR training) and the KAP scores, as well as identifying variables that significantly influence the KAP scores.
2.4 Statistical analysis
A descriptive analysis was performed to define the distribution of baseline variables and characteristics of the sample. The dependent variable was a good AMR KAP, and a score higher than the median result (12 points) was considered “good knowledge” of AMR. Continuous variables were compared between groups using the Mann-Whitney U test, while categorical variables were analyzed using a chi-squared test. A logistic regression model was used, with AMR good knowledge as the dependent variable and the available factors at the baseline evaluation as independent variables in the univariate analysis. Variables found to be significant (p-value < 0.05) in the univariate analysis were included in the multivariate analysis. The strength of the association between baseline factors and good AMR CAP (outcome) was measured using adjusted odds ratios (aORs) with 95% confidence intervals (CIs). All statistical tests were two-tailed, and a p-value < 0.05 was considered statistically significant. Statistical analyses were performed using R Statistical Software (v4.1.3; R Core Team 2021) in R Studio Version.
2.5 Ethical approval
Ethical approval was not required; participation was voluntary, anonymous, without compensation, and did not involve the collection of clinical data. Informed consent for completion of the questionnaire was declared on the first page. However, the study was conducted in accordance with the Declaration of Helsinki and national and institutional standards.
3. Results
As shown in Table 1, a total of 848 nursing students, nurses, and other healthcare professionals participated in the survey. Among them 61.9% (n = 525) were students, while 37.3% (n = 316) were registered nurses. The majority of the population (71.58%, n = 607) identified as female, and the median age was 22 (IQR 21–25), with 82.3% (n = 698) residing in southern Italy. Most of the interviewed were students (61.9%, = 525), with 55.9% of them attending second or third year of university, and 39.6% (n = 336) scored as having “low KAP,” with a median of the years of service of 6.50 (IQR 3–11.5). Figure 1 show the response to selected questions.
Table 1
Descriptive characteristics of 848 participants stratifying for high or low knowledge of AMR.
| OVERALL (N = 848) | HIGH KAP2 (N = 512) | LOW KAP3 (N = 336) | P-VALUE | |
|---|---|---|---|---|
| Which gender do you identify with? | ||||
| Female | 607 (71.6%) | 393 (76.8%) | 214 (63.7%) | <0.001 |
| Male | 229 (27.0%) | 114 (22.3%) | 115 (34.2%) | |
| Nonbinary | 4 (0.5%) | 3 (0.6%) | 1 (0.3%) | |
| Other | 2 (0.2%) | 0 (0%) | 2 (0.6%) | |
| Missing | 6 (0.7%) | 2 (0.4%) | 4 (1.2%) | |
| Age | ||||
| Median [Q1, Q3] | 22.0 [21.0, 25.0] | 22.0 [21.0, 26.0] | 22.0 [21.0, 24.0] | 0.0014 |
| Missing | 14 (1.7%) | 6 (1.2%) | 8 (2.4%) | |
| Current position | ||||
| Working | 316 (37.3%) | 217 (42.4%) | 99 (29.5%) | <0.001 |
| Studying | 525 (61.9%) | 294 (57.4%) | 231 (68.8%) | |
| Missing | 7 (0.8%) | 1 (0.2%) | 6 (1.8%) | |
| Area | ||||
| Central Italy | 58 (6.8%) | 47 (9.2%) | 11 (3.3%) | 0.00424 |
| Northern Italy | 71 (8.4%) | 44 (8.6%) | 27 (8.0%) | |
| Southern Italy | 698 (82.3%) | 412 (80.5%) | 286 (85.1%) | |
| Missing | 21 (2.5%) | 9 (1.8%) | 12 (3.6%) | |
| Profession | ||||
| Nurse | 307/316 (97.2%) | 213/316 (67.4%) | 94/316 (29.7%) | - |
| Healthcare profession | 8 (0.9%) | 3 (0.6%) | 5 (1.5%) | |
| Bachelor’s degree | ||||
| Other | 2 (0.2%) | 1 (0.2%) | 1 (0.3%) | 0.984 |
| Nursing | 516 (60.8%) | 289 (56.4%) | 227 (67.6%) | |
| Obstetrics (midwife) | 7 (0.8%) | 4 (0.8%) | 3 (0.9%) | |
| Missing | 323 (38.1%) | 218 (42.6%) | 105 (31.3%) | |
| Setting | ||||
| Other services | 209 (24.6%) | 125 (24.4%) | 84 (25.0%) | 0.808 |
| Ambulatory/DH | 6 (0.7%) | 5 (1.0%) | 1 (0.3%) | |
| Intensive care | 35 (4.1%) | 24 (4.7%) | 11 (3.3%) | |
| Obstetrics | 23 (2.7%) | 16 (3.1%) | 7 (2.1%) | |
| Emergency room | 54 (6.4%) | 31 (6.1%) | 23 (6.8%) | |
| Rehabilitation | 12 (1.4%) | 7 (1.4%) | 5 (1.5%) | |
| Surgical setting | 171 (20.2%) | 101 (19.7%) | 70 (20.8%) | |
| Clinical setting | 240 (28.3%) | 150 (29.3%) | 90 (26.8%) | |
| Missing | 98 (11.6%) | 53 (10.4%) | 45 (13.4%) | |
| Academic year | ||||
| First year | 45 (5.3%) | 9 (1.8%) | 36 (10.7%) | <0.001 |
| Second year | 282 (33.3%) | 180 (35.2%) | 102 (30.4%) | |
| Third year | 192 (22.6%) | 101 (19.7%) | 91 (27.1%) | |
| Missing | 329 (38.8%) | 222 (43.4%) | 107 (31.8%) | |
| Years of service | ||||
| Median [Q1, Q3] | 5.00 [2.50, 12.0] | 5.00 [2.00, 12.0] | 6.50 [3.00, 11.5] | 0.27 |
| Missing | 533 (62.9%) | 296 (57.8%) | 237 (70.5%) | |
| Did you receive any education on AMR from your hospital/university? Answer: “Yes” | 156 (18.4%) | 101 (19.7%) | 55 (16.4%) | 0.253 |
| How were you trained on the subject of AMR? | ||||
| Self taught | 315 (37.1%) | 216 (42.2%) | 99 (29.5%) | <0.001 |
| Master courses | 24 (2.8%) | 20 (3.9%) | 4 (1.2%) | 0.0339 |
| University | 519 (61.2%) | 319 (62.3%) | 200 (59.5%) | 0.459 |
| Events funded by pharmaceutical companies? | 8 (0.9%) | 1 (0.2%) | 7 (2.1%) | 0.0156 |
| Hospital meetings | 320 (37.7%) | 195 (38.1%) | 125 (37.2%) | 0.852 |
| Hospital/University meetings with external lecturers | 36 (4.2%) | 25 (4.9%) | 11 (3.3%) | 0.336 |
[i] 1 Bold The p-value represents a statistically significant variable.
[ii] 2 High knowledge, attitude, and practice (KAP) scores related to antimicrobial resistance (AMR).
[iii] 3 Low knowledge, attitude, and practice (KAP) scores related to antimicrobial resistance (AMR).
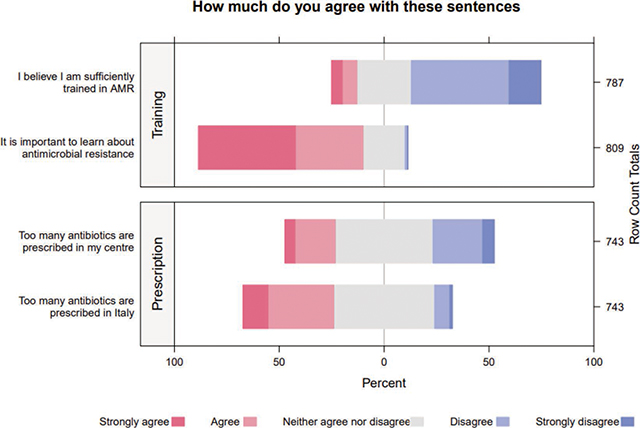
Figure 1
Likert Scale of Training on AMR and Personal Beliefs about the Prescription of Antibiotics.
In the multivariate analysis (Table 2), being female (aOR 1.69, 95% CI 1.23–2.34; p = 0.001) and independently studying AMR (aOR 1.53, 95% CI 1.12–2.11; p = 0.007) were variables associated with a high KAP score. In contrast, residing in southern Italy (aOR 0.47, 95% CI 0.22–0.96; p = 0.04) and receiving AMR training from pharmaceutical companies (aOR 0.08, 95% CI 0.004–0.531; p = 0.02) were associated with a low KAP score.
Table 2
Crude multiple logistic regression for factors associated with high KAP.
| FACTOR | AOR | LOW: 95%CI | HIGH: 95%CI | P-VALUE |
|---|---|---|---|---|
| (reference: Males) | 0.906 | 0.507 | 1.636 | 0.740 |
| Females | 1.699 | 1.232 | 2.344 | 0.001 |
| Being a student | 0.717 | 0.500 | 1.022 | 0.068 |
| Living in Central Italy | 2.507 | 1.098 | 6.029 | 0.033 |
| Living in Southern Italy | 0.479 | 0.220 | 0.962 | 0.048 |
| Being self-taught | 1.538 | 1.126 | 2.110 | 0.007 |
| Having attained a Master class on AMR | 2.954 | 1.020 | 11.169 | 0.068 |
| Working or studying in a setting where AMR training is provided by pharmaceutical companies. | 0.082 | 0.004 | 0.531 | 0.027 |
[i] aOR: adjusted odds ratio; CI: confidence interval; bold p-value represents a statistical significative variable.
4. Discussion
In recent years, nurses are increasingly recognized as key actors in antimicrobial stewardship (AMS) programs due to their unique position within healthcare teams and their direct interactions with patients. Their involvement is crucial in ensuring the appropriate use of antibiotics, which helps in reducing antibiotic resistance, improving patient outcomes, and optimizing healthcare resources [20, 21], with increasing efforts being made to broaden the knowledge in this area [22]. In our study, being female and having studied AMR as an autodidact were associated with high KAP score, while being trained during events funded by pharmaceutical companies and living in southern Italy were linked to low KAP score; however, the latter should be considered as a bias as 85.3 % of enrolled participants worked or studied in southern Italy, with Apulia as the most represented region (53% of the interviewed) (Table 1).
Nurses often exhibit a higher level of awareness about the national action plan on antibiotic resistance, proving to be more capable of adhering to WHO’s five moments of hand hygiene [18] while having the lowest knowledge about antimicrobic use and resistance [23]. A study conducted in Italy in early 2020 demonstrated that also among young doctors, the percentage of correct answers on multidrug-resistant germs was very low, despite most claiming to have a good knowledge on AMR [24]; the same results have been reached by many other studies conducted among under- and post-graduate medical doctors [25, 26]. By contrast, in the present study, most of the participants felt they lacked sufficient AMR training (Figure 1); nevertheless, the highest percentage of correct answers was given in the Knowledge section, while the lowest score was obtained in the Practices section (mean score 6.7 (± 1.4) vs. 4.1 (± 2.3)).
In the Attitude section, it is worth stressing that only 15.7% of the participants agreed with the statement “I dedicate time to educate patients, caregivers, colleagues, support staff about infection risks, mitigation, and AMR management” (Table 3). The relatively high scores in terms of knowledge among all participants can likely be attributed to their young age and recent completion of university studies. However, the lack of experience in clinical practice may have hindered certain skills, such as ensuring that urine bags are not lifted off the ground (Table 3). As expected, the worker group exhibited a higher practice score than the students (4.3 ± 2.1 vs. 4.0 ± 2.4).
Table 3
Composition of the outcome score.
| ITEM | WORKERS (N = 316) | STUDENTS (N = 525) | OVERALL (N = 841) | P-VALUE |
|---|---|---|---|---|
| Knowledge | ||||
| The optimal intravenous infusion time for Piperacillin/Tazobactam is 3 hours/continuous infusion | 152 (48.1%) | 212 (40.4%) | 364 (43.3%) | 0.034 |
| Wearing gloves replaces handwashing | 302 (95.6%) | 510 (97.1%) | 812 (96.6%) | 0.31 |
| The use of hand sanitizer is equivalent to washing hands with soap and water | 204 (64.6%) | 369 (70.3%) | 573 (68.1%) | 0.098 |
| The COVID-19 pandemic has reduced the spread of AMR in our country | 248 (78.5%) | 369 (70.3%) | 617 (73.4%) | 0.011 |
| It is good practice for all hospitalized patients to be under antibiotic coverage | 296 (93.7%) | 419 (79.8%) | 715 (85.0%) | <0.001 |
| In a patient in septic shock, antibiotic administration is one of the actions to be taken during the ‘golden hour’ | 235 (74.4%) | 345 (65.7%) | 580 (69.0%) | 0.010 |
| Which of these procedures is NOT part of the 5 fundamental moments of Hand Hygiene: wash your own hands: | 208 (65.8%) | 279 (53.1%) | 487 (57.9%) | <0.001 |
| Antibiotic resistance is an expressed property | 223 (70.6%) | 385 (73.3%) | 608 (72.3%) | 0.431 |
| KNOWLEDGE SCORE - Mean (SD) | 6.9 (± 1.5) | 6.5 (± 1.4) | 6.7 (± 1.4) | <0.001 |
| Attitudes | ||||
| How willing are you to support a specific Antibiotic Resistance exam during your academic path? | 268 (84.8%) | 384 (73.1%) | 652 (77.5%) | <0.001 |
| How willing are you to attend AMR prevention courses? | 292 (92.4%) | 451 (85.9%) | 743 (88.3%) | 0.006 |
| How willing are you to create a monitoring network for correct antibiotic administration and report any resistance cases? | 291 (92.1%) | 437 (83.2%) | 728 (86.6%) | <0.001 |
| How willing are you to follow indications and procedures that reduce antibiotic resistance? | 300 (94.9%) | 474 (90.3%) | 774 (92.0%) | 0.022 |
| ATTITUDE SCORE - Mean (SD) | 4.6 (± 0.79) | 4.3 (± 1.1) | 4.4 (± 1.0) | <0.001 |
| Practices | ||||
| I wash my hands before putting on gloves | 183 (57.9%) | 276 (52.6%) | 459 (54.6%) | 0.151 |
| I wash my hands after removing gloves | 221 (69.9%) | 326 (62.1%) | 547 (65.0%) | 0.025 |
| I adhere to the antibiotic administration timeframes | 133 (42.1%) | 254 (48.4%) | 387 (46.0%) | 0.088 |
| I use disposable gowns in contact isolations | 175 (55.4%) | 243 (46.3%) | 418 (49.7%) | 0.013 |
| I notice that contact isolations are not adequately indicated | 55 (17.4%) | 112 (21.3%) | 167 (19.9%) | 0.196 |
| I agree that the provided materials (gloves, hand sanitizer, disposable gowns, ROT, etc.) are not readily available | 46 (14.6%) | 95 (18.1%) | 141 (16.8%) | 0.217 |
| I ensure that the urine bag in patients with urinary catheters is lifted off the ground | 174 (55.1%) | 191 (36.4%) | 365 (43.4%) | <0.001 |
| I dedicate time to educate patients, caregivers, colleagues, support staff about infection risks, mitigation, and AMR management | 46 (14.6%) | 86 (16.4%) | 132 (15.7%) | 0.544 |
| Practices score - Mean (SD) | 4.3 (± 2.1) | 4.0 (± 2.4) | 4.1 (± 2.3) | 0.0591 |
| KAP score Mean (SD) | 14 (± 3.0) | 13 (± 3.2) | 13 (± 3.2) | <0.001 |
[i] The table shows the total number and percentage of correct answers. Bold p value represents a statistical significative variable.
Furthermore, in the knowledge section, almost 74% of the respondents agreed with the sentence “The COVID-19 pandemic has reduced the spread of AMR in our country.” Globally, the COVID-19 pandemic led to increased antimicrobial use [27] due to the concern of bacterial co- and superinfections [28], contributing to the spread of multidrug-resistant strains [29]. In particular, during pandemic peaks, there are concerns that the spread of biofilm-producing pathogens such as A. baumannii and Staphylococcus aureus [30] may have been enhanced by the loss of key infection control practices, such as changing or disinfecting gloves when passing from one patient to another. The COVID-19 pandemic has significantly impacted perceptions of AMR. The increased use of antibiotics to treat COVID-19 patients, especially early in the pandemic when the clinical understanding of the virus was still developing, has fueled concerns about AMR. Many COVID-19 patients received antibiotics to treat secondary bacterial infections or out of precaution; this overuse, with the potential to accelerate the development of resistant bacteria, has collectively heightened the urgency to address AMR through improved detection, characterization, and response strategies [31].
In this regard, despite having shown a high capacity for adaptation and a high level of competence in the pandemic [32], during which the role of nurses has been largely glorified by mass media [7], specific AMS interventions targeting or involving nurses were lacking.
Another peculiar finding is that receiving AMR training from pharmaceutical companies correlated with low KAP scores. However, it is crucial to note that only the 1.9 % (N = 16) of the interviewed declared such things, while the majority were trained at university (61.20% [N = 519]) or self-taught (37.14% [N = 315]) (Table 3); this last variable was also associated with a high KAP score (aOR 1.53, 95% CI 1.12–2.11; p = 0.007).
Effective AMR management requires contextualized programs. To enhance nurses’ and other health professionals’ performance, educational strategies aiming to improve self-awareness should be evaluated. In a good AMR monitoring and management program, contextualization is the keystone for a good outcome. It should be noted that in our study while many health professionals were aware of inappropriate antimicrobial prescriptions in Italy, they did not recognize such practices within their own centers. In addition, 86.7% (N = 735) declared not to know a colleague with a specific training on AMR or infection control, and they disagreed that they were sufficiently trained in AMR (Figure 1). Furthermore, only 46% declared to adhere to the antibiotic administration timeframes, and only half of the interviewed (49.7%) declared to use disposable gowns in contact isolations, despite almost all of them declaring that provided materials were available (Table 3). These data are in line with other studies in the literature [33], suggesting that despite personal equipment being present, there is a poor use of devices by the nursing staff. Therefore, to boost the performance of nurses and health professionals, educational strategies in enhancing self-awareness must be evaluated [34].
One of the most important determinants of the emergence of antibiotic resistance is poor training for healthcare professionals [35, 36]. A multicounty study conducted in 2022 clearly demonstrated that nurses with AMS training exhibited higher AMS-related skills, in terms of capability and motivation to perform AMS, emphasizing the impact of quality training on AMS behaviors [37]. Much needs to be done in reducing AMR by improving hospital staff performance and reducing the theory–practice gap [38]. Strategies should focus on continuous education on AMR and AMS, with continuous training and periodical evaluations on knowledge and skills, possibly integrating them into academic curricula and/or specialized degree programs.
Limitations of this study were several: first, the young age of the participants does not give the right representation of the population, considering that the average age of nurses in Italy is 52.2 years [39]. Furthermore, the study recruitment was conducted starting from the region Apulia, and the sample is not representative of the entire country; since, as previously stressed, 53% of the interviewed were from this region, the lack of randomization during the recruitment does not give a faithful view of other contexts. Similarly to other cross-sectional surveys [40], our study represents a single snapshot in a multifaceted panorama, in which evidence and perceptions may vary. Finally, the study relied on self-reported data, which may be subject to social desirability bias.
On the other hand, strengths of the study included the multicenter approach, the relatively high numerosity, the use of a robust data collection tool (REDCap), and the use of a structured questionnaire following standardized guidelines.
5. Conclusions
Good knowledge, attitudes, and practices related to AMR among nurses were associated with being female, working in Central Italy, and relying on self-teaching. Participants demonstrated a positive attitude toward adherence to guidelines and a willingness to engage in further education focused on AMR prevention, indicating a readiness to enhance their professional competencies to combat AMR effectively. However, the study also unveiled concerning practices, such as inconsistencies in the use of disposable gowns in contact isolations and adherence to antibiotic administration timeframes, highlighting areas that necessitate immediate improvement.
Our study offers insights for tailored interventions to prevent the emergence and spread of drug-resistant pathogens, such as an effective training during university years and continuous refresher courses for nurses and hospital staff. The emphasis should be on a multifaceted educational approach that includes active involvement in decision-making processes, patient education, and adherence to best practices in infection control and antibiotic administration. Participants in the study demonstrated a positive attitude toward adherence to guidelines and a willingness to engage in further education focused on AMR prevention. This indicates a readiness to enhance their professional competencies to combat AMR effectively. The evolving landscape of healthcare in 2024 necessitates that healthcare professionals possess a skill set far more diverse and specialized than that of their predecessors from 20–30 years ago. Modern medical and nurse training must now emphasize infection control, climate change, and AMR as essential components. Medical and nurse faculties need to adapt their curricula to provide contemporary and comprehensive training in these areas. By doing so, they will ensure that future healthcare professionals are equipped to handle the complex health challenges of our time [41].
Author Contributions
Conceptualization, FDG. and FVS.; methodology, FVS, FDG.; data curation, G.D.G, R.N., A.A., L.P., D.D.S, G.C., LF.; writing—original draft preparation, EDV. F.V.S., G.C.; writing—review and editing, G.M., A.T., D.M. F.V.S., M.B., N.V., A.D.V.; visualization, F.D.G..; supervision, A.S.; funding acquisition, A.S. All authors have read and agreed to the published version of the manuscript.”
Funding
This research was partially supported by EU funding within the NextGenerationEU-MUR PNRR Extended Partnership initiative on Emerging Infectious Diseases (Project no. PE00000007, INF-ACT).
Ethical Approval
Ethical review and approval were waived for this study due to lack of involvement of human subjects, animals, or plants.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Public Involvement Statement
No public involvement in any aspect of this research.
Guidelines and Standards Statement
The manuscript followed STROBE guidelines for observational studies.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Competing Interests
The authors have no competing interests to declare.
Additional File
The additional file for this article can be found as follows:
Supplementary Table
Distribution of KAP correct answers stratified by job position. DOI: https://doi.org/10.5334/aogh.4488.s1
