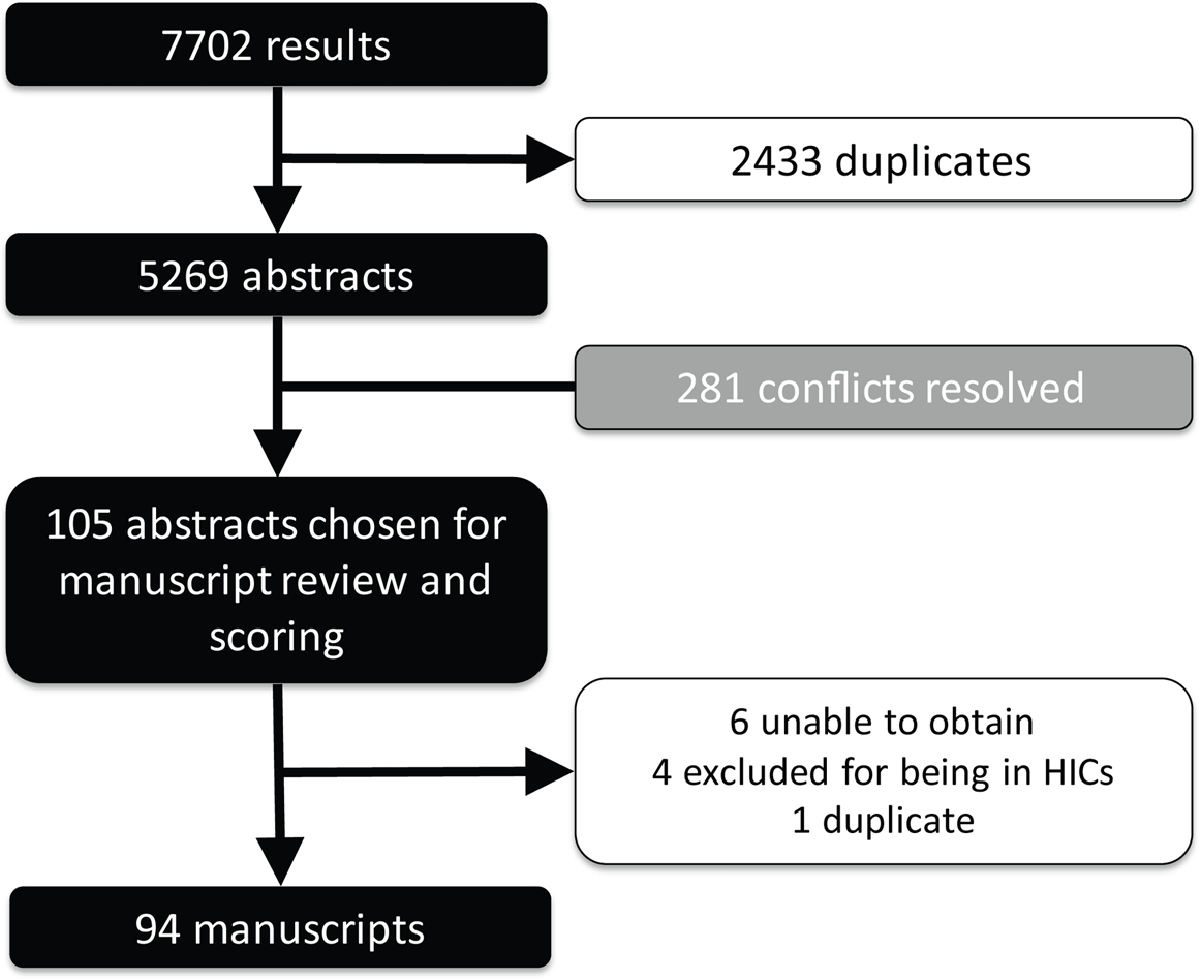
Figure 1
PRISM chart.
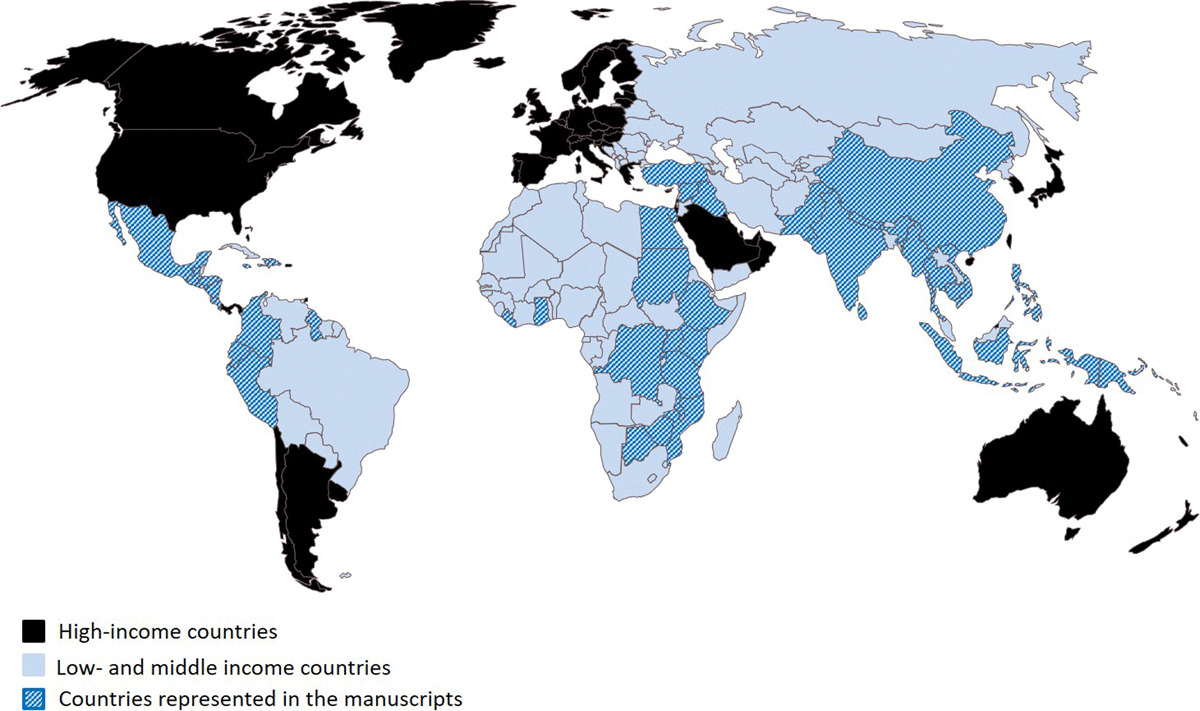
Figure 2
Low- and middle-income countries with programs highlighted in the 94 abstracts.
Table 1
Summary of the 94 included manuscripts.
| Characteristics | Number of Manuscripts |
|---|---|
| Content | |
| Broad EM | 30 |
| Trauma | 18 |
| Pediatrics | 17 |
| Ultrasound | 16 |
| Procedures | 5 |
| Pediatric Trauma | 2 |
| Disaster | 2 |
| Toxicology | 1 |
| Neurology | 1 |
| CPR | 1 |
| Maternal and Child Health | 1 |
| Learners | |
| Physicians | 33 |
| Physicians and Nurses | 17 |
| Multidisciplinary* | 15 |
| Nurses | 8 |
| Medical Students | 6 |
| Health Workers | 4 |
| Physician Assistants/Nurse Practitioners | 1 |
| Unspecified | 10 |
| Program Duration | |
| Short (up to 1 month) | 51 |
| Medium (>1 month to 1 year) | 3 |
| Long (>1 year) | 15 |
| Unspecified | 25 |
[i] * Physicians and/or nurses along with other clinical and non-clinical professions and/or staff.
Table 2
Overview high-scoring manuscripts on content-specific EM programs.
| First Author | Journal | Year Published | Low-resource Setting | Higher-resource Partner | Learners | General Overview (short: up to 1 month; medium: >1 month to 1 year; long: >1 year) |
|---|---|---|---|---|---|---|
| Becker | Trop Med Int Health | 2017 | Ghana | USA | Physicians | Ultrasound, unspecified duration |
| Cioè-Peña | Trauma | 2017 | El Salvador | USA | Physicians and Nurses | Trauma, short duration |
| Crouse | Pediatr Emerg Care | 2016 | Guatemala | USA | Physicians, Nurses, Medical Students, Others | Pediatrics, short duration |
| Denny | World J Emerg Med | 2018 | Tanzania | USA | Physicians, Students, Others | Ultrasound, short duration |
| Henwood | Trop Med Int Health | 2016 | Rwanda | USA, Canada | Physicians | Ultrasound, short duration |
| Kapoor | Emerg Med J | 2016 | Guatemala | USA | Physicians and Nurses | Pediatric Trauma, short duration |
| Kesinger | Injury | 2014 | Colombia | USA | Physicians | Trauma, unspecified duration |
| Merchant | World J Surg | 2015 | Mozambique | USA | Hospital Personnel, Others | Trauma, short duration |
| McCredie | Int Health | 2018 | Nepal | Canada, UK, USA | Physicians | Neurological Emergencies, short duration |
| Meaney | Resuscitation | 2012 | Botswana | USA | All Healthcare Providers | CPR, short duration |
| Reynolds | AfJEM | 2016 | Tanzania, Mexico | USA | Physicians | Ultrasound, short duration |
| Senarathna | PLoS One | 2013 | Sri Lanka | Australia | Hospital Staff | Toxicological Emergencies, short duration |
| Stolz | Trop Med Int Health | 2015 | Uganda | USA | Nurses | Ultrasound, long duration |
| Tafoya | J Emerg Med | 2017 | Ghana | USA | Physicians | Ultrasound, short duration |
| Wanjiku | AfJEM | 2017 | Kenya | USA | Medical Students | Trauma, short duration |
Table 3
Overview high-scoring manuscripts on broad EM programs.
| First Author | Journal | Year Published | Low-resource Setting | Higher-resource Partner | Learners | General Overview (short: up to 1 month; medium: >1 month to 1 year; long: >1 year) |
|---|---|---|---|---|---|---|
| Aggarwal | J Emerg Trauma Shock | 2014 | India | USA | Physicians | Comprehensive long residency program |
| Hammerstedt | Ann Emerg Med | 2014 | Uganda | USA | Nurses | Comprehensive long course; development of new provider level |
| Keyes | Ann Emerg Med | 1999 | Costa Rica | USA | Physicians | Comprehensive long residency program |
| Lim | Afr J Health Professions Educ | 2017 | Tanzania | USA, South Africa | Physicians | Comprehensive long residency program |
| Meshkat | BMC Med Educ | 2018 | Ethiopia | Canada | Physicians | Comprehensive long residency program |
| Mahadevan | AEM Educ Train | 2018 | Uganda | USA | Medical Students | Online vs classroom-based training; short course |
| Niyogi | AfJEM | 2015 | Ghana | USA | Physician Assistants | Task-shifting; short course |
| Pean | Ann Global Health | 2015 | Haiti | USA | Medical Students | Bilateral exchange; short course |
| Reynolds | J Public Health Policy | 2012 | Tanzania | USA, Canada, South Africa | Physicians and Nurses | Comprehensive training at multiple levels up to residency program level (medium and long) |
| Rouhani | Int J Emerg Med | 2018 | Haiti | USA | Physicians | Bridging the gap to residency programs; comprehensive medium-duration course |
| Stanley | Confl Health | 2015 | Thailand/Myanmar | UK | Nurses (and medics) | Primary care setting/front line providers; short course |
Table 4
Program components from the selected manuscripts on broad EM programs.
| First Author | Goals and Objectives | Certification/Recognition | Curriculum Outline/Content | Methods of Assessment | Funding | Logistics | Educational Resources | Outcomes | Challenges |
|---|---|---|---|---|---|---|---|---|---|
| Aggarwal | To provide guidelines for EM curricula in India – residency and medical student | Formal residency training | Core topics and required procedures for residents outlined; off-service rotations (minimum two weeks); medical student rotation (one month); no specific academic activities for medical students; required Casualty (two weeks) or EM (four weeks) posting during internship; no specific academic activities for interns; academic activities are department-wide | Thesis requirement; end-of-rotation assessment; log book; final examination with theory and practical components with short-answer questions, short cases, procedural skills (simulated), and OSCEs | Not discussed | Three-year training program; institutional requirements for ED resources and capacity and EM instructors defined | Calls for re-organization/re-structuring of existing resources; lists commonly used books and journals; reports essential list for departmental library | Clear requirements for institutions for the practice of and training in EM | Ongoing conflict and confusion with other specialty degrees such as trauma and surgery and critical care |
| Hammerstedt | To deliver emergency care through non-physician providers (Emergency Care Practitioners, or ECPs) in rural, low-resource settings | Emergency Care Practitioner certification | Graduated clinical and educational responsibilities; research and quality improvement requirements; weekly conferences comprised of didactic lectures, simulation, and procedural skill laboratories First year (Junior ECP) – 40 hours per week in beside learning; three hours of conference per week Second year (Senior ECP) – lead the junior-level conferences; present morbidity and mortality lectures; bimonthly CME classes on topics such as teaching | Intermittent quizzes and final written and oral examinations; procedure and patient follow-up logs; regular feedback with program director; oral case-based remediation test if needed; regular evaluation by visiting emergency physicians | Non-profit organization (Global Emergency Care) | Two-year program, train-the-trainer model | Core competencies from Uganda’s Medical Education for Equitable Services to All Ugandans and the US’s Accreditation Council for Graduate Medical Education Outcome Project; content developed by global emergency care physicians, the hospital medical superintendent, and faculty from Mbarara University and the Ministry of Health | Emergency care practitioners trained; plans to monitor patient outcomes and to expand to other sites | Tracking outcomes; expansion to other sites; funding; continued international faculty support |
| Keyes | To develop EM as a specialty in Costa Rica | Certificate for the Faculty Preparation Course; formal residency training | Faculty Preparation Course: review of core EM topics and instruction in teaching techniques – two hours on case review and journal club and four hours of lectures as well as clinical rotations (200 hours) and workshops; two-thirds of lectures in flipped classroom format Residency: overlap with the Faculty Preparation Course as well as a preceptor program and weekly grand rounds | Written and oral examinations monthly | Project HOPE, People-to-people Health Foundation and USAID | Faculty Preparation Course on-site by international faculty (one year) followed by the residency program (three years) supported by the first faculty for at least five years; learners included foreign physicians | ACLS, ATLS, PALS; US residency materials adapted to the local setting | 14 graduates from the residency as of 1999 | Attrition; payment for/status of physicians after graduation |
| Lim | To determine the acceptability of small-group learning in EM training | Formal residency training | Initially a lecture-based format in 2010 and redesigned to include small-group learning (40% of the curriculum) in 2014 including case-based seminars, procedure labs, and resuscitation simulations | Described elsewhere – written, oral and practical examinations; quantitative and qualitative survey | Described elsewhere – Abbott Fund Tanzania along with a departmental business plan for financial sustainability | Small groups done weekly (seminars) or 1–2 times per month (procedure labs, simulations) with an instructor-learner ratio of 4-6:1 | Described elsewhere – African Federation for Emergency Medicine; International Federation for Emergency Medicine | Small groups more effective at improving clinical practice and preferred for enjoyment of learning and peer- and instructor-relationship building; preferred by learners with more experience | Novel type of learning; some sessions remain too “lecture-like”; relationship building may be difficult across learner levels |
| Meshkat | To develop and deliver comprehensive EM residency training; specific objectives outlined in the manuscript | Formal residency training | Clinical, Clinical Epidemiology, and EM Administration streams; didactics (separated into blocks), beside teaching, simulation, procedural sessions, and journal club; three half days a week for three months of the year; off-service rotations; formal faculty-resident mentorship program; monthly video conferencing | Session and rotation evaluations; written and practical examinations | University-based funding; Grand Challenges Canada; International Development Research Centre; hospital-based funding | Three-year program with annually repeating junior lecture series and bi-annually repeating senior series; three one-month teaching trips by visiting faculty/senior residents; briefings for visiting faculty; curriculum co-director oversight | Core content based on facility assessment, learner needs assessment, and evaluation of disease burden; free and open-access EM-specific materials listed; University of Toronto postgraduate medical education documents used to develop evaluation methods | The program is in its seventh year as of 2018 with 34 graduates, 20 working in EDs throughout Ethiopia, and 25 modules published online | Development of content by outside experts leads to discordance with local practice and resources; the program was time and resource-intensive in first three years; gaps in visiting faculty led to low morale; internet connection with teleconferencing occasionally poor |
| Mahadevan | To determine differences in knowledge acquisition between online and classroom-based teaching on EM concepts | None | 20 modules; 10–15-minute videos or in-person teaching; case-based | Multiple choice and free-response questions | University-based grant | The online course was offered during 10 weeks of the academic year and the classroom-based course was completed over one week during the school break | Novel course developed by Stanford physicians; clips from the show ER | Both groups improved their scores on the post-test with no significant difference overall between the two groups | High numbers of late enrollees and attrition, especially in online course; the online group post-test was delayed by three months |
| Niyogi | To increase knowledge and to allow for task-shifting in the delivery of emergency care by teaching physician assistants (PAs) to identify and stabilize patients with acute conditions; focus on ABCs | In-service training in the Ghana Health Service | Didactic lectures, problem- and case-based small group sessions, skill stations, simulations, laminated algorithms, and a tabletop mass casualty incident exercise; initial training of trainers and supervision of initial trainings by international faculty | Written testing; observation of learners; case review; simulations | Not described | Nine-day trainer training with a refresher six months later; five-day in-service trainings led by trainers in groups of 2–3 | ABCCC approach from the Integrated Management of Adolescent and Adult Illnesses and the Integrated Management of Childhood Illnesses; Ghana Standard Treatment Guidelines | All post-test scores improved from pre-test scores; the trainer refresher pre-test scores fell nearly to initial pre-test levels, but regional pre-test refresher scores stayed relatively high; 22 initial senior trainers, 39 enrolled in initial regional courses | Decay in knowledge over time; minimal differences in knowledge between trainers and trainees; resource limitations at non-training sites; scope of practice limitations for PAs; lack of familiarity with leading/facilitating case-based methodologies and simulation; refresher courses delayed too long; inability for trainees to leave clinical requirements for the training |
| Pean | To increase knowledge and confidence in emergency response skills using a near-peer model | BLS certification | BLS (three days); EM Module – lectures and skills sessions (two days) | Written examination and observed practical skills examination; fund of knowledge tests and self-efficacy surveys; one-year follow up survey | Self-funded and/or sponsored by private donations as well as Doctor’s Hospital at Renaissance in Edinburg, Texas, and the Icahn School of Medicine at Mount Sinai in New York, New York | One week annually for two years; student to instructor ratio 3:1; follow up survey given during the second year; lectures in the morning followed by skills sessions in the afternoon | BLS resources supplied by the Regional Emergency Medical Services Council of New York City; STRAKER Translations for translating written material; EM Module from the introductory course at Icahn School of Medicine at Mount Sinai | Improvements in fund of knowledge and self-efficacy test scores | Unexpected scheduling changes; language barrier; difficulty with maintaining continuity and connection among cohorts; high levels of non-completion and absenteeism; difficulties in communicating expectations; limited access to electricity |
| Reynolds | To provide multiple levels of training to provide emergency care | Formal residency training – Master of Medicine track | International faculty with transition to local faculty; competency-based; half of the time is spent on rotations in other specialties | Written multiple choice questions and essay exam; oral case-based exam; observed clinical exam (OSCE) with case presentation; professional performance audits | Abbott Fund Tanzania along with a departmental business plan for financial sustainability | 10-module nursing curriculum; 1-year registrar program; 3-year residency program | African Federation for Emergency Medicine; International Federation for Emergency Medicine | 90% of nurses have completed the program; residency graduates since 2013; credentialed registrars | Differences in scope of practice in low-resource settings – curricula and off-service rotations must be modified accordingly; culture of practice slow to change |
| Rouhani | To address a gap in human resources and knowledge in EM until more physicians are able to complete formal residency programs | Formal certificate with the Ministry of Health and National Medical School | Didactic lectures, simulation, journal club, morbidity and mortality conference, skill sessions clinical supervision, and development and delivery of one lecture; learners comprised of physicians from multiple hospitals; international and national faculty | Attendance of 75%, 180 supervised clinical hours, written pre- and post-test, completed case and procedure log | Course free of charge; participants retained full salary; non-local participants provided food and housing; subsidized in-country expenses for visiting faculty | 6-month course; 96-hour didactic program conducted every other week; eight visiting faculty volunteering 3–4 weeks | Use of established residency resources; ACLS and PALS resources | 11/14 graduates still working in Emergency Departments one year later; average improvement of 15 points between pre- and post-test scores | Frequent turn-over of clinical supervisors; resource limitations at non-training sites; views of staff/culture of institution; lack of curriculum flexibility; varied baseline knowledge; language barrier |
| Stanley | To improve competence in assessment and management of emergent conditions | None | Scenario-based drills/training with whiteboard and reference cards; focus on ABCDE | Observed scenarios (OSCE) and feedback form; pre-assessment; 1–2-week post-assessment and 8-week assessment | Not described | Three sites; four days at each site (pre-assessment, training, post-assessment, 8-week assessment) with two identical sessions daily | Previously used local training tools and instructor experience | Assessment scores and self-reported confidence scores all improved after the intervention | Attendance low |
Table 5
Sample list of curricula and content resources.
| Organization | Resources | Website* |
|---|---|---|
| Global Health Emergency Medicine (GHEM) | Teaching modules | http://ghem.ca/modules/ |
| African Federation for Emergency Medicine (AFEM) | Curricula, lecture bank, ultrasound lecture bank | https://afem.africa/resources/ |
| World Health Organization (WHO) | Full short course | https://www.who.int/emergencycare/publications/Basic-Emergency-Care/en/ |
| International Student Association of Emergency Medicine (ISAEM) and the International Emergency Medicine Education Project (iEM) | Medical student resources | https://isaem.net/ https://iem-student.org |
| International Federation for Emergency Medicine | General guidelines; curricula outlines | https://www.ifem.cc/ |
| OPENPediatrics | Pediatric-specific resources | https://www.openpediatrics.org/ |
| Emergency Ultrasound Teaching | Ultrasound-specific resources | http://emergencyultrasoundteaching.com/ |
| Free, Open-Access Medical Education Resources | One list of general resources | https://rebelem.com/focused-foamed-the-learners-lens/ |
| American College of Emergency Physicians (ACEP) International Section | General resources from an EM organization | https://www.acep.org/how-we-serve/sections/international-emergency-medicine/free-educational-resources/ |
[i] * Accessed: May 2019; the authors do not specifically endorse any particular resource, nor do they verify the accuracy of the content listed at the sites above.
