The Shaukat Khanum Memorial Trust has existed since February 1990. The first Shaukat Khanum Memorial Cancer Hospital and Research Center (SKMCH&RC) opened for patients in Lahore on December 29, 1994. The operations of SKMCH&RC, Peshawar, commenced in December 2015. Two distinct centers with outpatient clinics and diagnostic facilities have been functioning in addition to these two hospitals: The Karachi Diagnostic Center, which has been in operation since 2010, and the Shaukat Khanum Diagnostic Center Liberty, which is situated in Lahore and has been operational since August 1, 2019. The Shaukat Khanum Diagnostic Center on Jail Road in Lahore opened to the public on December 17, 2003.
SKMCH&RC hospitals are associated with outpatient, inpatient, and diagnostic facilities. The cancer registry officers and medical coders facilitate cancer registration to ensure the quality, accuracy, and timeliness of the data reported. In the Cancer Registry and Clinical Data Management section, certified or experienced registry officers impart training to the staff. Junior staff members attend in-house, extensive, and formal training programs before they begin abstracting cases. They enhance their skills through training imparted after audit checks and online continuing educational programs.
The study aimed to present the distribution of cancer cases registered at SKMCH&RC over 28 years.
This study comprised patient information entered into the hospital-based cancer registry, which is an integral part of the Hospital Information System, over 28 years, from December 1994 to December 2022, after registration of the patients at the centers affiliated with the Trust. To present the aggregated findings, all these facilities are referred to as SKMCH&RC or the hospital.
This study did not involve an experiment. After the records were reviewed retrospectively, the anonymized results were generated. No individual patient consent or informing the patients was required. The SKMCH&RC Institutional Review Board (IRB), officially known as the “Institutional Review Board, SKMCH&RC,” reviewed the study and granted it an exempt status, eliminating the need for informed consent (Reference No. EX-01-11-23-02). The same IRB authorized the study (Reference No. EX-01-11-23-02). The OHRP lists the IRB as “IRB00005898 – Shaukat Khanum Mem Cancer Hosp”.
At SKMCH&RC, the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes,[1] replaced the ICD-9-CM codes, which had been in use until 2013. Brain and spinal cord tumors have been abstracted and included in the report since January 2004; before this, neoplasms with benign and uncertain behavior were excluded.
Cases were identified using the case-finding lists for inclusion in the registry under the guidelines established by the Surveillance Epidemiology and End Results (SEER) program.[2] Thereby, a search for reportable cases was conducted. Casefinding sources included documents on inpatient discharges, outpatient encounters, pathology or cytology reports, radiology, nuclear medicine, radiation therapy, chemotherapy outpatient, emergency assessment room, and pain clinic.[2]
The list of reportable cancers was modified at SKMCH&RC after including the following: all types of skin cancers (C44), prostatic intraepithelial carcinoma (PIN III-8148/2), carcinoma in situ of the cervix (CIN III-8077/2), systemic mastocytosis (D47.02), atypical chronic myeloid leukemia BCR/ABL-negative (C92.2), and chronic myeloid leukemia BCR/ABL-positive (C92.1).[3]
However, the following were excluded: Idiopathic hypereosinophilic syndrome (HES) (D72.110), lymphocytic variant HES [LHES (D72.111)], other HES (D72.118), HES unspecified (D72.119), cytologic evidence of malignancy on the smear of the anus (R85.614), cytologic evidence of malignancy on the smear of the cervix (R87.614), and cytologic evidence of malignancy on the smear of the vagina (R87.624).
In this study, the lower gastrointestinal (GI) tract included the colon, rectum, anal canal, and anus. After making changes to the list of cancers that needed to be reported, the results showed 119,486 cases of reportable cancers; however, other than the central nervous system tumors, which have been reportable since 2004, 8443 tumors with the behavior codes/0 (benign tumors) or/1 (uncertain whether benign or malignant, borderline malignancy, low malignant potential, and uncertain malignant potential) were excluded (4). Both/2 (carcinoma in situ, intraepithelial, non-infiltrating, and non-invasive), and/3 (malignant and primary site) neoplasms were included.[4]
For the most frequently registered cancers, the ICD-10-CM codes,[1] corresponding to the cancer type in adults, are shown in parentheses: breast (C50, D05), ovary and uterine adnexa (C56, C57), lip and oral cavity (C00-C08, D00.00–D00.07), cervix uteri (C53, D06), colon, rectum, anal canal, and anus (C18-C21, D01.0–D01.49, C7A.020–C7A.029, and C49.A4–C49.A5), corpus uteri and uterus (C54–C55, C58, D07.0), esophagus (C15, D00.1), thyroid (C73), non-Hodgkin lymphoma (NHL) (C82–C86, C88.4), melanoma and other skin cancers (C43– C44, D03-D04), prostate (C61, D07.5), liver and intrahepatic bile ducts (C22), trachea, bronchus, and lung (C33–C34, D02.1–D02.22, C7A.090), urinary bladder (C67, D09.0), leukemia (C91–C95), brain (C70–C71), and Hodgkin lymphoma (C81).[1]
For the commonly registered cancers in children, coding based on the International Classification of Diseases for Oncology, third edition (ICD-O-3), was used: Hodgkin lymphoma (9650–9667), acute lymphoblastic leukemia (ALL) (9835–9837), NHL (9591, 9670–9729), osteosarcoma (9180–9195), retinoblastoma (9510–9513), Ewing’s sarcoma (primitive neuroectodermal tumor (PNET (9260, 9364)), germ cell tumor (9060–9090), nephroblastoma (8960), glioma (9380–9480), and rhabdomyosarcoma (8900–8921).[5]
IBM SPSS Statistics 20 and Excel Version 2401 from Microsoft 365 were used for the data analysis. The top ten malignancies were shown after the cases were divided into two age groups: adults above the age of 18 years and children under or equal to 18 years.
In 28 years, from December 29, 1994, to December 31, 2022, 119,486 malignancies were registered at SKMCH&RC. Of those, 58,082 (48.6%) were seen in males and 61,404 (51.4%) in females. 11,943 tumors (10.0%) were identified in children, compared to 107,543 tumors (90.0%) in adults. Table 1 displays the stratification of malignant cases by age group (adults and children), whereas Figure 1 shows the counts of malignancies in males and females according to the 5-year age group.
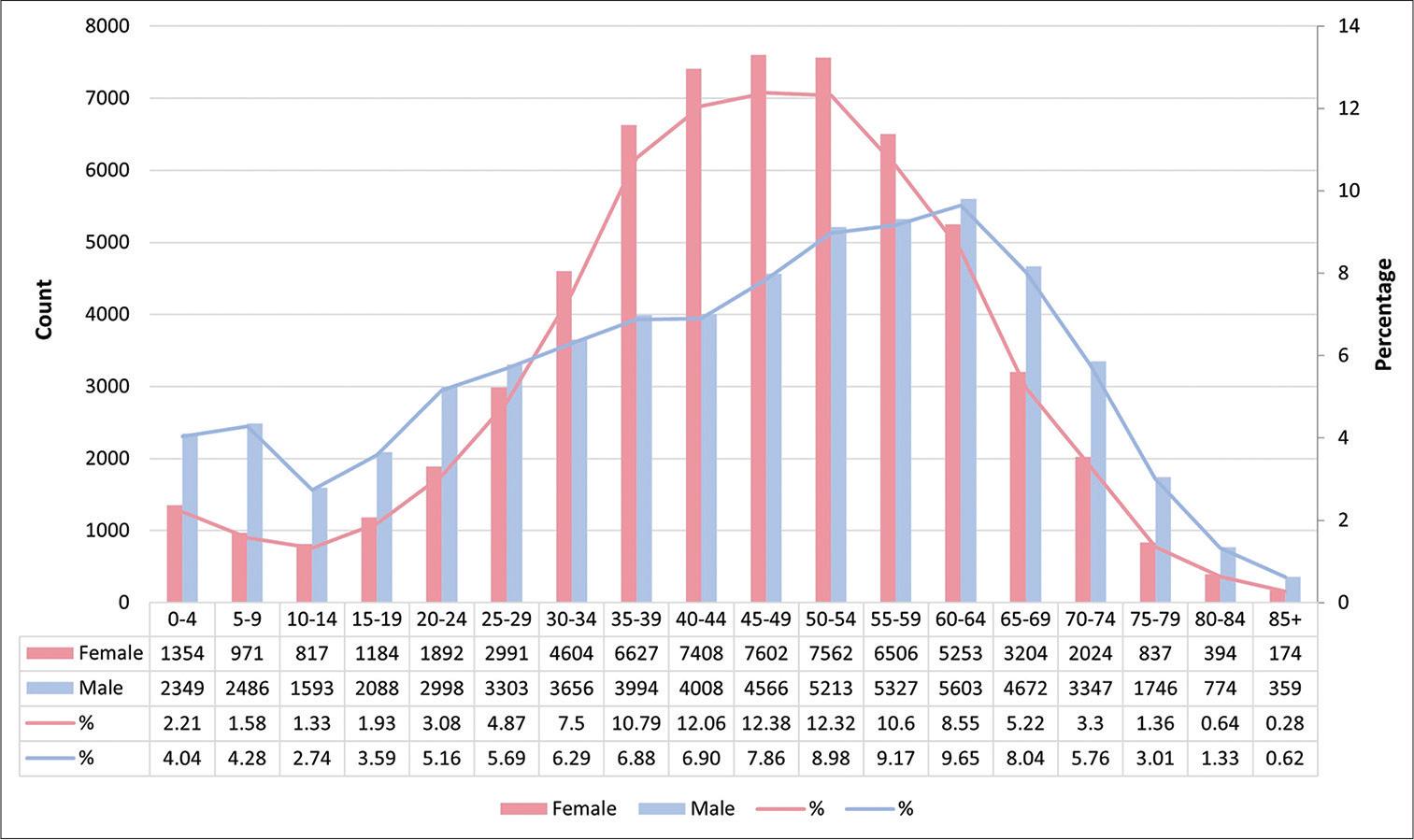
Distribution of malignancies by sex (N = 61,404 in females and N = 58,082 in males) and 5-year age group, SKMCH&RC, December 1994 to December 2022
Distribution of neoplasms by age group, SKMCH&RC, December 1994 to December 2022
| Behavior | Age group | Registered patients (117,174) | Reported neoplasms (119,486) |
|---|---|---|---|
| Malignant | Adults | 105,311 | 107,543 |
| Children | 11,863 | 11,943 | |
| Total | 117,174 | 119,486 |
The difference in the number of registered patients and reported neoplasms was attributed to multiple malignancies diagnosed in 2,312 patients.
Malignancies with behavior codes/2 and/3 were included. Benign CNS tumors with behavior codes/0 and/1 were also included. These can be life-threatening if located in a vital area
Table 2 shows that the province of Punjab accounted for 66.8% of the 119,486 malignancies. Khyber Pakhtunkhwa, which comprises the Federally Administered Tribal Areas (FATA) and the Northwest Frontier Province (NWFP), accounted for 20.5%. On May 28, 2018, FATA became a part of Khyber Pakhtunkhwa province. NWFP was renamed “Khyber Pakhtunkhwa” in 2010.[6]
Distribution of malignancies (N=119,486) according to the geographic area of residence of the patients, SKMCH&RC, December 1994 to December 2022
| Region | Count | Percentage |
|---|---|---|
| Punjab | 79,863 | 66.8 |
| Khyber Pakhtunkhwa | 24,458 | 20.5 |
| Sindh | 3,856 | 3.2 |
| Balochistan | 1,731 | 1.4 |
| Federal capital | 1,339 | 1.1 |
| Gilgit-Baltistan | 223 | 0.2 |
| Unoccupied Jammu and Kashmir | 1,144 | 1 |
| Afghanistan | 6,678 | 5.6 |
| Other countries | 49 | 0.04 |
| Not defined | 145 | 0.1 |
Given that the oldest SKMCH&RC hospital is in Punjab’s provincial capital, Lahore, and that this province is home to 50% of the nation’s population, it is understandable why most patients represent Punjab.
The top ten malignancies registered at the hospital during the past 28 years were categorized according to sex and age group. Neoplasms of the breast, lower GI tract, lip and oral cavity, leukemia, and NHL were the most frequent malignancies registered at the hospital, according to the data on all age groups and both sexes combined (Figure 2).
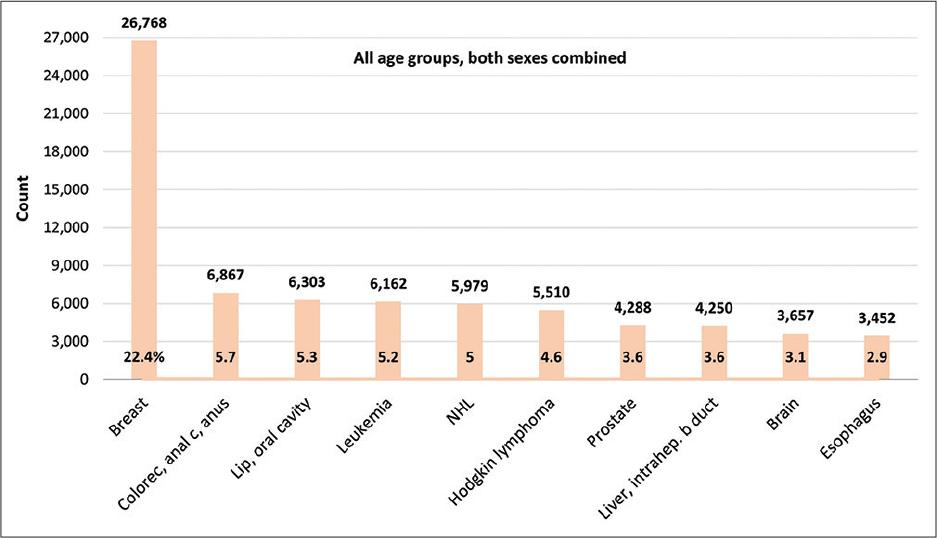
Top ten malignancies among all age groups, both sexes combined (N = 119,486), SKMCH&RC, December 1994 to December 2022 (NHL is an acronym for non-Hodgkin lymphoma)
Neoplasms of the breast, ovary and uterine adnexa, lip and oral cavity, cervix, and lower GI tract were frequently diagnosed among adult females. In contrast, malignancies of the lower GI, prostate, lip and oral cavity (excluding nasopharyngeal cancers), NHL, and liver and intrahepatic bile ducts were commonly seen in adult males (Figure 3). Table 3 displays the proportional distribution of cases in adult females and males.
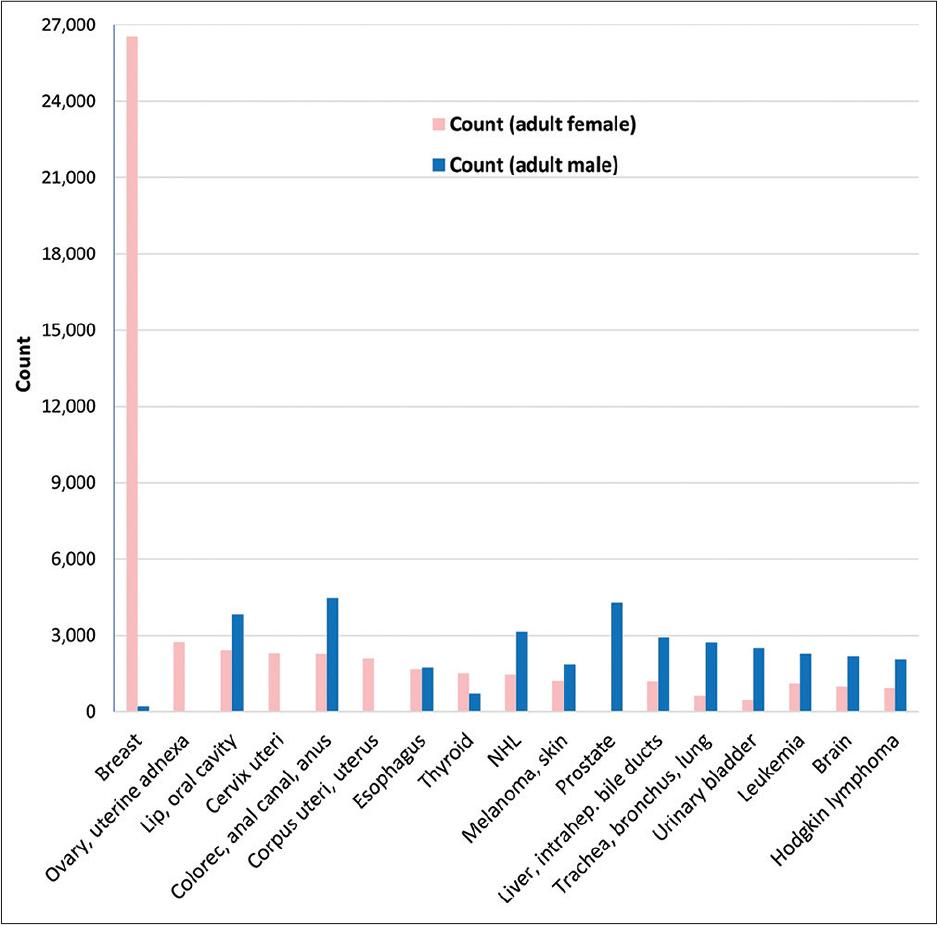
Top ten malignancies among adult (>18 years) females (N = 57,397) and males (N = 50,146), SKMCH&RC, December 1994 to December 2022 (NHL is an acronym for non-Hodgkin lymphoma and skin cancers include both melanoma and non-melanoma)
Top ten malignancies among adults (>18 years), by sex (N=119,486), SKMCH&RC, December 1994 to December 2022
| Cancer in adults | Female cancer count: 57,397 | % | Male cancer count: 50,146 | % |
|---|---|---|---|---|
| Breast | 26,558 | 46.3 | 202 | 0.4 |
| Ovary, uterine adnexa | 2,765 | 4.8 | 0 | 0 |
| Lip, oral cavity | 2,412 | 4.2 | 3,840 | 7.7 |
| Cervix uteri | 2,291 | 4 | 0 | 0 |
| Colon, rectum, anal canal, anus | 2,274 | 4 | 4,503 | 9 |
| Corpus uteri, uterus | 2,101 | 3.7 | 0 | 0 |
| Esophagus | 1,688 | 2.9 | 1,753 | 3.5 |
| Thyroid | 1,548 | 2.7 | 735 | 1.5 |
| NHL | 1,458 | 2.5 | 3,142 | 6.3 |
| Melanoma, non-melanoma skin ca | 1,213 | 2.1 | 1,870 | 3.7 |
| Prostate | 0 | 0 | 4,287 | 8.5 |
| Liver, intrahepatic bile ducts | 1,197 | 2.1 | 2,936 | 5.9 |
| Trachea, bronchus, lung | 648 | 1.1 | 2,730 | 5.4 |
| Urinary bladder | 460 | 0.8 | 2,520 | 5 |
| Leukemia | 1,112 | 1.9 | 2,272 | 4.5 |
| Brain | 1,010 | 1.8 | 2,183 | 4.4 |
| Hodgkin lymphoma | 951 | 1.7 | 2,064 | 4.1 |
In children, the most frequent cancers were Hodgkin lymphoma, ALL, and NHL (Figure 4).
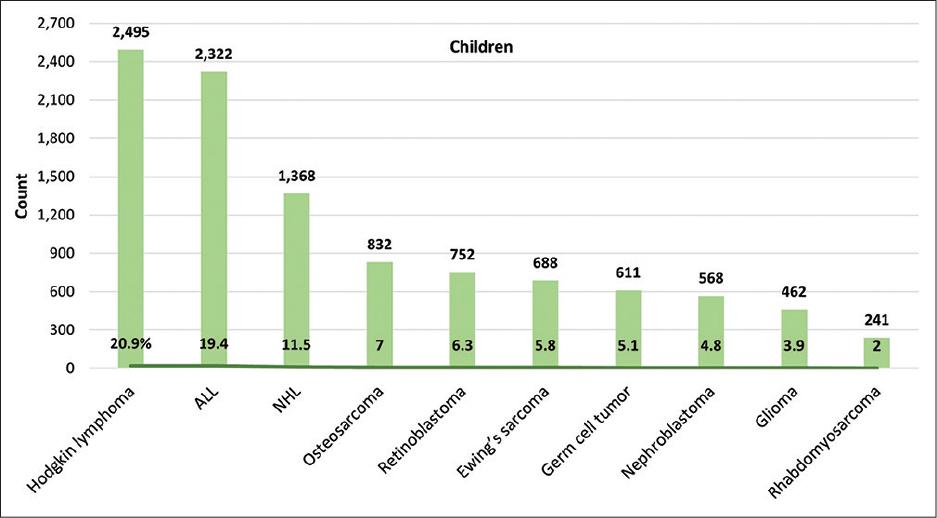
Top ten malignancies in children (≤18 years), both sexes combined (N = 11,943), SKMCH&RC, December 1994 to December 2022 (ALL is an acronym for acute lymphoblastic leukemia and NHL is an acronym for non-Hodgkin lymphoma)
It is the first of its kind, an extensive report on hospital-based cancer registration over 28 years from any hospital in Pakistan. Although patient triage determined by hospital policy impacts cancer registration, the information available is invaluable as the foundation for research studies conducted at SKMCH&RC, for multicentered studies and clinical trials, and for reporting them to a regional registry. Nevertheless, there are not many online publications on hospital-based cancer registration in Pakistan, and the studies available are limited in scope. These reports represent the oncology centers of the Pakistan Atomic Energy Commission (2018–2019: N = 79,254 and 2015– 2017: N = 102,022),[7,8] Shifa International Hospital (2018–2020: N = 8,898),[9] and the pathology-based Dow Diagnostic Research and Reference Laboratory (2010–2019: N = 22,858).[10] No reports were available on the institutional registries representing the main stakeholders such as the Aga Khan University Hospital, the Indus Hospital, the Pakistan Institute of Medical Sciences, the Cancer Care Hospital, the Armed Forces Institute of Pathology, or any other government or private hospital.[11]
The small number of hospital-based registries currently in operation and the dearth of publications on institutional cancer registration are concerning. What is more problematic, though, is the misrepresentation and distortion of the SKMCH&RC findings that are readily available on the Internet.[12] The results from SKMCH&RC have been distorted in a paper published by non-SKMCH&RC employees.[13] The authors falsely claim that these results represent the population of Pakistan, whereas, in reality, they merely represent a hospital-based registry. The paper indicates that approximately 4100 new cases are diagnosed in Pakistan annually, in a population of two hundred million.[13] This figure is incorrect. Globocan has estimated that more than 150,000 new cases were diagnosed in 1 year in Pakistan.[14] For readers, legislators, health-care personnel, and the public, the content included in the paper is flawed and misleading.[13]
There is an urgent need to train individuals in cancer registration and medical coding and establish hospital-based registries in each hospital. Maintaining accurate records is beneficial for the nation’s population-based cancer surveillance system.