Fig. 1
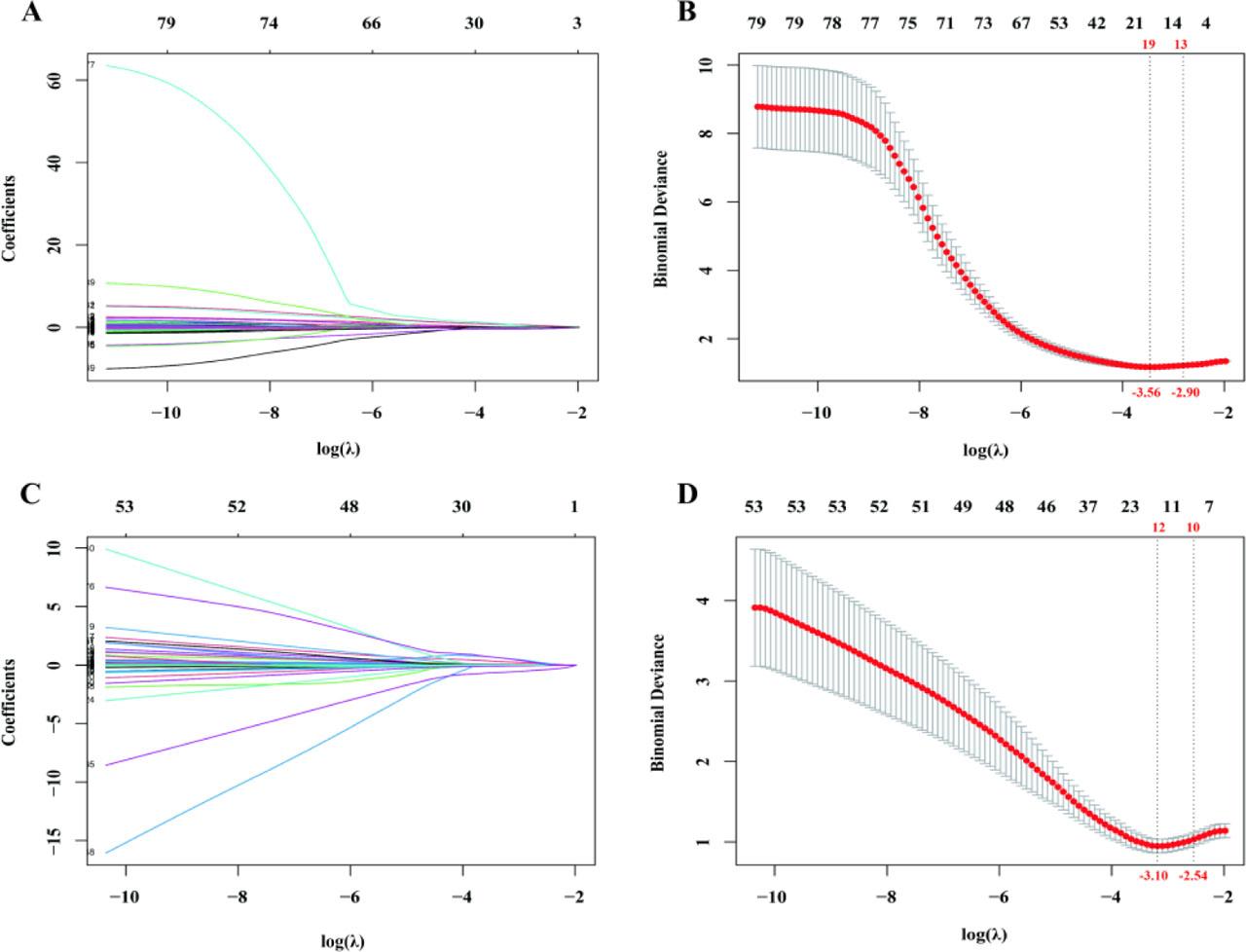
Fig. 2

Fig. 3
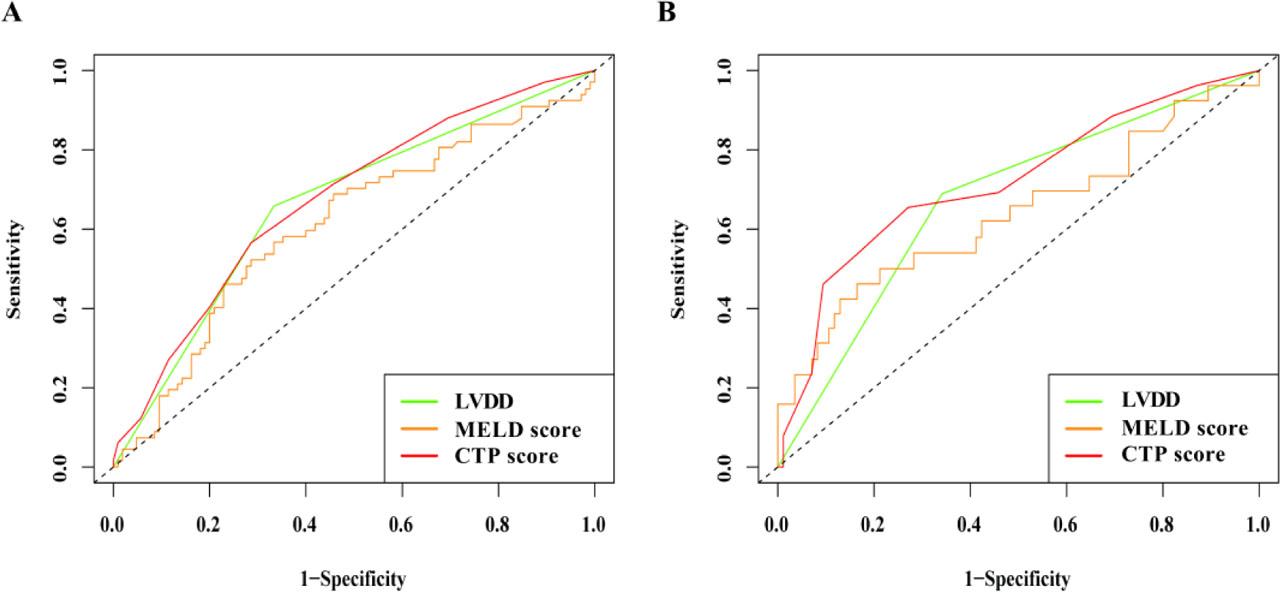
Fig. 4

Univariate and multivariate Cox regression of 1-year mortality risk
| Participants | Factors | Univariate Cox | Multivariate Cox | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | ||
| Total | BMI | 0.917 | 0.851–0.987 | 0.021 | 0.876 | 0.808–0.950 | 0.001 |
| Hepatic malignancy | 2.579 | 1.635–4.069 | <0.001 | 1.863 | 1.107–3.141 | 0.019 | |
| MAD | 1.069 | 0.999–1.155 | 0.088 | ||||
| RVOTD | 1.087 | 1.039–1.137 | <0.001 | 1.077 | 1.018–1.139 | 0.008 | |
| LVDD | 2.447 | 1.522–3.933 | <0.001 | 2.109 | 1.279–3.478 | 0.003 | |
| WBC | 1.114 | 1.065–1.165 | <0.001 | ||||
| PLT | 1.004 | 1.002–1.006 | <0.001 | 1.003 | 1.0002–1.0062 | 0.035 | |
| Na | 0.886 | 0.839–0.936 | <0.001 | ||||
| DBIL | 1.004 | 1.001–1.007 | 0.001 | ||||
| GGT | 1.001 | 1.001–1.002 | 0.007 | ||||
| ALP | 1.002 | 1.001–1.003 | <0.001 | ||||
| CHE | 0.352 | 0.213–0.580 | <0.001 | ||||
| INR | 4.713 | 2.197–10.110 | <0.001 | 7.031 | 2.504–19.748 | <0.001 | |
| Without hepatic malignancy | Etiology of cirrhosis | 3.874 | 1.482–10.129 | 0.006 | |||
| viral hepatitis | 1 | - | - | ||||
| alcohol | 2.169 | 0.929–5.064 | 0.074 | ||||
| virus+alcohol | 0.423 | 0.056–3.106 | 0.398 | ||||
| others | 3.150 | 1.332–7.448 | 0.009 | ||||
| RVOTD | 1.061 | 1.017–1.107 | 0.006 | ||||
| LVDD | 3.020 | 1.441–6.332 | 0.003 | 2.351 | 1.040–5.313 | 0.040 | |
| RDW | 1.215 | 1.063–1.388 | 0.004 | ||||
| CO2 | 0.886 | 0.828–0.948 | <0.001 | 0.840 | 0.764–0.922 | <0.001 | |
| CREA | 1.003 | 1.001–1.004 | 0.003 | ||||
| TBIL | 1.005 | 1.002–1.008 | <0.001 | 1.007 | 1.003–1.011 | 0.001 | |
| CHE | 0.248 | 0.114–0.540 | <0.001 | ||||
| INR | 10.400 | 2.963–36.510 | <0.001 | ||||
| CTP score | 1.291 | 1.116–1.494 | <0.001 | ||||
Demographic, basic clinical characteristics, and baseline information
| Factors | Total (n = 194) | Non-LVDD group (n = 102) | LVDD group (n = 92) | t/Z/χ2 | P | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, M(P25, P75) years | 55.0(47.0, 60.2) | 49.0(43.0, 57.3) | 59.0(53.2, 65.7) | −5.936 | <0.001 | |
| Male sex, n(%) | 135(69.6) | 77(75.5) | 58(63) | 3.541 | 0.060 | |
| Han ethnicity, n(%) | 177(91.2) | 96(94.1) | 81(88) | 2.232 | 0.135 | |
| BMI, M(P25, P75) kg/cm2 | 22.0(20.3, 24.3) | 22.0(20.0, 23.9) | 22.4(20.4, 24.6) | −0.807 | 0.420 | |
| Smoking history, n(%) | ||||||
| Yes | 103(53.1) | 60(58.9) | 43(46.7) | 3.204 | 0.202 | |
| No | 84(43.3) | 38(37.3) | 46(50) | |||
| Quit | 7(3.6) | 4(3.9) | 3(3.3) | |||
| Alcohol consumption, n(%) | ||||||
| Yes | 82(42.3) | 48(47.1) | 34(37) | 2.849 | 0.241 | |
| No | 91(46.9) | 42(41.2) | 49(53.3) | |||
| Quit | 21(10.8) | 12(11.8) | 9(9.8) | |||
| Family history of hepatic malignant, n(%) | 22(11.3) | 13(12.7) | 9(9.8) | 0.422 | 0.516 | |
| Basic clinical information | ||||||
| Etiology of cirrhosis, n(%) | 7.603 | 0.055 | ||||
| Viral hepatitis | 144(74.2) | 83(81.4) | 61(66.2) | |||
| Alcohol | 17(8.8) | 6(5.9) | 11(12) | |||
| Virus + Alcohol | 18(9.3) | 9(8.8) | 9(9.8) | |||
| Others | 15(7.7) | 4(3.9) | 11(12) | |||
| Hepatic malignant, n(%) | 124(63.9) | 31(30.4) | 39(42.4) | 3.020 | 0.082 | |
| EGVB, n(%) | 22(11.3) | 12(11.8) | 10(10.9) | 0.039 | 0.844 | |
| Systolic blood pressure, M(P25, P75) mmHg | 115.0(104.0, 128.0) | 115.0(101.7, 122.0) | 117.0(105.0, 134.0) | −1.752 | 0.080 | |
| Diastolic blood pressure, M(P25, P75) mmHg | 72.0(66.0, 82.0) | 71.0(65.0, 78.0) | 74.0(68.0, 85.0) | −2.066 | 0.039 | |
| Heart rate, M(P25, P75) bpm | 82.0(72.0, 92.0) | 80.0(72.0, 91.0) | 83.5(71.3, 92.0) | −0.334 | 0.738. | |
| Liver function | ||||||
| CTP, M(P25, P75) scores | 9.0(8.0, 11.0) | 9.0(7.0, 11.0) | 9.0(8.0, 11.0) | −0.889 | 0.374 | |
| MELD, M(P25, P75) scores | 12.6(10.0, 17.0) | 12.4(10.1, 16.4) | 12.6(9.5, 15.7) | −0.517 | 0.605 | |
| Laboratory findings | ||||||
| TBIL, M(P25, P75) μmol/L | 31.9(18.2, 64.5) | 32.2(18.0, 77.8) | 31.6(18.2, 58.1) | −0.142 | 0.887 | |
| DBIL, M(P25, P75) μmol/L | 14.4(7.8, 36.0) | 13.3(7.5, 44.6) | 14.6(7.8, 28.8) | −0.187 | 0.852 | |
| ALT, M(P25, P75) U/L | 35.0(23.0, 75.0) | 37.0(24.8, 72.3) | 32.5(23.0, 78.0) | −0.940 | 0.347 | |
| AST, M(P25, P75) U/L | 54.0(37.8, 120.0) | 58.5(37.0, 109.75) | 51.0(38.0, 132.7) | −0069 | 0.945 | |
| GGT, M(P25, P75) U/L | 96.0(40.8, 169.6) | 80.5(38.7, 156.3) | 103.5(46.4, 162.7) | −1.247 | 0.212 | |
| ALP, M(P25, P75) U/L | 142.0(102.8, 201.2) | 142.0(105.2, 195.0) | 153(100.0, 217.0) | −0.513 | 0.608 | |
| TP, M(P25, P75) g/L | 61.6(57.5, 67.4) | 61.8(57.0, 67.1) | 61.3(57.7, 68.2) | −0.133 | 0.894 | |
| PALB, M(P25, P75) g/L | 76.1(49.1, 110.3) | 77.0(46.4, 105.4) | 71.1(52.1, 112.8) | −0.428 | 0.669 | |
| ALB, M(P25, P75) g/L | 29.5(25.7, 33.3) | 30.2(27.3, 35.0) | 28.2(24.8, 31.8) | −2.596 | 0.009 | |
| GLOB, M(P25, P75) g/L | 31.2(27.2, 36.7) | 30.4(27.0, 35.5) | 32.1(28.0, 37.8) | −1.629 | 0.103 | |
| CHE, M(P25, P75) U/L | 2978.0(2136.8, 4008.3) | 2978.0(2214.0, 3999.0) | 2886.5(2089.7, 4253.5) | −0.636 | 0.525 | |
| PT, M(P25, P75) sec | 16.6(15.3, 18.4) | 16.6(15.3, 18.4) | 16.6(15.4, 18.1) | −0.236 | 0.814 | |
| PTA, M(P25, P75) % | 59.8(68.0, 50.7) | 59.7(50.1, 69.9) | 59.8(51.0, 68.0) | −0.008 | 0.994 | |
| INR, M(P25, P75) | 1.4(1.3, 1.6) | 1.4(1.2, 1.6) | 1.4(1.2, 1.5) | −0.003 | 0.998 | |
| WBC, M(P25, P75) ×109/L | 4.4(3.1, 7.3) | 4.1(2.7, 7.9) | 4.5(3.4, 7.4) | −1.694 | 0.092 | |
| RBC, (x̅±s) ×1012/L | 3.6±0.8 | 3.6±0.7 | 3.5±0.8 | 0.556 | 0.579 | |
| HGB, M(P25, P75) g/L | 115.0(97.8, 133.0) | 117.5(95.0, 132.3) | 115.0(99.3, 133.0) | 0.080 | 0.937 | |
| PLT, M(P25, P75) ×109/L | 89.5(59.7, 141.5) | 83.5(53.7, 139.0) | 100.0(71.2, 142.5) | −1.580 | 0.114 | |
| K, (x̅±s) mmol/L | 3.7±0.5 | 3.7±0.5 | 3.8±0.5 | −2.053 | 0.041 | |
| Na, M(P25, P75) mmol/L | 138.9(136.1, 141.1) | 138.9(136.5, 141.2) | 108.9(105.8, 140.8) | −0.690 | 0.490 | |
| Ca, (x̅±s) mmol/L | 2.1±0.2 | 2.0±0.1 | 2.09±0.2 | −0.752 | 0.453 | |
| CL, M(P25, P75) mmol/L | 106.9(136.1, 141.1) | 106.9(103.9, 109.4) | 106.5(103.1, 109.4) | −0.491 | 0.630 | |
| CO2, M(P25, P75) mmol/L | 23.3(21.5, 25.2) | 23.2(21.7, 24.9) | 23.4(21.3, 25.2) | −0.122 | 0.903 | |
| BUN, M(P25, P75) mmol/L | 4.8(3.8, 7.1) | 4.5(3.6, 6.5) | 5.2(4.1, 8.5) | −2.768 | 0.006 | |
| Crea, M(P25, P75) μmol/L | 61.5(52.0, 74.0) | 60.0(49.0, 73.0) | 63.5(53.0, 80.7) | −1.515 | 0.130 | |
| UA, M(P25, P75) μmol/L | 295.0(244.0, 375.2) | 290.5(243.7, 355.2) | 301(242.2, 406.0) | −0.946 | 0.344 | |
| FPG, M(P25, P75) mmol/L | 5.6(4.9, 7.4) | 5.5(4.8, 7.1) | 5.7(5.0, 8.2) | −1.375 | 0.169 | |
| TG, M(P25, P75) mmol/L | 0.8(0.6, 1.3) | 0.8(0.5, 1.2) | 0.8(0.6, 1.2) | −1.204 | 0.229 | |
| CHOL, M(P25, P75) mmol/L | 3.2(2.6, 3.9) | 3.1(2.5, 3.5) | 3.1(2.7, 4.2) | −2.427 | 0.015 | |
| HDL-C, M(P25, P75) mmol/L | 0.8(0.5, 1.1) | 0.7(0.4, 1.0) | 0.7(0.5, 1.0) | −0.552 | 0.581 | |
| LDL-C, M(P25, P75) mmol/L | 1.9(1.4, 2.5) | 1.8(1.3, 2.2) | 2.0(1.4, 2.8) | −2.957 | 0.003 | |
| CEA, M(P25, P75) μg/L | 3.2(2.1, 4.8) | 3.0(2.0, 4.5) | 3.6(2.3, 5.0) | −2.300 | 0.021 | |
| AFP, M(P25, P75) μg/L | 6.4(3.1, 66.7) | 6.3(3.2, 38.9) | 6.8(2.8, 100.4) | −0.391 | 0.696 | |
| CA125, M(P25, P75) U/mL | 107.5(31.5, 276.5) | 76.8(27.9, 228.2) | 152.9(40.9, 442.8) | −2.944 | 0.003 | |
| CA199, M(P25, P75) U/mL | 31.8(17.4, 68.5) | 31.5(16.3, 72.9) | 34.0(18.3, 67.2) | −0.210 | 0.834 | |
| LYMP, M(P25, P75) ×109/L | 0.9(0.6, 1.3) | 0.9(0.5, 1.2) | 0.9(0.5, 1.2) | −0.344 | 0.730 | |
| HCT, (x̅±s) % | 33.0±7.6 | 33.0±7.1 | 33.0±8.1 | 0.013 | 0.990 | |
| RDW, M(P25, P75) fL | 15.7(14.4, 17.0) | 15.7(14.4, 17.2) | 15.3(14.2, 16.9) | −0.613 | 0.540 | |
Cardiac Parameters of TTE [M(P25, P75)]
| Parameters of TTE | Total (n = 194) | Non-LVDD group (n = 102) | LVDD group (n = 92) | t/Z/χ2 | P |
|---|---|---|---|---|---|
| Aortic Valve Ring Internal Diameter, mm | 23.0(22.0, 25.0) | 23.0(22.0, 25.0) | 24.0(21.2, 25.7) | −1.382 | 0.173 |
| Ascending Aorta Internal Diameter, mm | 25.0(23.0, 27.0) | 25.0(23.0, 26.0) | 25.5(23.0, 28.0) | −1.947 | 0.052 |
| Mitral annulus diameter (MAD), mm | 20.0(18.0, 22.0) | 20.0(18.0, 22.0) | 21.0(19.0, 22.0) | −0.897 | 0.370 |
| Left Cardiac Chamber Diameter (LCD), mm | 28.0(26.0, 31.0) | 28.0(25.0, 31.0) | 28.0(26.0, 31.0) | −0.435 | 0.663 |
| Intrapericardial Pressure, mmHg | 42.0(38.7, 46.0) | 43.0(39.0, 46.0) | 42.0(39.0, 46.0) | −0.785 | 0.432 |
| Right Ventricular Diameter, mm | 20.0(18.0, 22.0) | 20.0(18.0, 22.0) | 20.0(18.0, 21.7) | −0.784 | 0.433 |
| Right Atrial Diameter, mm | 32.0(30.0, 35.0) | 32.5(30.0, 35.0) | 32.0(29.0, 34.0) | −1.255 | 0.210 |
| right ventricular outflow tract diameter (RVOTD), mm | 22.0(20.0, 24.0) | 22.0(20.0, 24.0) | 23.0(21.0, 25.0) | −1.573 | 0.116 |
| Interventricular Septum Thickness, mm | 9.0(8.0, 10.0) | 9.0(8.0, 10.0) | 9.0(8.0, 10.0) | −1.385 | 0.166 |
| Left Posterior Wall Thickness, mm | 9.0(8.0, 10.0) | 9.0(8.0, 10.0) | 9.0(8.0, 10.0) | −1.015 | 0.310 |
| end-diastolic volume (EDV), ml | 100.5(89.0, 117.2) | 102.0(89.0, 113.0) | 99.5(89.5, 121.0) | −0.320 | 0.749 |
| end-systolic volume (ESV), ml | 31.0(23.0, 40.0) | 31.0(24.0, 40.0) | 32.0(23.0, 42.5) | −0.238 | 0.812 |
| ejection fraction (EF), % | 68.0(64.0, 73.0) | 69.0(64.0, 72.2) | 67.0(63.0, 73.0) | −0.792 | 0.428 |
| Fractional Shortening, % | 38.0(34.0, 42.0) | 38.0(35.0, 42.0) | 37.0(34.0, 42.7) | −0.921 | 0.357 |
| stroke volume (SV), ml | 70.0(61.0, 80.0) | 69.5(60.0, 78.6) | 71.0(61.0, 80.0) | −0.353 | 0.724 |
| E-point Septal Separation, mm | 5.0(5.0, 6.0) | 5.0(5.0, 6.0) | 5.0(5.0, 6.0) | −1.358 | 0.174 |
| Pulmonary Artery Systolic Pressure, mmHg | 24.0(22.7, 28.0) | 24.0(21.0, 28.0) | 24.0(23.0, 28.0) | −0.116 | 0.908 |
| Tricuspid Regurgitation (peak velocity), m/s | 220.0(210.0, 246.0) | 220.0(200.0, 240.0) | 220.0(210.0, 240.0) | −0.275 | 0.783 |
| Pulmonary Artery Valve Forward Flow Rate, m/s | 113.0(96.7, 131.0) | 111.0(94.7, 130.0) | 113.0(100.0, 134.2) | −0.899 | 0.369 |
| Pulmonary Pulmonic Valve Forward Flow Rate, m/s | 90.0(80.0, 104.5) | 90.5(80.7, 102.2) | 90.0(80.0, 106.7) | −0.193 | 0.847 |
| E-wave/A-wave ratio (E/A) | 0.9(0.7, 1.3) | 1.2(1.0, 1.3) | 0.7(0.6, 0.8) | −9.412 | <0.001 |