Figure 1-

Figure 2-

Figure 3-
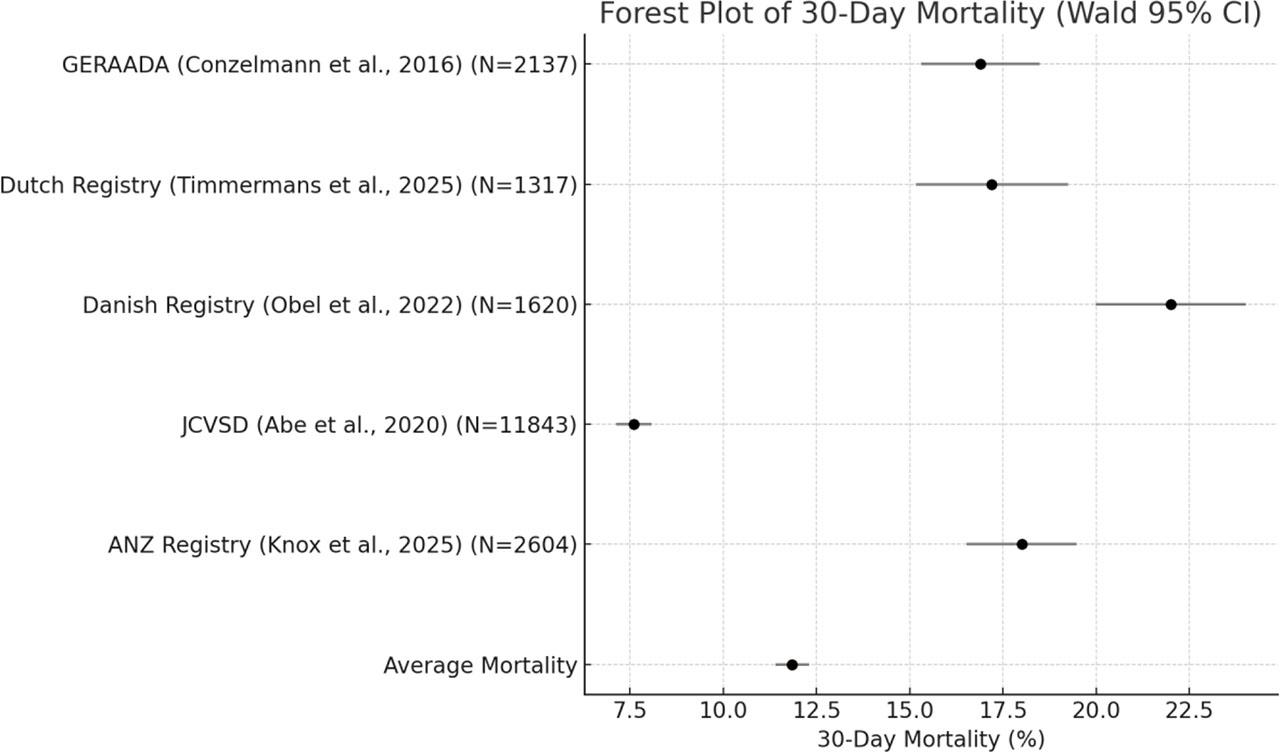
Figure 4-

Risk of Bias Assessment Across Included Registries
| Registry / Study | Clearly Defined Inclusion Criteria | Standardized Outcome Definitions | National or Multicentre Scope | Consecutive Case Inclusion | Completeness of Data Reported | Risk of Selection Bias |
|---|---|---|---|---|---|---|
| IRAD [4,6] | ✓ | ✓ | Multicentre | ✓ | ✓ | Moderate |
| GERAADA [7] | ✓ | ✓ | Multicentre | ✓ | ✓ | Low |
| ERTAAD [15] | ✓ | ✓ | Multicentre | ✓ | ✓ | Moderate |
| NORCAAD [8] | ✓ | ✓ | Multicentre | ✓ | ✓ | Moderate |
| STS Adult Cardiac Surgery Database [16] | ✓ | ✓ | National | ✓ | ✓ | Low |
| Australian and New Zealand SCTS [13] | ✓ | ✓ | National | ✓ | ✓ | Low |
| UK Aortic Group [12] | ✓ | ✓ | National | ✓ | ✓ | Low |
| Dutch Nationwide Registry [10] | ✓ | ✓ | National | ✓ | ✓ | Moderate |
| RENADA-RO [25] | ✓ | ✓ | National | ✓ | ✓ | Moderate |
| Danish National Registry [11] | ✓ | ✓ | National | ✓ | ✓ | Moderate |
| Nationwide German Diagnosis-Related Group Statistics [21] | ✓ | ✓ | National | ✗ | ✗ | Moderate |
| National Inpatient Sample [18] | ✓ | ✓ | National | ✗ | ✗ | Moderate |
| JRAD [22] | ✓ | ✓ | National | ✓ | ✓ | Low |
| JROAD-DPC [20] | ✓ | ✓ | National | ✓ | ✓ | Low |
| Japan Cardiovascular Surgery Database [17] | ✓ | ✓ | National | ✓ | ✓ | Low |
| China Registry [24] | ✓ | ✓ | National | ✓ | ✓ | Moderate |
| Sino-RAD [23] | ✓ | ✓ | National | ✓ | ✓ | Moderate |
Preoperative Risk Factors Reported Across Registries
| Study | Malperfusion | Cardiogenic shock | Reduced LVEF | PCS | Surgical Mortality |
|---|---|---|---|---|---|
| 30% | 15% | Not reported | 14.2% | in-hospital 21% |
| 33.6% | 57.8% | Not reported | Not reported | 30-day 16.9% |
|
| 43.6% | Not reported | 3.6% | in-hospital 18.2% |
| 33.9% | 21.4% | Not reported | Not reported | in-hospital 16% |
| Not reported | 30% | Not reported | 5.2% | in-hospital 17% |
| 36.5% | 14.5% | 20.4% | 6% | in-hospital 17.8% |
| Not reported | 15.8% | Not reported | Not included | operative 17.4% |
| Not reported | 15.5% | 28.1% | 1.2% | operative 9.5% |
| Not reported | 19.5% | Not reported | 16.3% | in-hospital 10.8% |
| 13.9% | 3.9% | Not reported | 4.2% | in-hospital 7.6% |
Mortality Outcomes and Demographic Profiles Across Major ATAAD Registries
| Study | N | Years | Age | Female Gender | Surgical Mortality | Medically Managed / Mortality |
|---|---|---|---|---|---|---|
| 5611 | 1996 – 2018 | 60.4± 14.1 | 32.9% | 48h 4.4% | 8.6 % / 23.7% |
| 2952 | 1996 – 2016 | in-hospital 25% → 18%* | 14% / 57% | ||
| 2477 | 2005 – 2021 | 63.5± 13.1 | 31% | in-hospital 18.2% | |
| 1159 | 2005 – 2014 | 61.5 ± 12.1 | 32.4% | in-hospital 16% | |
| 2137 | 2006 – 2010 | 60.5± 13.6 | 38.3% | 30-day 16.9% | |
| 14911 | 2006 – 2014 | 64 ± 9 | 35% | in-hospital 19.5% | |
| 1157 | 2006 – 2015 | 66 [57–74] | 35.4% | in-hospital 18% | 26% / 52% |
| 1620 | 1996 – 2016 | 63.5 ± 12.9 | 32.5% | 30-day 22% | |
| 1317 | 2018 – 2021 | 63.1 ± 11.8 | 41% | in-hospital 20.4% → 13.9% | |
| 30-day 17.2% | ||||||
| 501 | 2011 – 2022 | 60 ± 11 | 35% | in-hospital 29% | |
| 4203 | 2009 – 2018 | 64 [52–73] | 33.3% | in-hospital 17.8% | |
| 7805 | 2017 – 2018 | 60.0 ± 13.6 | 34% | in-hospital 15.3% | |
| 2982 | 2011 – 2012 | 59.7 ± 14.0 | 34.4% | operative 17.4% | |
| 11843 | 2008 – 2015 | 69 [60–77] | 51.8% | operative9.5% | |
| 30-day 7.6% | ||||||
| 1217 | 2011 – 2016 | 67.9 ± 13.1 | 52.1% | in-hospital 10.8% | 24.8% / 16.6% |
| 10131 | 2012 – 2015 | 69.8 ± 13.5 | 53.1% | in-hospital 11.8% | 33% / 49.7% |
| 1058 | 2018 – 2021 | 51.6 ± 11.7 | 23.8% | in-hospital 7.6% | |
| 1582 | 2012 – 2016 | 48.9 ± 11.1 | 21.7% | in-hospital 5.5% | 7.8% / not mentioned |
| 2604 | 2001 – 2021 | 65 [54–74] | 33% | 30-day 18% |
Methodological Characteristics of Contemporary ATAAD Registries
| Study | Region | Study Type | Data Source | Included |
|---|---|---|---|---|
| 14 countries | retrospective analysis of prospectively collected data | standardized case report forms (350 variables) | AAD – tertiary referral centres |
| 8 european countries | retrospective analysis of prospectively collected data | standardized case report forms | Surgically treated ATAAD – referral centres |
| Denmark, Finland, Iceland, Sweden | retrospective analysis of prospectively collected data | standardized case report forms (194 variables) | Surgically treated ATAAD – referral centres |
| Austria, Switzerland, Germany | prospective | standardized case report forms (90 parameters) | Surgically treated ATAAD |
| Germany | retrospective | ICD-10 codes & other codes | Surgically treated AAD – nationwide coverage |
| Denmark | retrospective | ICD-10 codes & other codes (linked 4 different registries) | Acute Aortic Dissection – nationwide coverage |
| Netherlands | retrospective analysis of prospectively collected data | standardized case report forms + mortality data via ICD-10 codes | Surgically treated AAD – nationwide coverage |
| Romania | retrospective analysis of prospectively collected data | standardized case report forms | ATAAD – referral centres |
| UK | retrospective analysis of prospectively collected data | standardized case report forms | Surgically treated ATAAD – referral centres |
| USA | retrospective | ICD-10 codes | Surgically treated ATAAD – nationwide coverage |
| USA | retrospective analysis of prospectively collected data | standardized case report forms (>260 variables) | Surgically treated ATAAD – nationwide coverage |
| Japan | retrospective analysis of prospectively collected data | standardized case report forms (255 variables) | Surgically treated AAD – nationwide coverage |
| Japan | retrospective | standardized case report forms (162 variables) | AAD – referral centres |
| Japan | retrospective | ICD-10 codes | AAD – nationwide coverage |
| China | retrospective analysis of prospectively collected data | standardized case report forms | Surgically treated ATAAD – referral centres |
| China | retrospective analysis of prospectively and retrospectively collected data | standardized case report forms | ATAAD and ATAIMH – referral centres |
| Australia and New Zealand | retrospective | standardized case report forms | Surgically treated ATAAD |