Figure 1.
PUMA score difference according to COPD severity
| COPD severity (GOLD) | P-value | |||
|---|---|---|---|---|
| 1 (n = 4) | 2 (n = 4) | 3 (n = 4) | ||
| PUMA score, mean ± SD | 7 ± 1 | 6 ± 1 | 7 ± 1 | P > 0.05 |
| <5, n (%) | 0 (0) | 0 (0) | 0 (0) | |
| ≥5, n (%) | 4 (100) | 4 (100) | 4 (100) | |
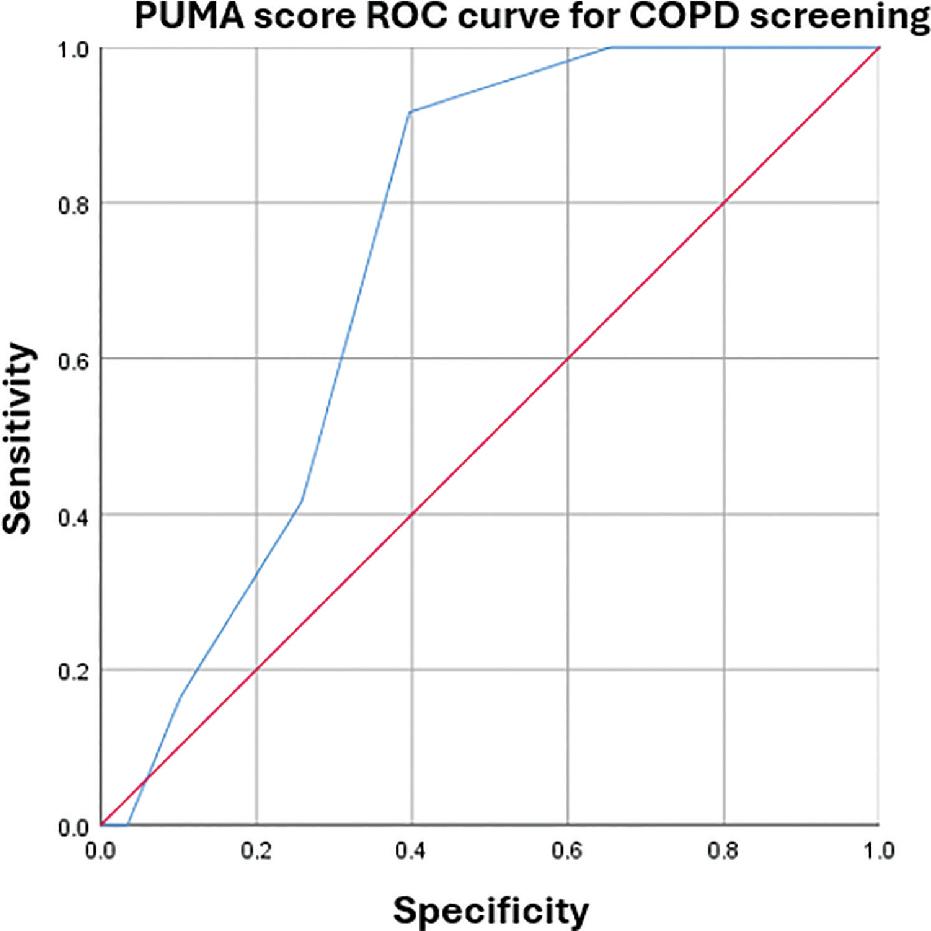
PUMA questionnaire performance on COPD diagnosis
| Category | Sensitivity (%) | Specificity (%) |
|---|---|---|
| ≥1 | 0 | 100 |
| ≥2 | 0 | 97 |
| ≥3 | 17 | 90 |
| ≥4 | 42 | 74 |
| ≥5 | 92 | 60 |
| ≥6 | 100 | 34 |
| ≥7 | 100 | 10 |
| ≥8 | 100 | 2 |
| ≥9 | 100 | 0 |
Baseline characteristics
| Characteristic | High-risk COPD (n = 70) | Mean ± SD/n (%) |
|---|---|---|
| Height (cm) | 163.3 ± 6.7 | |
| Weight (kg) | 64.5 ± 12.8 | |
| Gender | Female | 5 (7%) |
| Male | 65 (93%) | |
| Age | 40–49 years old | 11 (16%) |
| 50–59 years old | 17 (24%) | |
| ≥60 years old | 42 (60%) | |
| Smoking status | <20 pack-years | 14 (20%) |
| 20–30 pack-years | 25 (36%) | |
| >30 pack-years | 31 (44%) | |
| Dyspnoea | No | 24 (34%) |
| Yes | 46 (66%) | |
| Chronic phlegm | No | 36 (51%) |
| Yes | 34 (49%) | |
| Chronic cough | No | 32 (46%) |
| Yes | 38 (54%) | |
| Previous spirometry | No | 54 (77%) |
| Yes | 16 (23%) | |
| PUMA score | 2 | 1 (1%) |
| 3 | 5 (7%) | |
| 4 | 14 (20%) | |
| 5 | 16 (23%) | |
| 6 | 14 (20%) | |
| 7 | 12 (17%) | |
| 8 | 6 (9%) | |
| 9 | 2 (3%) | |
| Bronchodilator usage | No | 64 (91%) |
| Yes | 6 (9%) | |
| Comorbidity | No | 32 (46%) |
| Yes | 38 (54%) | |
| Hypertension | No | 49 (70%) |
| Yes | 21 (30%) | |
| Diabetes mellitus | No | 52 (74%) |
| Yes | 18 (26%) | |
| Tuberculosis | No | 68 (97%) |
| Yes | 2 (3%) | |
| Asthma | No | 67 (96%) |
| Yes | 3 (4%) | |
| No | 67 (96%) | |
| Congestive Heart failure | Yes | 3 (4%) |
| No | 67 (96%) | |
| Acute Coronary syndrome | Yes | 3 (4%) |
| Hepatitis B | No | 69 (99%) |
| Yes | 1 (1%) | |
| Hepatitis C | No | 69 (99%) |
| Yes | 1 (1%) |
Spirometry examination on high-risk COPD
| Variables | Mean ± SD/median (min–max) | N |
|---|---|---|
| VC (mL) | 2640.57 ± 754.36 | 70 |
| VC predicted | 3038 (338–6952) | 70 |
| VC% predicted | 85.6 (41.1–426) | 70 |
| Highest FVC pre-bronchodilator (mL) | 2565 ± 776 | 70 |
| FVC post-bronchodilator | 2616 ± 720 | 65 |
| FVC predicted (mL) | 3032 (1020–6952) | 70 |
| FVC% predicted | 84.1 (39.9–335.3) | 70 |
| FEV1 pre-bronchodilator | 1987 ± 732 | 70 |
| FEV1 predicted | 2244 (211–5902) | 70 |
| FEV1 post-bronchodilator | 2032 ± 696 | 65 |
| % FEV1 pre-bronchodilator | 87.8 (33.6–393.4) | 70 |
| % FEV1 post-bronchodilator | 95 (39–483) | 65 |
| FEV1/FVC pre-bronchodilator | 80.4 (44.9–95.7) | 70 |
| FEV1/FVC post-bronchodilator | 81 (44–99) | 66 |
| Highest PEF | 6.06 ± 2.3 | 70 |
| PFE post-bronchodilator | 6 ± 2 | 65 |
| FEV1 change (%) | 4 (0–27) | 65 |
| FEV1 change (mL) | 80 (0–430) | 65 |