The ongoing war in Ukraine has precipitated a profound humanitarian crisis, with millions of individuals displaced and exposed to violence, loss, and uncertainty (United Nations High Commissioner for Refugees [UNHCR], 2023). These experiences have significantly impacted the mental health and psychosocial well-being of affected populations, contributing to elevated rates of anxiety, depression, and post-traumatic stress disorder (PTSD) (Hino et al., 2023; Roberts et al., 2019). In response, mental health and psychosocial support (MHPSS) has emerged as a critical component of humanitarian interventions, which aims to address both the psychological and social dimensions of well-being (Inter-Agency Standing Committee [IASC], 2007).
MHPSS encompasses a wide range of activities designed to protect or promote psychosocial well-being and/or prevent or treat mental conditions (IASC, 2007). Effective MHPSS systems rely on a layered model of complementary interventions, ranging from the integration of social considerations in basic services and security (layer 1), to strengthening community and family supports (layer 2), to delivering focused support (layer 3) and specialized clinical care (layer 4) (IASC, 2007). Central to the effectiveness of MHPSS is the concept of social support, which plays a pivotal role in buffering the adverse effects of stress and fostering resilience (Cohen & Wills, 1985). Social support, defined as the perception or experience of being cared for, esteemed, and part of a network of mutual obligations (Cobb, 1976), is particularly crucial in conflict settings where traditional support systems may be disrupted (Hertog, 2024).
MHPSS coordination is a critical, multisectoral function within humanitarian responses, ensuring that diverse actors across health, protection, education, and other sectors work collaboratively to meet the mental health and psychosocial needs of affected populations. Core coordination actions include maintaining an inclusive and functional Technical Working Group (TWG), managing and sharing information, establishing referral pathways and stakeholder linkages, building the capacity of local and non-specialist actors, conducting joint monitoring and evaluation, promoting long-term sustainability of services, and advocacy (IASC, 2022).
In Ukraine, the coordination of MHPSS efforts has been led by the MHPSS TWG, a collaborative platform involving UN entities, international and local non-governmental organizations (NGOs) (ReliefWeb, 2024). This coordination is essential to ensure that interventions are aligned, resources efficiently allocated, and services are accessible to those in need (IASC, 2022). However, challenges such as inconsistent funding, stigma, and burnout among service providers persist, underscoring the need for a deeper understanding of coordination mechanisms (Harrison et al., 2021; Kang et al., 2024; Vus et al. 2024).
This study aims to bridge the gap between theory and practice in MHPSS coordination. By visualizing complex coordination dynamics and mental health data, the article seeks to make the intricacies of MHPSS more accessible to a broader non-specialist audience, including policymakers and humanitarian practitioners. Furthermore, the focus on Ukraine provides a timely case study, given the ongoing conflict and the global attention on mental health in crisis settings (World Health Organization [WHO], 2023).
In addition, the article explores how MHPSS coordination frameworks are operationalized in Ukraine's conflict-affected settings, with a particular focus on their role in enhancing social support and psychological well-being. By offering both theoretical reflection and practical insights, this research aims to contribute to more effective, locally grounded, and sustainable MHPSS interventions in Ukraine and other crisis-affected regions.
Building on the theoretical foundations outlined earlier, this section explores the practical implementation of MHPSS coordination in Ukraine amidst its protracted conflict. Since the onset of hostilities in 2014, and their escalation in 2022, Ukraine has faced unprecedented challenges in delivering MHPSS to millions of affected individuals, including internally displaced persons (IDPs), veterans, and civilians in conflict zones. This section analyzes the mechanisms, actors, and challenges involved in coordinating MHPSS, drawing on empirical data and reports from humanitarian agencies.
MHPSS coordination in Ukraine operates within a complex humanitarian system, guided by the IASC framework and localized through national and sub-national TWGs. The MHPSS TWG, operating within the humanitarian cluster system, serves as the backbone for coordination efforts. Co-led by the World Health Organization (WHO) and non-governmental organizations like the International Medical Corps (IMC), the TWG brings together more than 300 partners, including UN agencies, international and local NGOs, and government bodies (ReliefWeb, 2024). The TWG's mandate is both pragmatic and aspirational: to ensure that MHPSS services are accessible, equitable, and responsive to the needs of a population.
Key coordination activities include:
Information management, including service mapping and referral systems: The TWG maintains a 4Ws (Who, What, Where, When) database to track MHPSS services across regions, ensuring efficient referrals between basic, community-based, focused, and specialized care providers (IASC, 2022).
Capacity building: Training programs for non-specialists, such as community health workers and teachers, have expanded the reach of focused non-specialized support, aligned with layer 3 of the IASC intervention pyramid (Kang et al., 2024).
Advocacy and policy alignment: The TWG collaborates with the Ukrainian Ministry of Health to integrate MHPSS into national healthcare systems, addressing critical infrastructure and policy gaps (UNHCR, 2023).
These efforts reflect a layered, complementary, and multi-sectoral model of care that bridges clinical, community, and policy dimensions, ensuring that interventions are both scalable and contextually relevant.
The effectiveness of MHPSS coordination in Ukraine is shaped by the dynamic contributions of international, national, and local actors:
International organizations such as WHO and UNICEF lead on technical guidance and funding, while NGOs like Médecins Sans Frontières (MSF) deliver specialized mental health services in frontline areas (Hino et al., 2023).
National government, despite limited resources, has prioritized mental health reforms, such as the Concepts for the development of mental health care in Ukraine for the period until 2030, which aligns with IASC guidelines (Ministry of Health of Ukraine, 2018; Frankova et al. 2024).
Local communities lead grassroots initiatives including resilience centers and peer support groups, leverage social support networks, and address layer 2 needs, fostering community cohesion (Harrison et al., 2021).
However, overlapping mandates and fragmented roles occasionally disrupt service alignment and reduce resource efficiency (Roberts et al., 2019).
To illustrate the scope of MHPSS coordination, future iterations of this article will include visual aids, such as:
A map of MHPSS service coverage across Ukraine, highlighting disparities between urban and rural areas (https://reliefweb.int/updates?view=maps&advanced-search=%28PC241%29&search=MHPSS; https://app.powerbi.com/view?r=eyJrIjoiOTJmZjg1ZWQtZDhlMC00YzYxLWFmZjQtOGY5ZjE0NDZlMDc2IiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9).
Flowcharts visualizing referral pathways across the layers of interventions (see fig. 1.).
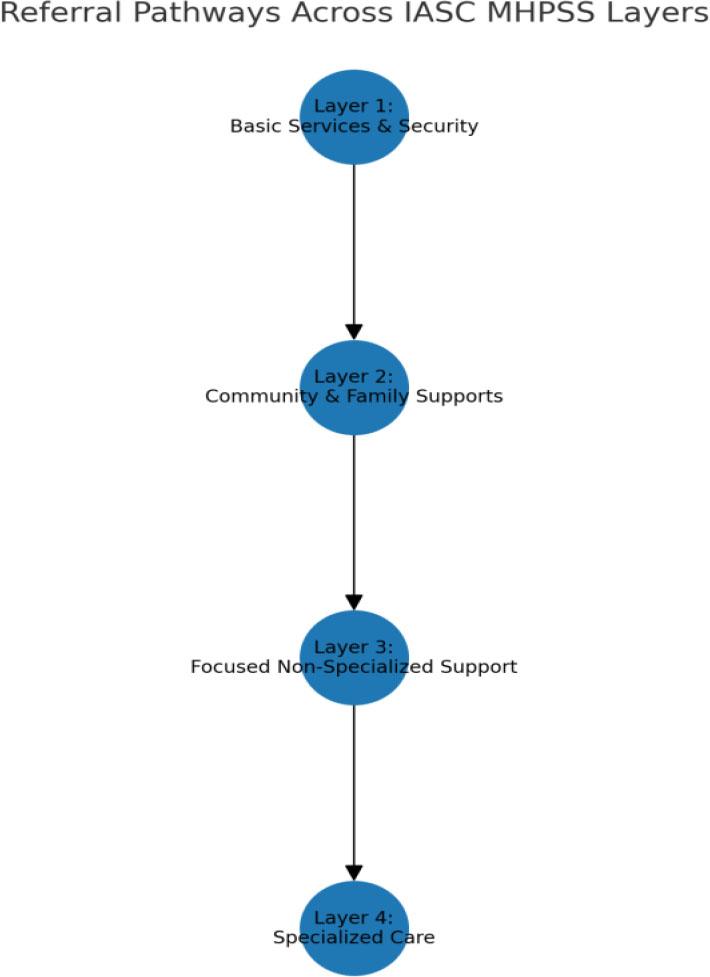
Referral Pathways Across IASC MHPSS Layers: This figure presents a simplified representation of referral pathways within the IASC MHPSS intervention framework. In practice, these pathways are non-linear and often overlapping. Individuals in need of specialized services may simultaneously benefit from lower-layer interventions, such as community-based support groups and basic services that uphold dignity and promote social inclusion.
MHPSS coordination in Ukraine demonstrates the practical application of the IASC intervention pyramid within a conflict-affected context. While notable progress has been achieved through coordination mechanisms, particularly the efforts led by the MHPSS TWG, persistent challenges remain, including stigma, provider burnout, funding shortfalls, and limited access to services. Addressing these issues will require innovative, context-responsive solutions. This study will subsequently examine MHPSS coordination in greater depth, focusing on its practical implementation and impact.
In Ukraine, where the reverberations of war are felt across communities and institutions, understanding MHPSS coordination requires both methodological rigor and adaptive thinking. This study adopts a combined theoretical and visual analytical approach to examine the interplay of actors, interventions, and operational challenges. Our aim is twofold: to construct a robust theoretical framework that explains MHPSS coordination dynamics and to visualize these complexities in a way that bridges academic insight with practical utility. Below, we outline the research design, data sources, and analytical approach that guide this exploration.
This study adopts a qualitative, desk-based research design grounded in narrative synthesis and complemented by theoretical modeling. Given the ongoing conflict and the logistical constraints of primary data collection, we leverage secondary sources, including peer-reviewed studies, humanitarian reports, and policy documents to build a comprehensive picture of MHPSS coordination. This approach aligns with Miller and Rasmussen's (2010) call for integrating trauma-focused and psychosocial frameworks in conflict settings, allowing us to explore social-environmental dimensions.
The methodology unfolds in two phases:
Conceptual Framework Development: Findings from the literature are synthesized into a conceptual model that identifies key variables, such as coordination mechanisms, stakeholder roles, and intervention outcomes, and maps the relationships among them.
Data Sourcing and Triangulation: Data are drawn from a purposive sample of secondary materials selected for their relevance to MHPSS coordination in the Ukrainian context. These include:
Academic Literature: Empirical studies such as Roberts et al. (2019) and Nguyen et al. (2023) which offer quantitative and qualitative insights into mental health prevalence, services, and intervention outcomes.
Humanitarian Reports: Documents from the MHPSS TWG, UNHCR (2023), and ReliefWeb (2024) offer operational data on coordination and service delivery.
Policy Frameworks: Strategic guidance from national and international sources, including the Ukrainian Ministry of Health's 2023 National Mental Health Strategy and the IASC (2007, 2022) which ground the analysis in policy and programmatic realities.
These sources are triangulated to ensure validity, cross-referencing empirical findings with practitioner perspectives and policy goals.
The analysis is conducted using a thematic narrative synthesis, a method well-suited to integrating diverse qualitative sources into a coherent explanatory framework (Popay et al., 2006). Drawing on the findings of the literature review, we organize the data into thematic clusters, including: The impact of conflict on mental health, the effectiveness of MHPSS interventions, coordination mechanisms, roles of key actors, and identified research and implementation gaps.
Within each theme, we apply an iterative process of analysis guided by three questions:
What recurring barriers, such as stigma, workforce burnout, or funding shortages, emerge across different contexts?
In what ways do local actors shape intervention outcomes?
How do coordination mechanisms mitigate or exacerbate inequities in access and quality?
To interpret these dynamics, we draw on the IASC MHPSS framework (2007) and localization theory (Barakat & Milton, 2020), proposing a conceptual model that emphasizes adaptability, multisectoral collaboration, and community ownership.
Findings are refined through constant comparison across data sources to ensure internal consistency and contextual relevance, ultimately producing a nuanced theoretical framework reflective of Ukraine's evolving MHPSS landscape.
While this methodology offers valuable insights, it is subject to several limitations. The reliance on secondary data limits our ability to capture real-time shifts in Ukraine's conflict dynamics. Additionally, the absence of primary stakeholder voices such as those of service users or frontline workers risks skewing the analysis toward the perspectives of institutional and published actors. To mitigate this, we prioritized recent and relevant sources to ensure relevance to the current crisis phase and applied triangulation across diverse document types.
This study portrays Ukraine's MHPSS coordination system as both strained and adaptive, situated in a context of protracted conflict, mass displacement, and institutional fragility. Coordination emerges not only as an operational necessity but as a strategic and conceptual anchor for effective humanitarian response.
The central role of the MHPSS TWG aligns with the IASC's vision of layered, multisectoral coordination, spanning from basic services to specialized clinical care (IASC, 2007). Tools such as the 4W mapping database and training initiatives for non-specialists bridge the gap between trauma-focused and community-based responses, resonating with Miller and Rasmussen's (2010) call to reconcile clinical and psychosocial paradigms. This synthesis addresses both the acute needs of individuals and the broader societal systems that underpin resilience.
The Service mapping tool holds promise for data-informed decision-making, offering actionable insights for resource allocation and referral management (OCHA, 2021). By visualizing service gaps, these tools could guide policymakers in targeting resources by deploying mobile clinics or streamlining referrals. Their significance lies not just in their utility but in their potential to bridge the gap between research and practice, a perennial challenge in MHPSS scholarship (Tol et al., 2011).
In addition, a nation-wide survey by Roberts et al. (2019) found that IDPs accessing community-based support reported a 25% reduction in psychological distress, affirming the role of social support as a protective factor. In 2023, the TWG partners have offered MHPSS services for over 1.2 million individuals, with 60% receiving community or family support, aligning with the IASC's emphasis on Layer 2 interventions (ReliefWeb, 2024). Yet, gaps persist. The prevalence of PTSD among veterans, estimated at 20–30%, underscores the need for expanded specialized care, particularly in rural regions where access remains limited (Nguyen et al., 2023; Hino et al., 2023).
Furthermore, several persistent barriers continue to impede the effective delivery of MHPSS services in Ukraine:
Stigma surrounding mental health: Cultural norms, especially among men and veterans, often frame mental health support as a sign of weakness. In a 2023 survey, only 40% of veterans with PTSD symptoms reported seeking help, primarily due to fear of judgment (Nguyen et al., 2023). This stigma discourages help-seeking behaviors and reduces service uptake (Kang et al., 2024).
Service provider burnout: MHPSS staff face high levels of emotional exhaustion due to sustained exposure to trauma, which in turn affects service quality and staff retention (Harrison et al., 2021). A study by Kang et al. (2024) found that 60% of MHPSS staff in Ukraine reported moderate to severe emotional exhaustion, highlighting the need for staff support programs.
Funding shortfalls: Humanitarian funding for MHPSS remains inadequate. In 2023, only 30% of the MHPSS budget outlined in the Ukraine Humanitarian Response Plan was fulfilled, constraining program scale and continuity (UNHCR, 2023). This scarcity is acutely felt in rural areas, where specialized services are scarce (Hino et al., 2023).
Restricted access in conflict zones: Ongoing hostilities, particularly in eastern and southern regions, severely limit the delivery of both basic and specialized mental health services (ReliefWeb, 2024).
These intersecting challenges highlight the urgent need for adaptive and flexible delivery models to expand MHPSS coverage in hard-to-reach and underserved areas. Innovations such as telehealth platforms and mobile clinics exemplify adaptive resilience, serving as systems-level responses to acute stressors that do not collapse but evolve under pressure (Holling, 2001). These modalities have helped extend services to populations otherwise excluded due to geographic or infrastructural barriers. Similarly, integrating mental health into primary care as a strategy to reduce stigma reflects a psychosocial approach that prioritizes community norms over clinical isolation (IASC, 2007).
However, these innovations should be seen as transitional measures, not long-term solutions. The unmet funding targets (only 30% of the MHPSS component of the 2023 Humanitarian Response Plan was financed) and high burnout rates among service providers underscore vulnerabilities that coordination alone cannot address (UNHCR, 2023; Kang et al., 2024). These findings urge a rethinking of humanitarian financing and workforce support, perhaps drawing on frameworks such as the Sphere Standards, which balance short-term efficiency with long-term sustainability (Sphere Association, 2018).
The literature also identifies persistent gaps in data sharing and service duplication (Harrison et al., 2021). These challenges reflect broader debates in humanitarian coordination, especially the divergence between centralized, top-down structures and the flexibility required for localized responses (Barakat & Milton, 2020). In Ukraine, the TWG's top-down structure may streamline efforts but risks sidelining local innovations, a dynamic deserving further exploration.
In addition, overlapping mandates and diverging priorities among actors occasionally hinder effective coordination. For instance, international NGOs often emphasize rapid-response interventions, while local organizations advocate for sustainable, community-driven approaches better aligned with long-term needs (Roberts et al., 2019). International agencies bring critical funding and technical expertise, but local organizations possess the contextual knowledge and social capital essential for sustainable delivery. This imbalance reflects the localization agenda's ongoing struggle for equitable power-sharing (Barakat & Milton, 2020). Few case examples illustrate both collaboration and friction, where local actors have raised concerns about externally led, short-term projects (Roberts et al., 2019).
This divergence is rooted in deeper humanitarian power dynamics, where those controlling resources often shape priorities (Duffield, 2012). Strengthening local leadership within coordination bodies such as the TWG could mitigate such disparities and promote more sustainable, community-anchored interventions, an approach with relevance far beyond Ukraine. In addition, the MHPSS TWG seeks to navigate these concerns by fostering multisectoral dialogue and promoting alignment through the IASC's Minimum Service Package, ensuring that no one is left behind (IASC, 2022).
Finally, this study is subject to several limitations. First, our reliance on secondary literature limits our ability to capture real-time shifts in Ukraine's MHPSS landscape, particularly as the conflict evolves. Primary data from frontline workers or beneficiaries could enrich the narrative, offering perspectives beyond what published studies provide. Furthermore, the specific focus on Ukraine may limit broader applicability, though the conceptual frameworks presented here are transferable to other crisis contexts.
This study has systematically examined the complex dynamics of MHPSS coordination in Ukraine, revealing a system characterized by both remarkable resilience and systemic challenges. Through a dual theoretical and visual analytical approach, we have explored the complex interplay between institutional actors, intervention strategies, and structural barriers findings that carry significant implications for humanitarian MHPSS delivery in conflict-affected regions globally.
The MHPSS TWG has emerged as a cornerstone of Ukraine's response, operationalizing the IASC guidelines to align multi-stakeholder efforts. However, persistent challenges underscore the necessity for adaptive coordination models. Such models could prioritize decentralized decision-making and context-specific adaptations to bridge gaps between policy frameworks and on-the-ground realities (IASC, 2022; Alem et al., 2023).
A persistent divergence exists between international actors (e.g., UN agencies, INGOs) and local stakeholders (e.g., community health workers, faith-based organizations). While international partners provide essential resources, their dominance in planning processes often marginalizes local expertise, inadvertently perpetuating dependency (Harrison et al., 2021). This study aligns with broader critiques of the “localization agenda” (Barbui et al, 2020), advocating for structural equity in funding and leadership to ensure sustainable MHPSS systems.
Ukraine's MHPSS landscape has demonstrated remarkable ingenuity, with telehealth platforms and mobile clinics mitigating barriers such as stigma (WHO, 2023) and infrastructure collapse. Yet, these solutions remain stopgap measures. For instance, digital interventions reach only a portion of frontline communities due to connectivity issues, highlighting the need for hybridized approaches that combine technology with community-based care (WHO, 2023a).
The study's visual tools including GIS-based service mapping and stakeholder network diagrams – have empirically demonstrated coordination gaps, such as the disproportionate concentration of services in urban centers (dn.who.int/media/docs/default-source/mental-health/special-initiative/who-mhpss-support-to-ukraine_feb_2023.pdf). These tools offer policymakers a data-driven roadmap for reallocating resources and strengthening multisectoral coordination (e.g., health, education, and peacebuilding sectors).
While this analysis provides a comprehensive overview of coordination challenges, its reliance on secondary data precludes granular insights into real-time implementation barriers. The absence of primary data from frontline providers and service users limits our understanding of lived experiences within the system.
To advance MHPSS coordination, three priorities emerge:
Invest in training programs for community health workers and grassroots organizations, ensuring interventions align with cultural norms.
Integrate MHPSS within broader humanitarian frameworks (e.g., peacebuilding, education) using IASC Common Monitoring and Evaluation Framework to track multi-sectoral outcomes.
Conduct longitudinal, mixed-methods research to better understand evolving needs among displaced populations and to evaluate the long-term efficacy of coordination models.
Ukraine's MHPSS infrastructure serves as both a microcosm of global humanitarian challenges and a testament to the resilience of decentralized, community-led support networks. By addressing the divergence between standardization and flexibility, global expertise and local agency, this study charts a path forward for MHPSS systems in conflict zones, one rooted in equity, innovation, and empirical rigor.