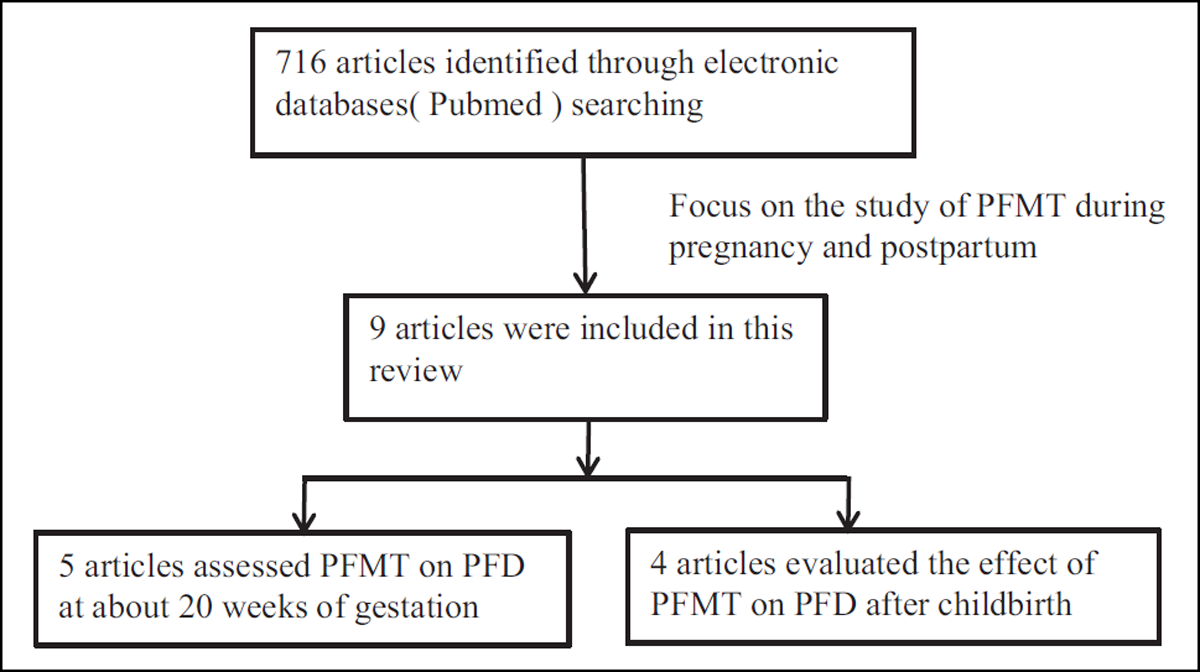
Figure 1
The flowchart of literature searching and screening.
Table 1
Summary of studies’ assessment of pelvic floor muscle training on PFD during pregnancy.
| Reference | Participants/GW | Training duration | Interventions | Primary outcome | Main findings |
|---|---|---|---|---|---|
| Reilly et al. 2002 | 268 nulliparous with bladder neck mobility;GW 20th | until delivery | Exp (n = 139): supervised PFMT + self-daily training Con (n = 129): verbal advice on PFMT Supervised PFMT program: one-to-one, every month; Self-daily training at home: 3 repetitions of 8 contractions for 6 s with 2 mins rest between repetitions (repeated BID). At 34th GW, the number of contractions per repetition was increased to 12. | Subjective reporting of SUI at 3 months postpartum. | Antenatal supervised PFMT can reduce the risk of postpartum SUI effectively in primigravidae with bladder neck mobility. |
| Siv et al. 2003 | 310 nulliparous; GW 20th | 12 weeks | Exp (n = 148): supervised PFMT + self-daily training Con (n = 153): received the customary information supervised PFMT program: 10–15 participants, 60 minutes per session, every week, 12th times. perform near-maximal PFM contractions, and hold the contraction 6–8 s. At the end of each contraction, add 3–4 fast contractions with about 6 s resting period; Self-daily training at home: 8–12 equally intensive PFM contractions BID. | Self-reports of UI at 36th GW and 3 months after childbirth | Intensive PFMT duringpregnancy prevents UI during pregnancy and after delivery. |
| Salvesen and Mørkved 2004 | 301 nulliparous; GW 20th | 12 weeks | Exp (n = 148): supervised PFMT + self-daily training Con (n = 153): received the customary information supervised PFMT program: 10–15 participants, 60 minutes per session, every week, 12 times. Perform near maximal PFM contractions, and to hold the contraction 6–8 s. At the end of each contraction, add 3–4 fast contractions with about 6 s resting period; Self-daily training at home: 8–12 equally intensive PFM contractions BID. | Duration of the second stage of labor and the rate of prolonged second stage* | A structured PFMT is associated with fewer cases of active pushing in the second stage of labor. |
| Agur et al. 2008 | 268 primigravidae with antenatal bladder neck mobility; GW 20th | until delivery | Exp(n = 139): supervised PFMT + self-daily training Con(n = 129): verbal advice on PFMTsupervised PFMT program: one-to-one, every month; Self-daily training at home: 3 repetitions of 8 contractions for 6 s with 2 mins rest between repetitions (repeated BID). At 34th GW, the number of contractions per repetition was increased to 12. | The duration of the second stage of labour and the incidence of instrumental deliveries | PFMT during pregnancy does not facilitate or obstruct labour or result in a higher incidence of prolonged labour* or instrumental delivery. |
| Szumilewicz et al. 2019 | 97 nulliparas; GW average 21th | 6 weeks | Exp (n = 70): high-low impact aerobics + PFMT Con (41) = no training high-low impact aerobics + PFMT: 3 times a week, every 2 weeks check the quality each session consisted of: a warm up, aerobics in the form of high- and low-impact aerobic choreography with music (25 min), strength conditioning exercises (25 min), and stretching and breathing exercises and relaxation (10 min). | PFM EMG | Prenatal exercise programs that include high- and low-impact aerobics and are supported by PFMT should be recommended for pregnant women. |
[i] BID = twice a day; Con = control group; EMG = electromyogram; Exp = experimental group; GW = gestational week; PFM = pelvic floor muscles; PFMT = pelvic floor muscles training; SUI = stress urinary incontinence; UI = urinary incontinence.
* The prolonged second stage is the time of active labor is longer than 60 minutes.
Table 2
Summary of studies’ assessment of pelvic floor muscle training on PFD after childbirth.
| Reference | Participants/after delivery | Training duration | Interventions | Primary outcome | Main findings |
|---|---|---|---|---|---|
| Siv and Kari 1997 | 196 mothers; 8 weeks | 8 weeks | Exp (n = 99): supervised PFMT + self-daily training Con (n = 99): followed the ordinary written postpartum instructions from the hospital Superxised PFMT program: 5–10 participants, 45 mins once a week; Self-daily training at home: 8–12 maximum PFM contractions BID, hold the contraction for 6–8 s, at the end of each contraction 3–4 fast contractions were added. | The improvement of PFM strength and the number of women with UI. | PFMT is effective in increasing pelvic floor muscle strength and reducing UI in the immediate postpartum period. |
| Gunvor et al. 2013 | 175 primiparous women; 6 weeks | 16 weeks | Exp (n = 87): superxised PFMT + self-daily training Con (n = 88): verbal advice on PFMT Superxised PFMT program: Once a week follow up; Self-daily training at home: 3 sets of 8–12 contractions close to maximum every day. | Self-reported UI | Postpartum PFMT did not decrease UI prevalence 6 months after delivery. |
| Kari et al. 2014 | 175 primiparous women; 6–8 weeks | 16 weeks | Exp (n = 87): superxised PFMT + self-daily training Con (n = 88): verbal advice on PFMT Superxised PFMT program: Once a week follow up; Self-daily training at home: 3 sets of 8–12 contractions close to maximum every day. | POP stage II or greater assessed by POP quantification, bladder neck position and symptoms of vaginal bulge | PFMT had no effect on POP. |
| Sigurdardottir et al. 2019 | 84 primiparous women with UI; 9 weeks | until 6 months postpartum | Exp (n = 41): superxised PFMT + self-daily training Con (n = 43): no training Superxised PFMT program: 12 sessions, each 45–60 min, once a week. one session is 10 close to maximum contractions and 7 s holding periods with a 10 s rest between each contraction, during appointments 8–9, add 3 fast contractions at the end of each contraction and do so in the remaining sessions. Self-daily training at home: 10 close-to-maximum PFM contractions, 3 sets/day + the Knack* | the rate of urinary and/or anal leakage | Postpartum PFMT decreased the rate of UI, increased muscle strength and endurance. |
[i] BID = twice a day; Con = control group; Exp = experimental group; PFM = pelvic floor muscles; PFMT = pelvic floor muscles training; UI = urinary incontinence.
* The knack is that patients are instructed to contract the pelvic floor every time when coughing or sneezing.
| Full name | Abbreviation |
| control group | Con |
| electromyogram | EMG |
| experimental group | Exp |
| gestational week | GW |
| Pelvic floor dysfunction | PFD |
| pelvic floor muscles | PFM |
| Pelvic floor muscles training | PFMT |
| pelvic organ prolapse | POP |
| sexual dysfunction | SD |
| stress urinary incontinence | SUI |
| twice a day | BID |
| urinary incontinence | UI |
