Significance of This Study
In 2015, an estimated 1.6 million deaths worldwide stemmed from a diabetes-related medical complication (WHO 2016). Cardiovascular complications are thought to be the most common medical complication. About 75% of individuals with diabetes die of cardiovascular disease—with the mortality rate from cardiovascular disease five times higher in people with diabetes than individuals without diabetes (NICE 2017). Emerging research suggests regular physical activity decreases the incidence of Type 2 diabetes related-complications such as cardiovascular disease and reduces the risk of mortality.
What are the new findings?
From the review of the available data, physical activity has been shown to improve glycemic control and cardiac function, and reduce insulin resistance and cholesterol levels in people with Type 2 Diabetes.
Recommendations
Individuals with type 2 diabetes should be advised to undertake regular physical activity but are recommended to undergo appropriate pre-exercise screening before beginning any vigorous program.
Type 2 Diabetes Mellitus (T2DM) is multisystem disease characterized by the body’s inability to produce or use the hormone insulin to regulate blood glucose levels. Type 2 Diabetes is a fast-growing worldwide epidemic that is only expected to increase due to rising rates of obesity and decreased physical activity (Morkos et al. 2018). By the year 2050, an estimated 1 in 3 adults in the United States will have diabetes (Sweatman et al. 2017). In terms of economic costs, diabetes costs health care systems an estimated $210.5 billion per annum due to the direct and indirect costs of diabetes-related medical complications (Sweatman et al. 2017). This epidemic has the potential to overwhelm health systems if it is not addressed from a public health perspective.
The prevailing theory on the modifiable risk factors which increase the risk of Type 2 diabetes development include a low-fiber high-glycemic index diet, high meat consumption, obesity, and lack of physical inactivity (Toumpanakis, Turnbull & Alba-Barba 2018). This insulin resistance and defect in the secretion of insulin leads to significant morbidity and mortality from complications due to elevated blood glucose. Due to an elevated blood glucose, individuals with type 2 diabetes are at an increased risk for coronary artery disease or end-stage kidney disease (Rees, Levy & Lansdown 2017). Similarly, over time the elevated blood glucose levels cause nervous system damage known as neuropathy which plays a major role in the development of foot ulcers. This widespread nervous system damage leads to a lack of sensation and in turn foot ulcer development which can cause on enormous effect on the quality of life for an individual (especially if lower-limb amputation becomes necessary due to foot ulceration) (Rees et al. 2017). Likewise, an elevated blood glucose level can cause a variety of eye problems, the most common being diabetic retinopathy which can lead to vision loss (Rees et al. 2017).
Individuals who are diagnosed with Type 2 diabetes are prescribed medication and are recommended to undertake lifestyle changes, including physical activity, weight reduction if overweight, and intake of a healthy diet (Toumpanakis, Tumbull & Alba-Barba 2018). Despite advancements in medicine and in the medical management of Type 2 Diabetes, the reduced life expectancy from diabetes related complications are increasingly unabated and remain unprecedented with diabetes being a leading cause of morbidity and mortality worldwide. In 2015, an estimated 1.6 million deaths worldwide stemmed from a diabetes-related medical complication (WHO 2016). Similarly, in the United States, diabetes is currently the 7th leading cause of death (CDC 2016). Cardiovascular complications are thought to be the most common diabetes-related medical complication. About 75% of individuals with diabetes die of cardiovascular disease—with the mortality rate from cardiovascular disease five times higher in people with diabetes than individuals without diabetes (NICE 2017).
Obesity remains the main preventable cause of type 2 diabetes and its’ related complications. With sedentary ways of life becoming more common, people are less likely to meet or exceed recommended guidelines of physical activity. Physical activity leads to a significant reduction in the risk of being diagnosed with diabetes and reduces the morbidity and mortality of diabetes (Bird & Hawley 2017). Obesity occurs due to an energy intake and energy expenditure imbalance (Sigal et al. 2018). Physical activity such as exercise leads to a balance or deficit in energy (Karstoft et al. 2013). With urbanization and public planning changes, individuals have less areas to walk and rely on motor vehicles and public transport to navigate urban spaces. Furthermore, socioeconomic factors such as the type of neighborhoods they live in, job loss, having to work overtime to maintain a standard of living, and poverty have reduced any opportunities individuals have to be physically active.
According to Bouchard, Blair and Haskell (2012), physical activity is defined as any bodily movement produced by skeletal muscles that results in an increase in the metabolic rate over resting energy expenditure. Exercise is a form of “leisure-time” physical activity performed repeatedly to improve fitness and health (Bouchard et al. 2012). Aerobic exercise is any physical activity such as walking, jogging, swimming, or cycling which involves continuous movements of large muscle groups (Sigal et al. 2013). Resistance exercise is any physical activity which involves weight bearing exercises to increase muscle strength and endurance. While flexibility exercises such as yoga are a form of physical activity which enhance the ability of joints to move through their whole range of motion (Sigal et al. 2013; Bouchard et al. 2012).
Physical activity has both immediate and longer-term effects on insulin sensitivity and glycemic control (Bird & Hawley 2017). This is especially crucial in individuals with type 2 diabetes. Within a short duration of time, type 2 diabetes has been shown to decrease aerobic capacity, reduce heart rate response, stroke volume and cardiovascular response in individuals (Gusso et al. 2008). During physical activity, glucose uptake occurs through a glucose transporter. Prior studies suggest physical activity improves insulin sensitivity through the glucose transporter, maintains body weight, reduces the risk of cardiovascular disease, reduces diabetes-related stress, and increases life expectancy in individuals diagnosed with diabetes (Sigal et al. 2013; Sigal et al. 2018). Emerging research also suggests regular physical activity decreases the incidence of type 2 diabetes related-complications and reduces the risk of mortality (Sigal et al. 2018). However, there is no general consensus as other studies have had contrasting results. The aim of this review was to assess the efficacy of physical activity to reduce the risk of diabetes related morbidity and mortality of individuals with type 2 diabetes.
Methods
Literature searches were conducted in the following databases: MEDLINE, Embase, CINAHL, PubMed, and the Cochrane library using the search terms “physical activity intervention” AND “type 2 diabetes.” The searches were conducted from September to November 25th 2018. Inclusion Criteria: Eligible studies included randomized controlled trials published since 2008 to present investigating the effect of physical activity and/or exercise on health outcomes in individuals with type 2 diabetes. Studies with participants with type 1 diabetes were excluded. The control groups had to have had standard usual care, no intervention, or some other intervention that were not physical activity based as a control. Because of the heterogeneity of the various physical activity studies reviewed, meta-analyses could not performed.
Results
After careful screening for studies which only met the inclusion criteria, 15 studies were selected from 300 study abstracts which were initially identified as meeting the inclusion criteria. Selection of the included studies and the inclusion and exclusion process are illustrated in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) diagram below (Figure 1).
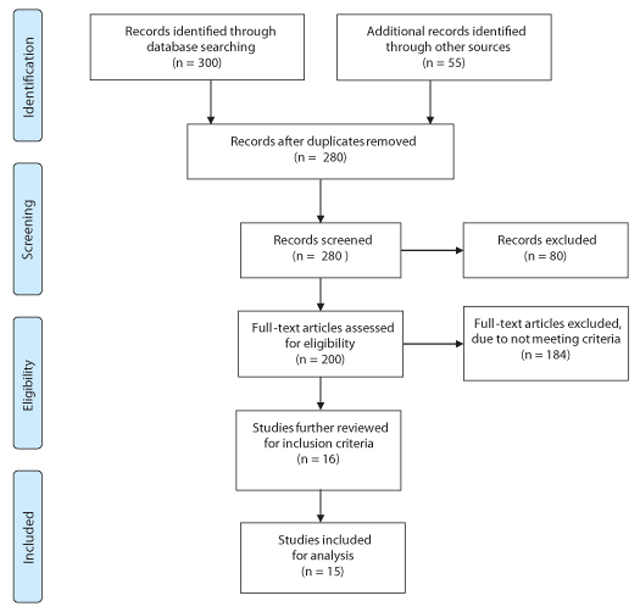
Figure 1
Prisma Diagram.
Study Characteristics
Study characteristics assessed included (sample size, follow-up time points), study participant’s characteristics as available (age, race, sex, disease co-morbidity), the type of physical activity intervention (i.e. aerobic or resistance training), and associated health outcomes (improved glycemic control, lowered cholesterol values, reduced mortality risk). The populations studied varied considerably. Some studies limited participation to women or the elderly, while other studies assessed intervention efficacy in individuals with co-morbidities such as hypertension or diabetic related peripheral neuropathy. The length of the interventions assessed varied from 4 to 12 months. Besides one study, all of the other randomized controlled trials assessed glycemic control and/or cholesterol values as outcomes of interest. In the LeMaster et al. (2008) study, the only outcome of interest was the prevalence of foot ulcers in individuals with type 2 diabetes and diabetic peripheral neuropathy. The intervention frequency of the various forms of physical activity varied considerably. The Church et al. (2010) intervention was 500 to 1000 MET minutes of aerobic training and 2 days of resistance training. The Balducci et al. (2010) intervention was a mix of aerobic and resistance training performed twice a week.
Types of Physical Activity
The interventions assessed in this review varied from playing soccer to walking on a treadmill. Four interventions used a combination of resistance and aerobic physical activity (Balducci et al. 2010; Church et al. 2010; Mitranun et al. 2014; Sparks et al. 2013). Mavros et al. (2013) assessed the efficacy of High-intensity progressive resistance power training to improve glycemic control in older adults. Similarly, Cassidy et al. (2006), studied the effect of HIIT (High Intensity Interval Training) to improve cardiac function in individuals with type 2 diabetes.
Discussion
The purpose of this systematic review was to investigate the efficacy of physical activity in reducing diabetes related health complications. The results of the systematic review varied considerably. According to the Vancea et al. (2009) study, walking on a treadmill as a form of physical activity for 3-5 times a week did not lead to any statistically significant differences in HbA1c between the intervention and control groups. However, the remainder of the studies reported physical activity had favorable effects on improving glycemic control and reducing HbA1c and cholesterol values. A possible explanation for the lack of results in the Vancea et al. (2009) study could possibly be attributed to the low MET (metabolic expenditure) of the form of physical activity used. For comparison, Sung and Bae (2012) reported that elderly individuals who walked 3 times per week for 50 minutes each time had reduced HbA1c and cholesterol levels in comparison to the sedentary controls. Similarly, Motahari-Tabari et al. (2014) reported that women who did a combination of stretching and flexibility exercises in combination with walking 3 times a week had significant reductions from baseline to intervention in insulin resistance.
Diabetic neuropathy is a medical condition where the nerves are damaged due to uncontrolled blood glucose levels. This nerve damage and reduced sensation in the extremities can lead to small injuries to develop without pain that can then develop into ulcers, infections, and gangrene requiring immediate amputation. In the LeMaster et al. (2008) study, physical activity such as a combination of walking, and leg strengthening and balance exercises did not lead to a difference in the prevalence of foot ulcers in individuals with type 2 diabetes and diabetic peripheral neuropathy.
In regard to cardiovascular risk reduction, Cassidy et al. (2016) reported individuals who were in the HIIT intervention group had improved cardiac function (systolic function and left ventricle mass) as well as reduced HbA1c. Individuals with type 2 diabetes often are at an increased risk of developing heart disease and reduced cardiac function due to elevated blood glucose levels. The results of the Cassidy et al. study are promising since about 75% of individuals with diabetes die of cardiovascular disease (NICE 2017). However, the Look ahead research study (2013), showed no statistically significant difference in the hazard risk between individuals in the intervention and control group. Over a follow up period of 11 years, there was no reduction in the risk of having a cardiovascular event for the participants in the intervention group who performed moderate intensity physical activity for at least 175 minutes per week.
The type of physical activity performed in the intervention had a substantial effect on the study results. Interventions with aerobic, resistance, or high intensity interval training were more likely to report a correlation between physical activity and improved health outcomes. In the Karsoft et al. (2013) intervention, individuals who did interval walking for 60 minutes, 5 times a week had improved glycemic control than the controls who did no form of physical activity. De Sousa et al. (2014) reported adult men and women who played soccer 3 times a week for 40 minutes had increased insulin sensitivity in comparison to the control group. Sparks et al. (2013) reported that individuals who performed aerobic, resistance, or a combination of both had reduced HbA1c and lower blood pressure values than individuals in the control group. From comparing the results of the various studies, it is apparent that aerobic exercise of greater than 5 times a week could lead to reduced HbA1c, insulin resistance, and cholesterol levels in individuals with type 2 diabetes. Physical activity is even more efficacious when aerobic activity is combined with resistance training.
Strengths and Limitations of the review
The review had numerous strengths. Evidence was only analyzed from randomized control studies (RCT) and this review was performed according to the thorough PRISMA guidelines. In regard to accuracy of measurement, 7 studies used HbA1c which is a more reliable measure of glycemic index as opposed to fasting blood glucose (NICE 2017).
It should be noted that this review only assessed the efficacy of physical activity in individuals with type 2 diabetes. There is a possibility that there might have been a different outcome if the inclusion criteria included studies with participants with type 1 diabetes. That limitation notwithstanding, the review identified how various forms of physical activity may improve health outcomes in various populations. The results from this review will be useful to researchers performing future research on the topic and to health care practitioners who seek to improve the health outcomes of their patients and clients with type 2 diabetes.
Limitations of Knowledge
When pooled together, 13 of the studies reviewed reported significant improvements in glycemic control. Previous studies have shown a concordance with this review’s findings. However, these studies varied in the types of physical activity studied and co-interventions used such as dietary restrictions, counselling, or group therapy. Larger randomized trials of these approaches are warranted in different types of communities living with type 2 diabetes.
Implications for future practice
Future research needs to clearly identify if physical activity has an impact on peripheral neuropathy and on the prevention foot ulcers. There also needs to be more research to identify the effect of physical activity in communities of color with type 2 diabetes. In all, the results from this review are promising. Individuals with diabetes should be encouraged to practice regular physical acitivity such as aerobic activity, resistance training, or HIIT for at least 30 minutes a day for 5 times a week.
Competing Interests
The author has no competing interests to declare.
