Table 1
VI-RADS scores
| VI-RADS 1 | It is highly improbable that there is any muscular invasion |
| VI-RADS 2 | The presence of muscle invasion is doubtful |
| VI-RADS 3 | The existence of muscle invasion is ambiguous |
| VI-RADS 4 | There is a high probability of muscle invasion |
| VI-RADS 5 | Muscle invasion and beyond the bladder is highly likely |
Table 2
Demographic data
| Age (years), mean | 67, 8 |
| Smoking history, n (%) | |
| Yes No | 10 (52) |
| 9 (48) | |
| Number of n | |
| Patients Lesions | 19 |
| 28 |
Table 3
Clinical characteristics of patients with incidental bladder lesions
| LARGEST LESION DIAMETER ONMPMRI (CM) | HISTOPATHOLOGY | |||
|---|---|---|---|---|
| VI-RADS SCORE | STAGE | GRADE | TREATMENT | |
| 1.1 | 2 | Ta | Low | TURBT |
| 1.5 | 2 | Ta | High | TURBT+BCG |
| 0.7 | 1 | Ta | Low | TURBT |
| 0.8 | 1 | Ta | Low | TURBT |
| 0.7 | 1 | Ta | Low | TURBT |
| 0.9 | 1 | Ta | Low | TURBT |
| 1.2 | 2 | Ta | Low | TURBT |
| 1.1 | 2 | Ta | Low | TURBT |
| 1.4 | 2 | Ta | Low | TURBT |
| 1.7 | 2 | Ta | Low | TURBT |
| 1.5 | 2 | Ta | Low | TURBT |
| 1.9 | 2 | Ta | Low | TURBT |
| 0.7 | 1 | Ta | Low | TURBT |
| 2.1 | 3 | T2, (SCNC) | High | Radical Cystectomy |
| 1.1 | 4 | T2 | High | Radical Cystectomy |
| 1.3 | 2 | Ta | Low | TURBT |
| 1.2 | 2 | Ta | Low | TURBT |
| 2 | 2 | Ta | Low | TURBT |
| 1.5 | 2 | Ta | Low | TURBT |
| 3.5 | 2 | T1 | High | TURBT + BCG |
| 0.6 | 1 | Ta | Low | TURBT |
| 0.9 | 1 | Ta | Low | TURBT |
| 0.8 | 1 | Ta | Low | TURBT |
| 0.7 | 1 | Ta | Low | TURBT |
| 0.8 | 1 | Ta | Low | TURBT |
| 2.8 | 5 | T2 | High | Radical Cystectomy |
| 0.5 | 1 | Benign (Inflamed urothelial tissue) | - | |
| 1.5 | 2 | Ta | Low | TURBT |
SCNC, small cell neuroendocrine carcinoma; TURBT, transurethral resection of bladder tumor; BCG, Bacillus Calmette–Guerin.
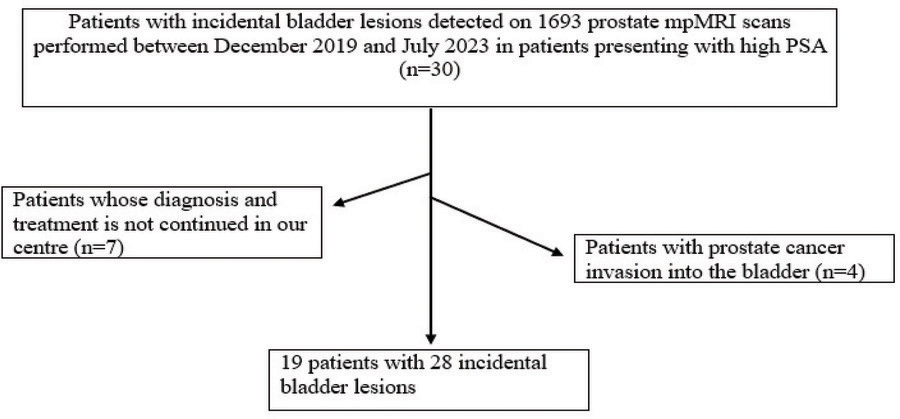
Figure 1
Flowchart of patient selection.
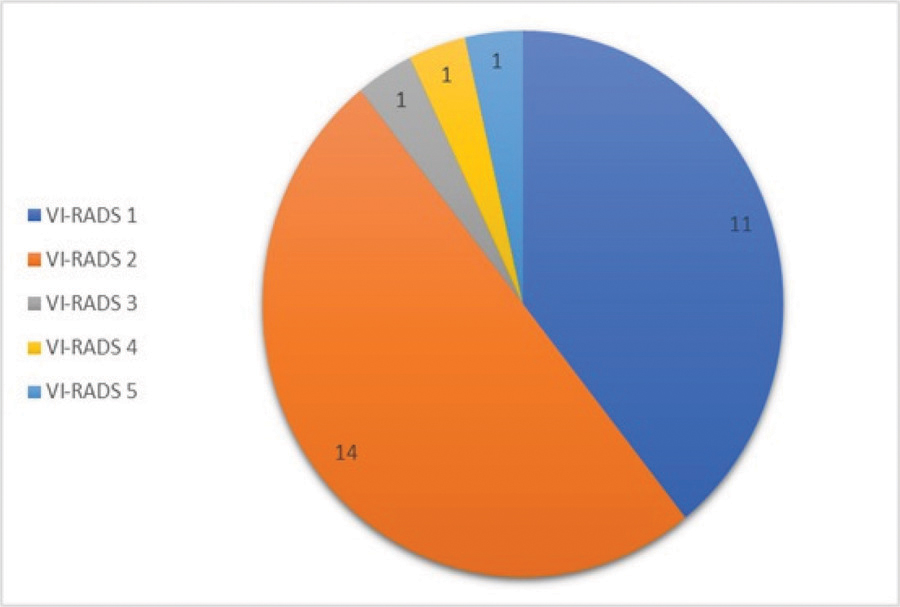
Figure 2
VI-RADS score distribution of incidental bladder lesions.
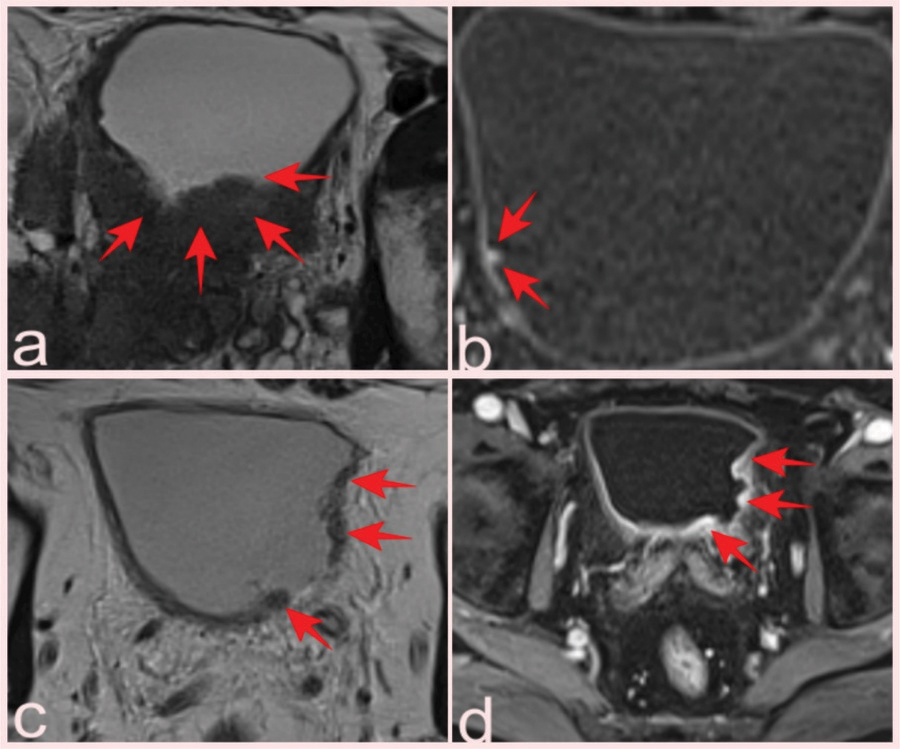
Figure 3
(a) Hypointense soft tissue showing bladder invasion on axial T2-WI in a 74-year-old man with Gleason score 3+4 prostate cancer (arrows). (b) Prostate mpMRI in a 66-year-old patient showed a 0.5 cm lesion on the right posterolateral wall of the bladder that was missed on conventional images but was detected by contrast uptake on DCE images and reported as VI-RADS 1; pathology was benign (Inflamed urothelial tissue) (arrows). T2-WI (c) and DCE (d) images of a 64-year-old patient with a high-grade pT2 tumor classified as VI-RADS 4 (arrows).
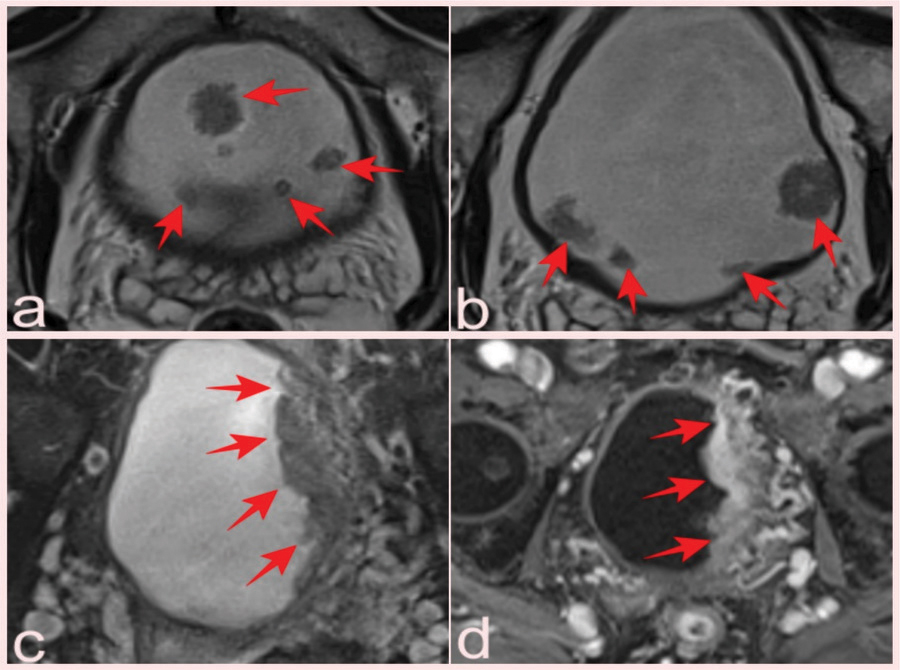
Figure 4
(a, b) Two slices from T2-WI of a 69-year-old patient who presented with elevated PSA and had a total of 10 lesions with pTa pathology, four of which were reported as VI-RADS 1 and six as VIRADS 2 (arrows). Fat-suppressed T2-WI (c) and (d) DCE images of a 75-year-old man with a serum PSA value of 8.9 ng/mL and Gleason score of 3 + 3 prostate cancer, with a lesion reported as VI-RADS 5 but pathologically as a high-grade pT2 tumor (arrows).
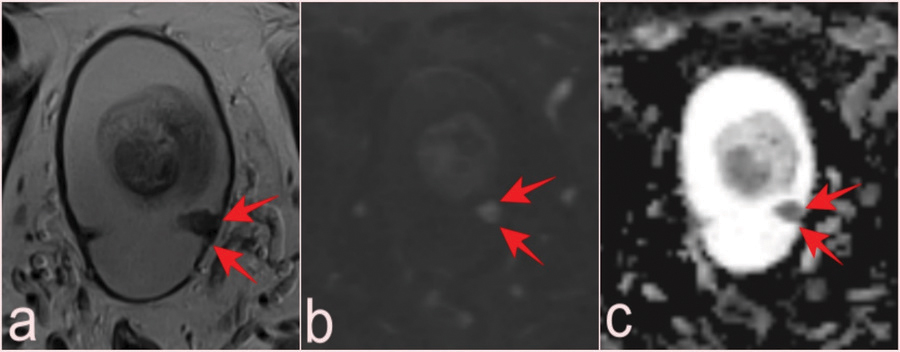
Figure 5
T2-WI (a), DWI (b), and ADC map (c) of a lesion with low-grade pTa tumor pathology reported as VI-RADS 1, which can be missed at the level of mucosal folds in a 69-year-old patient with prostate mpMRI after PSA elevation (arrows). ADC, apparent diffusion coefficient.
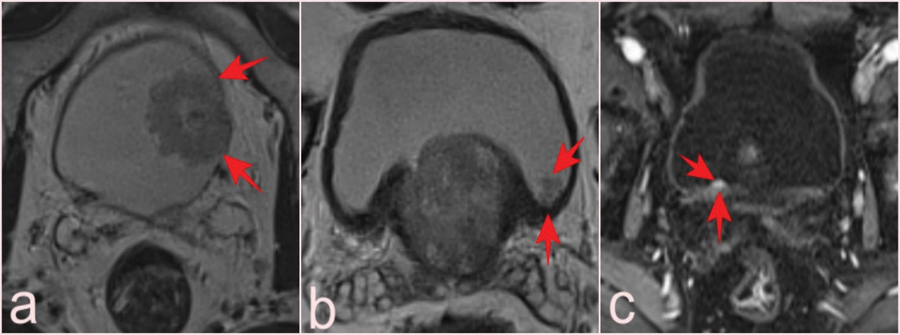
Figure 6
(a) T2-WI shows a VI-RADS 2 lesion with a high-grade pT1 tumor in a 74-year-old patient (arrows). (b) In a 60-year-old patient, a T2-WI image revealed a VI-RADS 1 lesion, 0.8 cm, missed without careful left posterior wall examination; pathology was pTa tumor (arrows). (c) VI-RADS 1 lesion, 0.6 cm, on the right posterior wall of a 74-year-old patient; contrast-enhanced DCE images aid selection; pathology: pTa tumor (arrows).
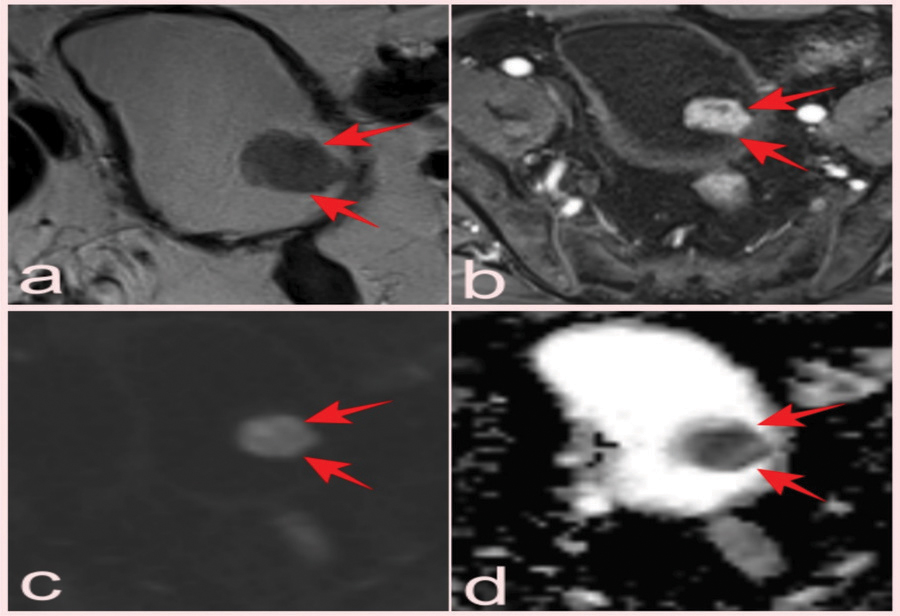
Figure 7
T2-WI (a), DCE images (b), DWI (c), and (d) ADC map of an incidental bladder lesion reported as VI-RADS 3 but pathologically diagnosed as high-grade pT2 small-cell neuroendocrine carcinoma on prostate mpMRI performed after elevated PSA in a 69-year-old patient (arrows).
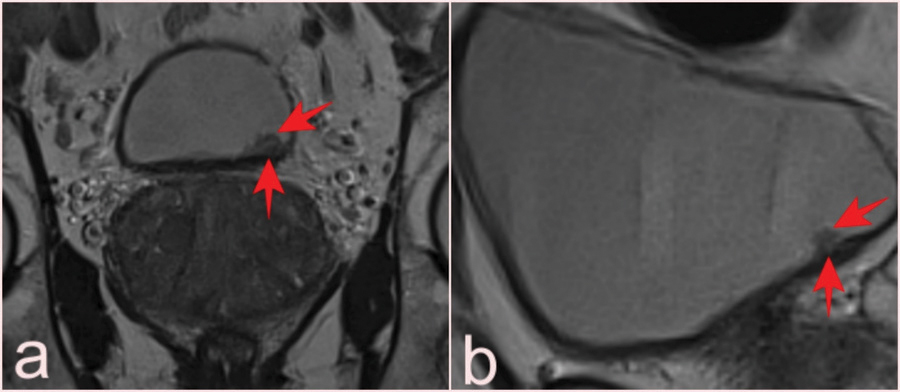
Figure 8
T2-WI of incidental bladder lesions detected only on coronal slices (a) in a 65-year-old patient, reported as VI-RADS 1, 0.7 cm in size and with pTa tumor pathology, and in sagittal slices (b) only in a 55-year-old patient, reported as VI-RADS 1, 0.8 cm in size and with pTa tumor pathology (arrows).
