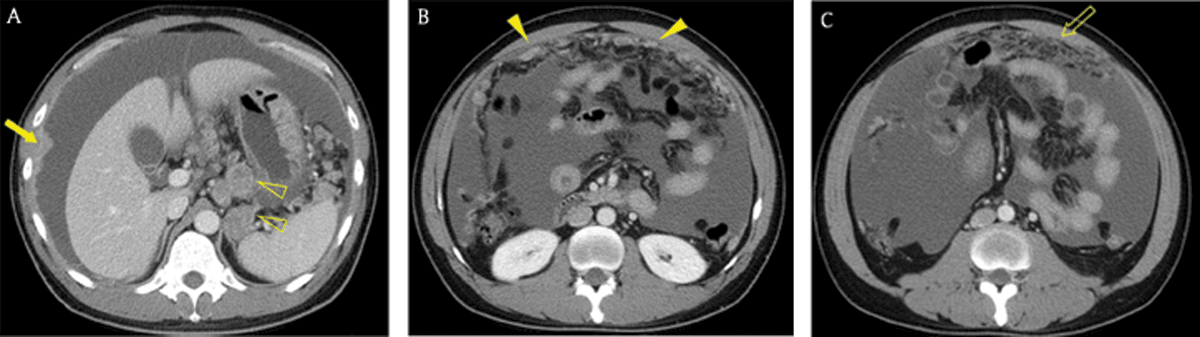
Figure 1
A 40-year-old man with advanced gastric cancer and peritoneal carcinomatosis. Axial portal venous phase CT images revealed multifocal discrete nodules (arrowheads) in the peritoneal cavity, peritoneal enhancement and thickening (arrow), ascites, and omental haziness (open arrow). Note the metastatic lymphadenopathy around the stomach (open arrowheads).
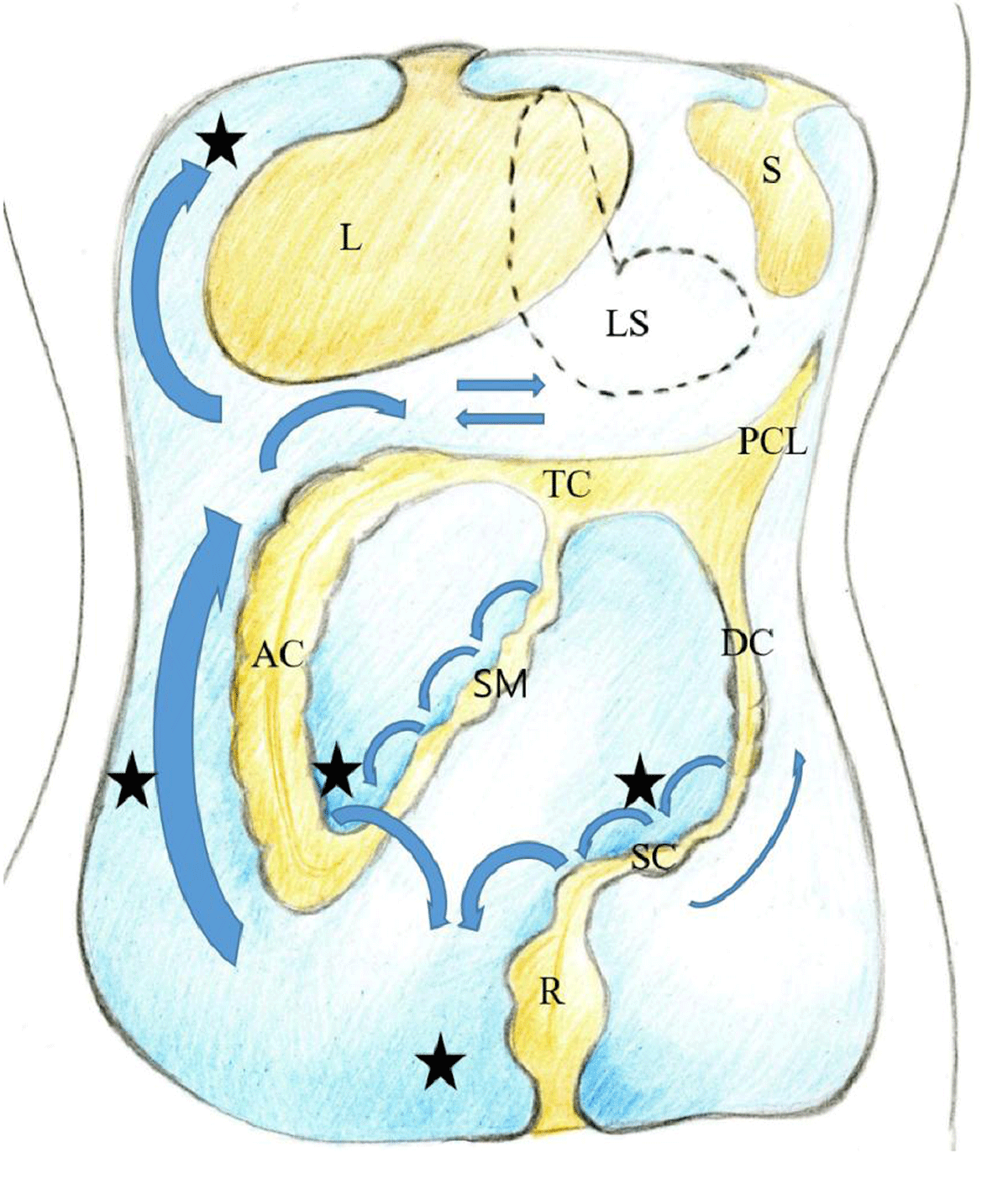
Figure 2
Coronal drawing of the peritoneal cavity illustrating the flow of peritoneal fluid (arrows) and frequent locations for peritoneal seeding (closed stars). L liver, LS lesser sac, S spleen, TC transverse mesocolon, PCL phrenicocolic ligament, AC ascending colon, DC descending colon, SM small bowel mesentery, SC sigmoid mesocolon, R rectum.
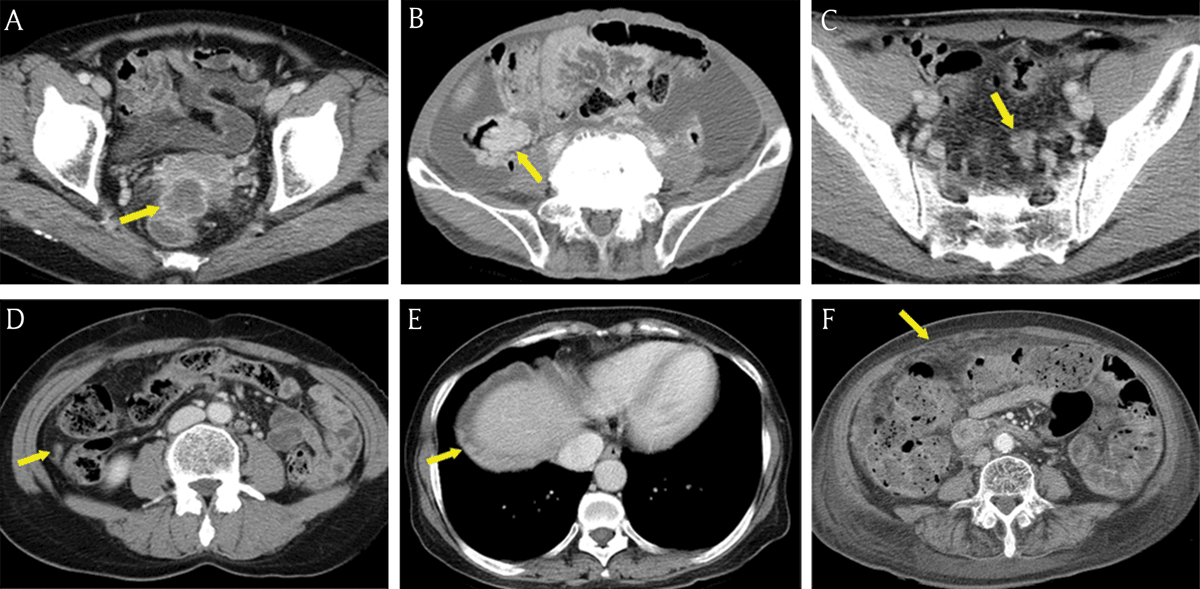
Figure 3
Common seeding sites in peritoneal carcinomatosis. (A–E) Axial portal venous phase CT images show the frequent locations for peritoneal seeding (arrows): peritoneal reflexion (A), lower small bowel mesentery (B), sigmoid mesocolon (C), right paracolic gutter (D), right subphrenic space (E), and greater omentum (F).
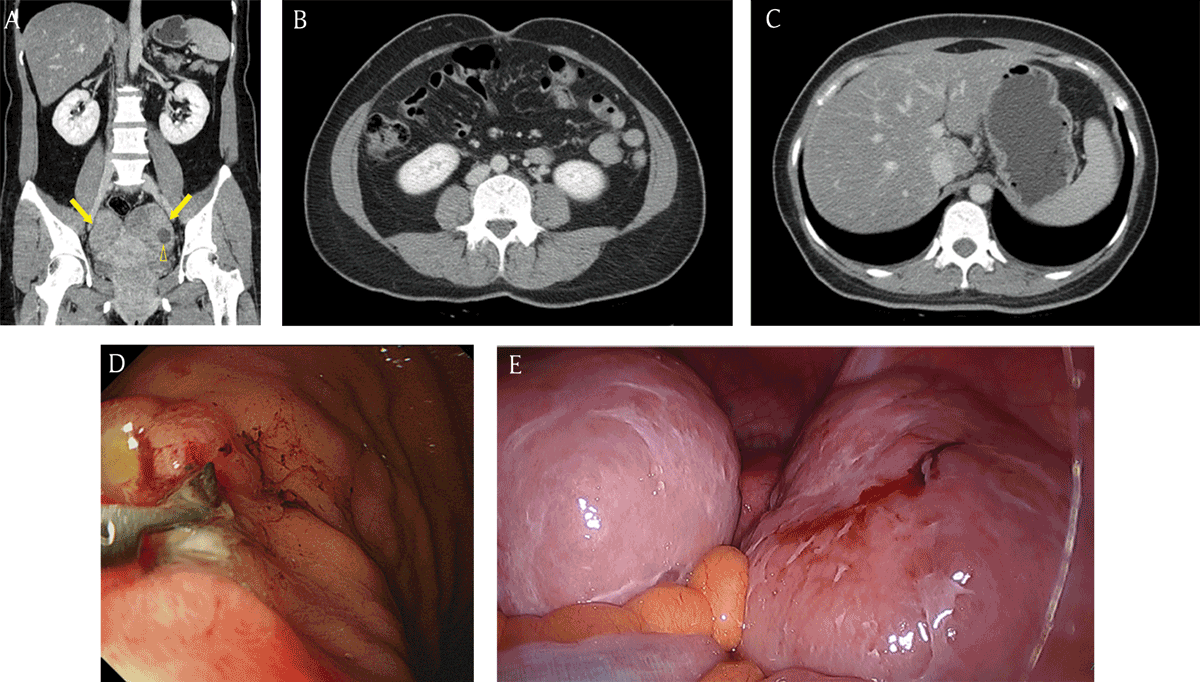
Figure 4
A 40-year-old woman with incidentally detected bilateral ovarian masses. (A) Coronal reformatted contrast-enhanced CT image demonstrated the heterogeneous enhancing masses (arrows) in the bilateral ovaries. Note the small cystic component (open arrowhead) within the ovarian mass. (B, C) There was no evidence of ascites, peritoneal thickening, abnormal lymph nodes, or a malignant tumor within an intra-abdominal solid organ or the gastrointestinal tract on the CT image. (D) Gastric adenocarcinoma with signet ring cell component was confirmed by endoscopy. (E) After surgical resection, the masses were diagnosed as Krukenberg tumors. Other peritoneal seeding lesions were detected in the surgical field.
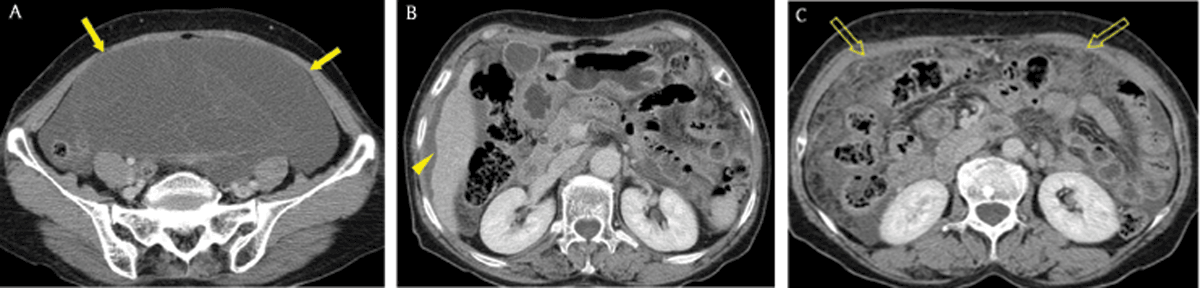
Figure 5
A 66-year-old woman with pseudomyxoma peritonei caused by appendiceal mucinous carcinoma. (A, B) Axial portal venous phase CT images showed fluid collection (arrows) with septa in the peritoneal cavity. Note scalloping of the liver surface (arrowhead) which implied extrinsic pressure by fluid in the perihepatic space. (C) Omental haziness (open arrows) was also detected.
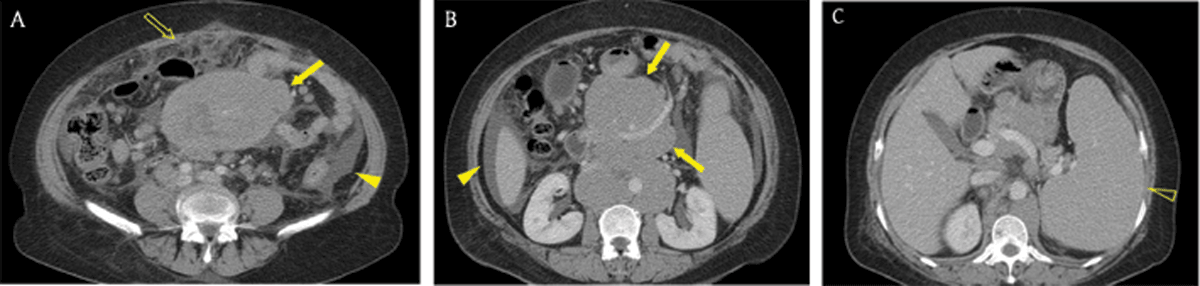
Figure 6
A 60-year-old woman with mantle cell lymphoma. (A, B) Axial portal venous phase CT images revealed omental haziness (open arrow) and ascites (arrowhead). Confluent and bulky lymphadenopathy (arrows) was located on both sides of the mesenteric vessels, representing the ‘sandwich sign’. (C) The size of the spleen (open arrowhead) was increased.
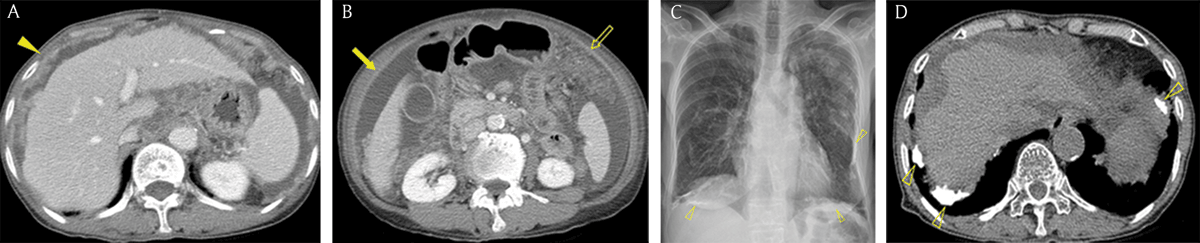
Figure 7
An 80-year-old woman with peritoneal malignant mesothelioma who had a history of asbestos exposure for more than 20 years. (A, B) Axial portal venous phase abdominal CT images showed multiple nodules (arrowhead), peritoneal thickening (arrow), ascites, and omental haziness (open arrow), findings that mimicked peritoneal carcinomatosis. (C) Chest radiograph demonstrated pleural opacities (open arrowheads) in the bilateral hemithorax. (D) An axial unenhanced chest CT image demonstrated multiple calcified plaques (open arrowheads) in both pleura.
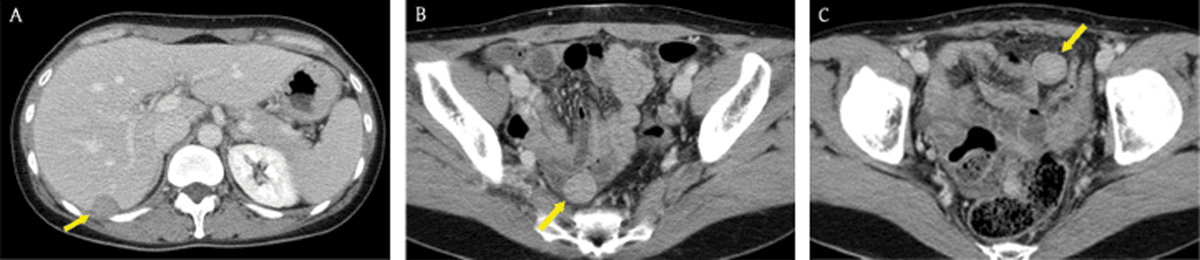
Figure 8
A 39-year-old woman whose surgical history included hysterectomy for uterine leiomyoma. Axial portal venous phase CT images showed multiple, well-circumscribed, solid masses (arrows) with mild-to-moderate enhancement in the peritoneal cavity. There were no abnormal lymph nodes, ascites, or omental haziness in the abdomen. The patient was diagnosed with leiomyomatosis peritonealis disseminata through percutaneous core needle biopsy under ultrasonography guidance.
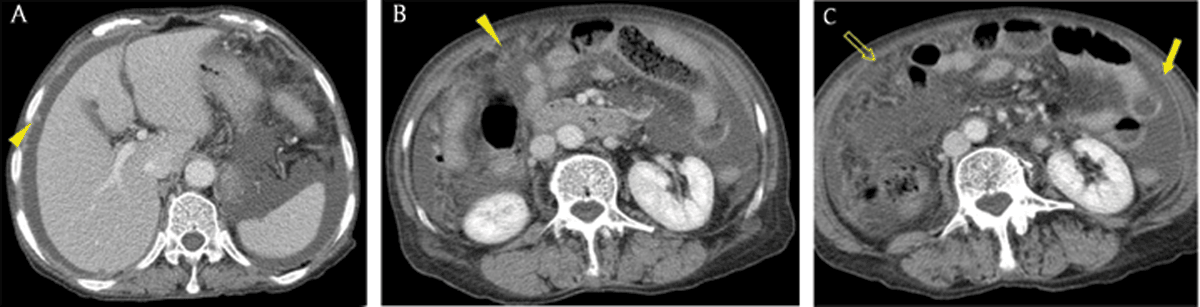
Figure 9
A 74-year-old woman with tuberculous peritonitis. Axial portal venous phase CT images showed multiple nodules (arrowheads), diffuse peritoneal thickening (arrow), ascites, and omental haziness (open arrow), findings that mimicked peritoneal carcinomatosis.
