
Figure 1
Case 1 – Conventional radiographs of the right fifth finger in a nine-year-old boy. Oblique view taken five years prior to the current admission (a). The lesion (arrow in a) was originally interpreted as a non-ossifying fibroma. Lateral (b) and anteroposterior (AP) view at current admission (c). The lesion has grown and consists of two components. The largest juxta-cortical and exophytic part causes pressure erosion of the dorsal cortex, which is thinned and focally destructed with overhanging edges (arrow in b). There is an associated soft tissue swelling. The smaller intramedullary part consists of a well-delineated radiolucent lesion with sclerotic borders. The latter is best seen on the AP view (arrow in c).
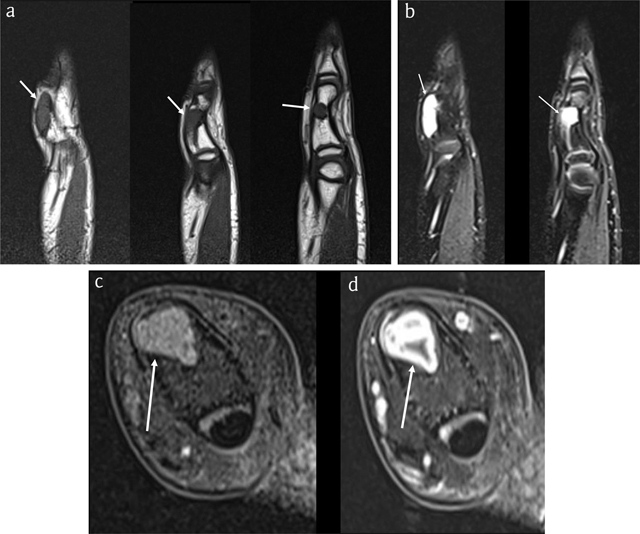
Figure 2
Case 1 – MRI. Sagittal T1-WI (3 adjacent slices) (a). Sagittal fat-suppressed (FS) T2-WI (2 adjacent slices) (b). Axial FS T1-WI (c). Axial FS T1-WI after intravenous administration of gadolinium contrast (d). The lesion is isointense to muscle on T1-WI (arrows in a) and hyperintense on FS T2-WI (arrows in b) and enhances peripherally, in keeping with chondroid matrix (arrow in d).
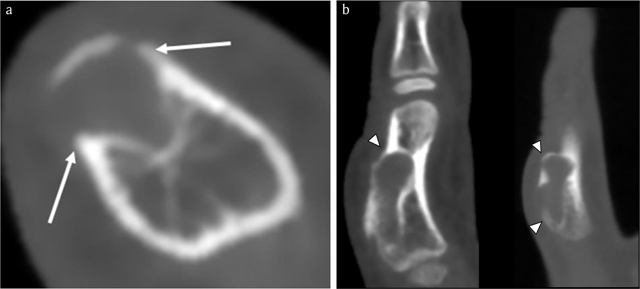
Figure 3
Case 1 – CBCT. Axial image (a). Sagittal reformatted images (2 adjacent slices) (b). Note an expansile radiolucent lesion at the dorsal phalangeal cortex with sclerotic borders (arrows in a). The smaller intramedullary and a larger exophytic components of the lesion are clearly depicted. The cortex is thinned and partially destructed with overhanging edges (arrowheads in b).
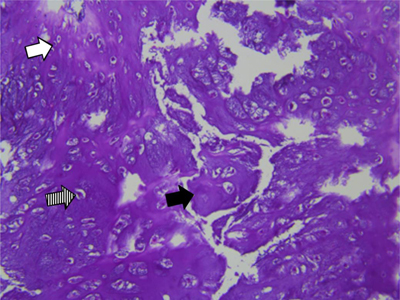
Figure 4
Case 1 – Histopathology of the resected specimen. Hematoxylin eosin staining, 200×:cartilaginous tissue with moderate cellularity. Note chondroid matrix (black arrow) with interspersed small (white arrow) to medium sized (dashed arrow) chondrocytes with no atypia or mitotic activity. There is absence of necrosis.

Figure 5
Case 2 – Clinical photograph of the right hand in a 59-year-old woman, showing a swelling at the dorso-ulnar aspect of the third finger (arrow).

Figure 6
Case 2 – Conventional radiographs of the right third finger. AP (a) and lateral view (b). Note a juxta-cortical radiolucent lesion at the dorso-ulnar aspect of the middle phalanx. The smaller intramedullary part is well-delineated and surrounded by a rim of sclerosis (arrow in a). The larger exophytic component consists of a bony protuberance with adjacent soft tissue swelling (arrowhead in b). There is focal breakthrough of the cortex (dotted arrow in a).
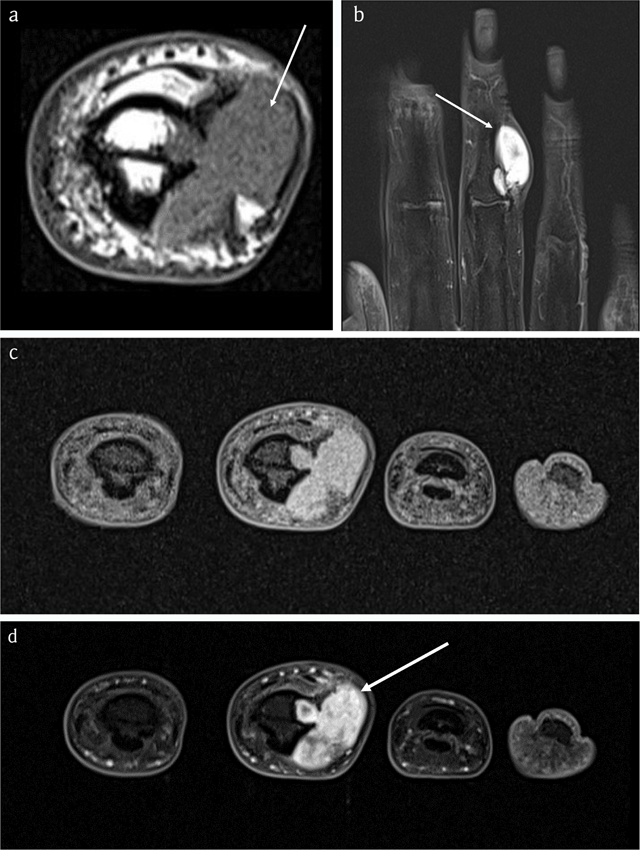
Figure 7
Case 2 – MRI. Axial T1-WI (a). Coronal FS T2-WI (b). Axial FS T1-WI (c). Axial FS T1-WI after administration of gadolinium contrast (d). The lesion is isointense to muscle (arrow in a) and hyperintense on FS T2-WI (arrow in b) with ring-and-arc enhancement (arrow in d), in keeping with chondroid matrix.
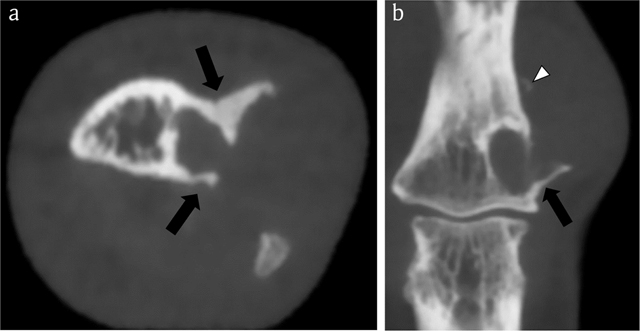
Figure 8
Case 2 – CBCT. Axial image (a). Coronal reformatted image (b). The lesion consists of a smaller intramedullary and a larger juxta-cortical component. The intramedullary part is well-delineated by a rim of peripheral sclerosis, whereas the juxta-cortical part causes scalloping of the outer cortex within overhanging edges (black arrows in a and b). The cortical breakthrough and overhanging margins are far better demonstrated than on CR (see Figure 6). Note a small fleck of calcification (white arrowhead), supporting the hypothesis that the lesion contains chondroid matrix.
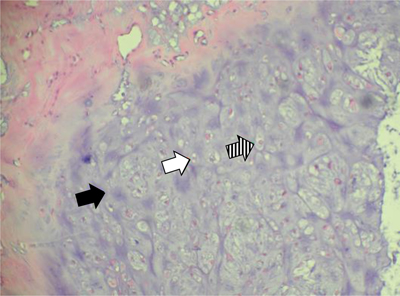
Figure 9
Case 2 – Histopathology of the resected specimen. Hematoxylin eosin staining, 200×: cartilaginous tissue with moderate cellularity. Note chondroid matrix (black arrow) with interspersed small (white arrow) to medium sized (dashed arrow) chondrocytes with no atypia or mitotic activity. There is absence of necrosis.
