Table 1
SWOT analysis for community hospitals in Singapore.
| STRENGTHS | WEAKNESSES |
|---|---|
| - Integrated care model with acute hospitals. - Close proximity to acute care for higher acuity for community hospitals that are co-located with acute hospitals. - Lower cost of care to healthcare system compared to acute hospitals. - Greater expertise in rehabilitation care and discharge planning amongst the multidisciplinary team. | - Wide variation in clinical capabilities across community hospitals, especially between co-located and standalone community hospitals without a neighbouring acute hospital partner. - Discharge delays due to social and logistical issues such as lack of rehabilitation potential or inadequate community support. - Disparity in access to advanced imaging across community hospitals - Reduced patient-clinical team ratio (including nurses and doctors) compared to acute hospitals. - Perceived unattractiveness for healthcare care professionals to work in community hospitals compared to acute hospitals. - Limited care capabilities in community hospitals necessitate the transfer of patients with deteriorating clinical conditions back to acute hospitals for advanced medical management. - Fragmented electronic health records (EHR) between acute and community hospitals slow down patient transfers and decision-making. |
| OPPORTUNITIES | THREATS |
| - Expansion of clinical capabilities to manage emerging clinical issues to minimise re-admissions to acute hospitals. - Subsidy expansion and improved access for all appropriate advanced imaging. - Direct admissions from community. - Increased collaboration with community partners. - Leveraging machine learning for early patient identification and propensity scoring to streamline admissions, optimise bed use, and improve care transitions. - Research on reducing re-admissions and improving outcomes. | - Expansion of clinical capabilities in community hospitals depends on securing adequate staffing resources to manage the anticipated increase in clinical workload. - Process inefficiencies remain as potential roadblocks to expanded care models, particularly the complex procedures for patient transfers and the complicated workflows requires to access acute hospitals’ imaging and laboratory services. - Greater demand and more complex care as population ages. - Current funding models are insufficient to support the expanding scope and enhanced capabilities expected of community hospitals. |
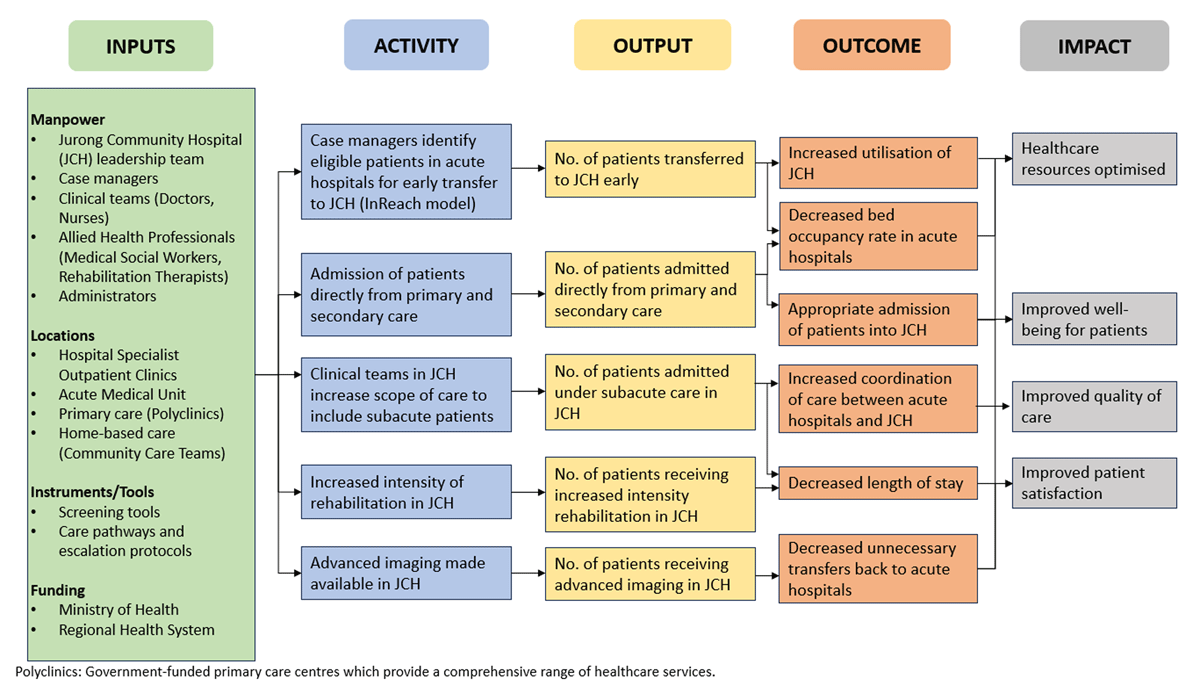
Figure 1
CHoF’s adapted programme theory to integrate care for the population.
