Table 1
Service modalities supporting care continuum in Catalonia.
| SERVICE MODALITIES | CHARACTERISTICS |
|---|---|
| Primary Care | |
| Primary Health Centers | Are the first point of contact for individuals seeking healthcare services and coordinate patients’ cure and/or care. |
| Home Care | Home-based support services directly provided by the primary care center |
| Intermediate Care (socio-health services) – Outpatient regime | |
| Specialized support teams | 1. UFISS – Professionals (physician, nurse, and social worker) devoted to assessment of complex geriatric cases. Ascribed to intermediate care hospitals. 2. EAIA – Dedicated to detection and management of multimorbid patients with high social risk showing acute clinical episodes. 3. ETODA – Stands for outpatient direct observation therapy teams devoted to a specific program for tuberculosis therapy. The aim is to guarantee the correct performance of the treatment by patients with social problems, through the direct supervision of the administration of the medication. |
| Palliative care (PADES) | Interdisciplinary teams, coordinated with the primary care center, devoted to end-of-life care with a holistic approach. |
| Socio-health day hospitals | The objectives of day care services are assessment and comprehensive treatment, rehabilitation and ongoing maintenance care targeting geriatric or multimorbid patients. |
| Intermediate Care (socio-health services) – Hospitalization | |
| Long stay units | For rehabilitative treatment, maintenance care and prevention of complications, and as support for elderly people with long-term chronic diseases that have generated functional disabilities. |
| Convalescence units | Mid-stay unit to restore the functions or activities affected by health problems in geriatric multimorbid patients needing functional recovery after undergoing a surgical, medical, or traumatic process. |
| Sub-acute care units | For people with chronic and advanced disease who, due clinical exacerbation, need the continuation of a treatment under continuous clinical supervision. The aim of this care is to achieve clinical stabilization and comprehensive rehabilitation |
| Palliative care units | End-of-life hospitalizations |
| Hospital Care – Hospital at Home | |
| Full (Hospital Avoidance) or partial (Early Discharge) substitution of conventional in-patient admission by home hospitalization (administered by hospital-based professional teams) for patients showing clinical criteria of hospitalization due to an acute health event. | |
| Social Support | |
| Interdepartmental Plan of Social and Health Interaction approved in 2014. Further developed in [23] | |
[i] UFISS: Functional Unit for Socio-health care; EAIA: Integrated Care Team for specific target groups; ETODA: Team Directly Supporting Therapy on Outpatient basis.
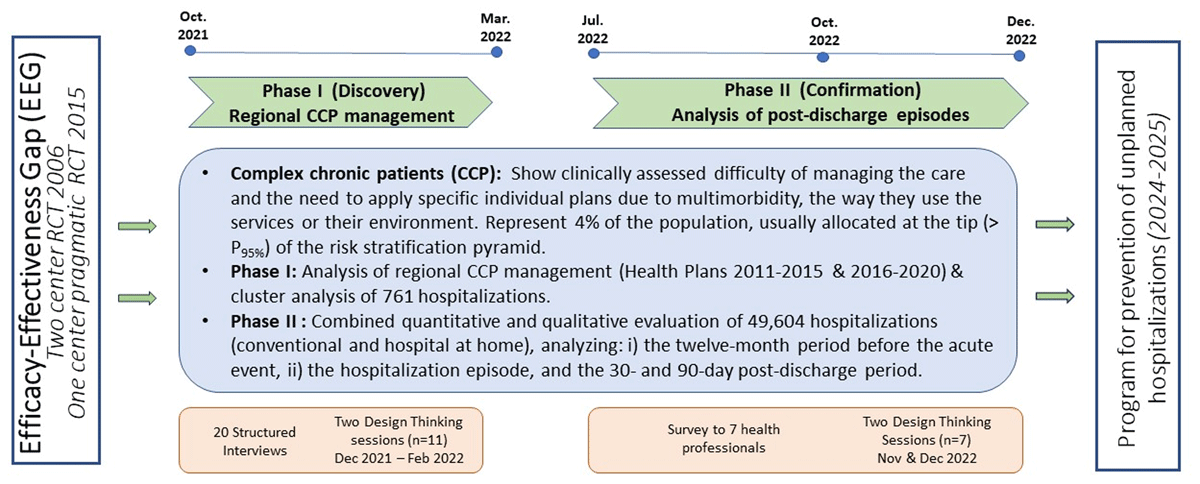
Figure 1
Two-phase co-design process timeline – A trigger: The efficacy-effectiveness gap (EEG) seen between two studies carried out in 2006 [6] and 2015 [12]. The Discovery phase: devoted to the analysis of regional Complex Chronic Patients (CCP) management and identifying the main explicable factors for the EEG. CCP represent 4% of the population, allocated above P95 of the population-based risk stratification pyramid. The Confirmation phase, assessing value generation of Hospital at Home, was used to analyse the interactions between the hospital teams and community-based services, reflecting the status of vertical integration [26]. The final outcome is the elaboration of a program for preventing unplanned hospitalizations to be tested during the period 2024–2025. DT: Design Thinking. RCT: Randomized controlled trial.

Figure 2
Radar plots of the main characteristics of the four clusters of patients identified in [25]. All the features are normalised and grouped into seven categories: i) age; ii) medical complexity; iii) functional capacity; iv) social frailty; v) unhealthy lifestyle habits; vi) use of healthcare resources; and vii) acute episode complexity. The mortality rates, hospital admissions and emergency room (ER) visits are displayed in red.
Table 2
Actions to be included in the program for prevention of unplanned hospitalizations.
| ACTIONS | COMMENTS |
|---|---|
| 1. CHANGE MANAGEMENT | |
| 1.1. Define flexible clinical processes with a holistic approach. | Design the framework of the clinical process considering: i) clinical endpoints, actions associated to main diagnosis and co-morbidities, as well as environmental and social factors. |
| 1.2. Define roles and profile of the advanced care nurse | Key roles are: i) patients’ empowerment for self-management, ii) care and cure actions following plans defined in 1.1, iii) early detection/management of exacerbations. Double ascription to primary care & Hospital at Home teams. Coordination with intermediate care service modalities |
| 1.3. Integrate primary to quaternary preventions | Evolution from current focus on primary prevention to integration of all prevention levels in the management of the program candidates |
| 1.4. Redefine interactions between nurse and patient | Initial motivational intervention followed by patient’s agreements on a personalized care plan (non-pharmacological interventions). Patient’s activation and empowerment following the procedures reported in [3233] |
| 1.5. Training programs for professionals and patients | Education/training of professionals and patients before the program initiation following the innovative approaches reported. |
| 2. PERSONALIZATION OF THE INTERVENTIONS | |
| 2.1 Service selection | Selection of the patient as candidate to the program or allocation into other service modalities indicated in Table 1 |
| 2.2. Harmonize disease- vs patient-oriented approaches. | The intervention (personalization of the clinical process) must consider the individual diseases (type, severity, and progress), as well as their potential interactions (also regarding pharmacological aspects). |
| 2.3. Consider social and environmental factors | The holistic approach of the intervention requires consideration of the non-clinical aspects (social status, education level, environment, etc…) that may have influence on health status |
| 2.4. Consider evolution of health status overtime | The characteristics of the intervention decided in the initial evaluation requires adaptation to the progress of the patient’s condition. The balance between cure and care should be considered. |
| 3. MATURE DIGITAL SUPPORT | |
| 3.1. Adaptive Case Management (ACM) | Combinations of multiple factors influencing the patient’s health status, and unexpected events (exacerbations), requires flexible management of the clinical process which can be achieved with an ACM approach. |
| 3.2. Communication Channel | A communication channel based on chat (including intelligent chatbots) with multimedia support is essential to provide proactive interactions among stakeholders. |
| 3.3. Collaborative work | Digital support to collaborative work among professionals and with patients across healthcare tiers in a must for executing share care agreements. |
| 3.4. Capture of patient’s self-tracking data | Efficient patients’ input data from: i) non-disruptive sensors, ii) chat with the advanced care nurse, and/or iii) short questionnaires (with Likert scales) may play a relevant role in decision-making and knowledge generation. |
| 3.5. Ad-hoc integration | Cloud-based technologies with ad-hoc integration with providers’ health information systems is the proposed approach for provision of digital support to the service. |
| 4. APPLICABLE ASSESSMENT IN REAL-WORLD SETTINGS | |
| 4.1. Evaluation of the process of implementation | Evolution of classical tools for assessment of the service deployment (i.e. Consolidated Framework for Implementation Research, CFIR [34] must be adopted to enhance applicability in real-world settings. |
| 4.2. (PROMS)/(PREMS) | Role of sensor measurements (i.e., Heart Rate Variability), info from the chat and short questions (Likert scale) are candidates to substitute classical questionnaires [33353637]. |
| 4.3. User-profiled dashboards | Identification of Key Performance Indicators (KPI) and build-up management dashboards can contribute to service quality assurance over time. |
| AQUAS: | Agency for Health Quality and Assessment of Catalonia |
| CAPSBE: | Consortium of primary health care Barcelona Esquerra |
| CCP: | Complex chronic patients |
| EEG: | Efficacy-effectiveness gap |
| ESCA: | Catalonia health survey |
| HCB: | Hospital Clinic of Barcelona |
| JADECARE: | Joint Action on implementation of digitally enabled integrated person-centred care |
| KPI: | Key performance indicators |
| PROMs: | Patient reported outcomes measures |
| PREMs: | Patient reported experience measures |
| RCT: | Randomized controlled trial |
| WHO: | World Health Organization |
