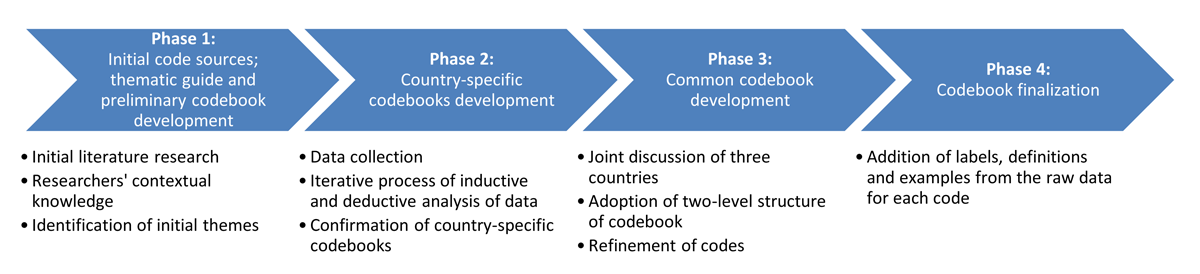
Figure 1
The four-phase process of the codebook for the evaluation of integrated care of arterial hypertension and type-2-diabetes.
Table 1
The characteristics of the data collection. HTN – arterial hypertension; T2D – type-2-diabetes.
| PARTICIPANTS LEVEL | CAMBODIA | SLOVENIA | BELGIUM |
|---|---|---|---|
| Micro | 14 focus groups: four with patients with HTN and/or T2D; five with health care workers; five with community health workers | 15 focus groups: seven with patients with HTN and T2D; eight with health care workers | not performed |
| Meso | 15 interviews | 11 interviews | 15 interviews |
| Macro | 18 interviews | 12 interviews | 13 interviews |
| Time period of data collection: | June 2019–September 2019 | May 2019–April 2020 | April 2019–September 2020 |
Table 2
Comprehensive codebook for evaluation of integrated care for arterial hypertension and type-2-diabetes. HTN – arterial hypertension, T2D – type-2-diabetes [33].
| THEME | DEFINITION |
|---|---|
| 1. Governance | the process of establishing and implementing principles, structures, and policies to effectively guide and regulate the actions and decisions within a particular system or organization |
| 1.1. Leadership, accountability and management | the skills, responsibilities, and strategies required to inspire, guide, and oversee individuals and resources towards achieving goals while upholding transparency and taking ownership for outcomes. |
| 1.2. Decision-making process | systematic series of steps to making a choice or taking a course of action |
| 1.3. Policy, regulation, strategy | national policy, strategy, and guideline for the prevention and control of HTN and T2D |
| 1.4. Regional and local authorities | designated authority/-ies that has the right to make decisions in an organised political community or in any area of activity at the local level |
| 1.5. Macro-level stakeholders | individuals, groups, or organisations directly or indirectly involved in the macro-level decision-making process (e.g., chambers, national institute of public health, ministry, etc.) |
| 1.6. Stakeholder collaboration | active engagement and cooperative efforts among diverse individuals or groups with a vested interest, fostering shared decision-making and collective problem-solving |
| 1.7. Political interest, commitment and power dynamics | influence, motivations, and actions of political actors within the health care system, highlighting their roles in shaping health care policies, resource allocation, and decision-making processes, which can impact health outcomes and the distribution of healthcare services. |
| 2. Health financing | strategies, mechanisms, and policies employed to generate and allocate financial resources for the provision of healthcare services, ensuring equitable access, sustainability, and efficient utilization of funds |
| 2.1. User financial payment | the amount that is not reimbursed by insurance and is thus paid by the patients (out-of-pocket) |
| 2.2. Budget/Sources of funding | the allocation and management of financial resources to support and sustain operations, projects, or initiatives |
| 2.3. Service provider financial payment | health care system financing (e.g., state budgets, municipal budgets, public health insurance, public pension insurance, voluntary health insurance, non-profit agency budgets, corporate budgets, etc.) |
| 2.4. Health insurance and social protection | establishment of comprehensive coverage and support systems to safeguard individuals and populations against health-related risks, providing financial protection and ensuring access to necessary healthcare services. |
| 3. Organisation of health care | design, structure, and coordination of healthcare services, aiming to optimize the delivery, accessibility, efficiency, and quality of care within a healthcare system |
| 3.1. Primary health care level | foundation level of health care that encompasses essential medical services provided by general practitioners, nurses, and other health care professionals in community-based settings, emphasizing preventive care, health promotion, and basic treatment of common illnesses and injuries |
| 3.2. Secondary and tertiary health care level | level of medical care that involves specialized clinical services provided by medical professionals in hospitals or clinics, focusing on the diagnosis, treatment, and management of specific health conditions and diseases |
| 3.3. Integration throughout the health care continuum | management and delivery of health services to individuals, ensuring they receive a seamless range of health promotion, disease prevention, diagnosis, treatment, disease management, rehabilitation, and palliative care services across various levels and locations within the healthcare system, tailored to their needs throughout their entire lifespan |
| 3.4. Team work | collaborative and coordinated efforts of individuals working together towards a common goal, leveraging their diverse skills, knowledge, and perspectives to achieve optimal outcomes |
| 3.5. Quality of care | ensuring that healthcare services meet the highest standards of safety, effectiveness, efficiency, equity, and patient-centeredness, resulting in improved health outcomes and patient satisfaction |
| 3.6. Following guidelines, protocols | adherence to established standards, evidence-based guidelines, and predefined protocols to ensure consistent, safe, and effective delivery of care and treatment to patients |
| 4. Health workforce | individuals involved in providing healthcare services, including professionals, support staff, and volunteers, who contribute to the promotion, prevention, treatment, and management of health conditions |
| 4.1. Health care workers/Non-health care workers | individuals employed in various roles within health care system |
| 4.2. Administration | management and oversight of organizational, financial, operational, and logistical aspects to ensure the efficient functioning and coordination of healthcare services and resources. |
| 4.3. Time burden | excessive time constraints and pressures experienced by health care providers (e.g., workload, administrative tasks, and limited resource availability) |
| 4.4. Burnout | physical, emotional, and mental exhaustion, as well as the feelings of depersonalization and reduced personal accomplishment, resulting from chronic work-related stress and overwhelming demands within the healthcare profession. |
| 4.5. Task sharing (formal and informal) among team members | formal and informal distribution of responsibilities, duties, and tasks within a healthcare team |
| 4.6. Education, training | acquisition and development of knowledge, skills, and competencies through formal and informal learning processes, aiming to enhance the professional capabilities and performance of health care practitioners |
| 5. Patients | individuals seeking or receiving health care services |
| 5.1. Patients’ attitude | emotions, beliefs, behaviors, and perceptions exhibited by individuals towards their health care experiences, providers, and treatment |
| 5.2. Patient empowerment | process of equipping individuals with the knowledge, skills, and confidence to actively participate in their health care decisions, take control of their health, and collaborate with health care providers for improved outcomes |
| 5.3. Lifestyle | habits, behaviors, choices, and activities individuals engage in daily that can influence their overall health, well-being, and susceptibility to certain diseases or conditions |
| 5.4. Accessibility | availability of health care services, facilities, and information, ensuring that individuals can obtain timely and appropriate care (e.g., proximity of health care facilities, affordability of services, availability of transportation, and language interpretation services) |
| 6. Community actors/Community link | engagement, collaboration, and integration of various individuals, organizations, and resources within the community to support and strengthen health care delivery, health promotion, and addressing local health needs |
| 6.1. Patients’ associations | formation of organized groups or associations by patients or their advocates to collectively advocate for their rights, provide support, share experiences, and promote initiatives aimed at improving the quality of care and the well-being of individuals facing specific health conditions or challenges |
| 6.2. Individuals | patients’ individual connections in the community (e.g., spouses, parents, children, friends, neighbours, etc.) |
| 6.3. Informal caregivers | unpaid individuals who provide physical, emotional, or logistical support to individuals with health conditions or disabilities, playing a vital role in their daily care and overall well-being (e.g., volunteers, patients as teachers, etc.) |
| 6.4. Local community | geographic area and its residents, emphasizing their involvement, resources, social networks, and collective efforts in promoting health, addressing health care needs |
| 6.5. Community health workers | trained individuals who are selected from the local community and work as frontline health care providers, delivering essential health care services, health education, and outreach initiatives to community members, particularly in underserved areas. (e.g., peer educators) |
| 7. Collaboration, communication | coordinated and effective exchange of information, ideas, and resources among healthcare professionals, patients, and stakeholders |
| 7.1. Horizontal and vertical collaboration | coordination among different organizations at the same level of health care or within the same sector (horizontal); and coordination across different levels of care or sectors (vertical) |
| 7.2. Between professionals and laymen | collaboration between health care workers and laymen |
| 7.3. Inter-generational | collaboration between different generations |
| 7.4. Intersectoral | collaboration and cooperation among different sectors, such as healthcare, education, social services, and government |
| 8. Pharmaceutical | development, manufacturing, distribution, and utilization of medications and medical products, with a focus on ensuring their safety, efficacy, accessibility, and appropriate use to improve patient health outcomes |
| 9. Health information system | collection, management, storage, analysis, and dissemination of health-related data and information, supporting decision-making, healthcare delivery, and public health interventions |
| 9.1. E-health | digital technologies, information, and communication systems to support and improve health care delivery, access to medical information, and the overall management of health |
| 9.2. Data management system | organization, storage, processing, and utilization of health-related data and information in a structured and secure manner, ensuring accuracy, accessibility, and confidentiality for effective decision-making and healthcare delivery |
| 9.3. Fragmentation | disjointed and disconnected nature of data and information within healthcare systems, hindering effective data sharing, interoperability, and comprehensive analysis |
