
Figure 1
PIP Domains for Integrated Care at the Provincial Level [3336].
Table 1
Practice Demographics (N = 9).
| CHARACTERISTIC | OHT A (n = 3) | OHT B (n = 6) | |
|---|---|---|---|
| Practice Type | Community Health Centre | 1 | 0 |
| Family Health Team | 1 | 6 | |
| Nurse Practitioner-Led Clinic | 1 | 0 | |
| Practice Size | 1–2 employees | 0 | 0 |
| 3–4 employees | 0 | 0 | |
| 5–10 employes | 0 | 0 | |
| Greater than 10 employees | 3 | 6 | |
| Practice Location | Inner City | 0 | 2 |
| Urban | 1 | 3 | |
| Suburban | 1 | 0 | |
| Rural | 1 | 1 | |
| Frontier | 0 | 0 | |
| Length of time integration effort has been active: | Effort is More Than 1 Year | 3 | 6 |
| The mental health clinician(s) in your practice is: | Employed by the practice or practice organization | 3 | 6 |
| How long has there been a mental health clinician as part of the practice? | More than 2 years | 3 | 6 |
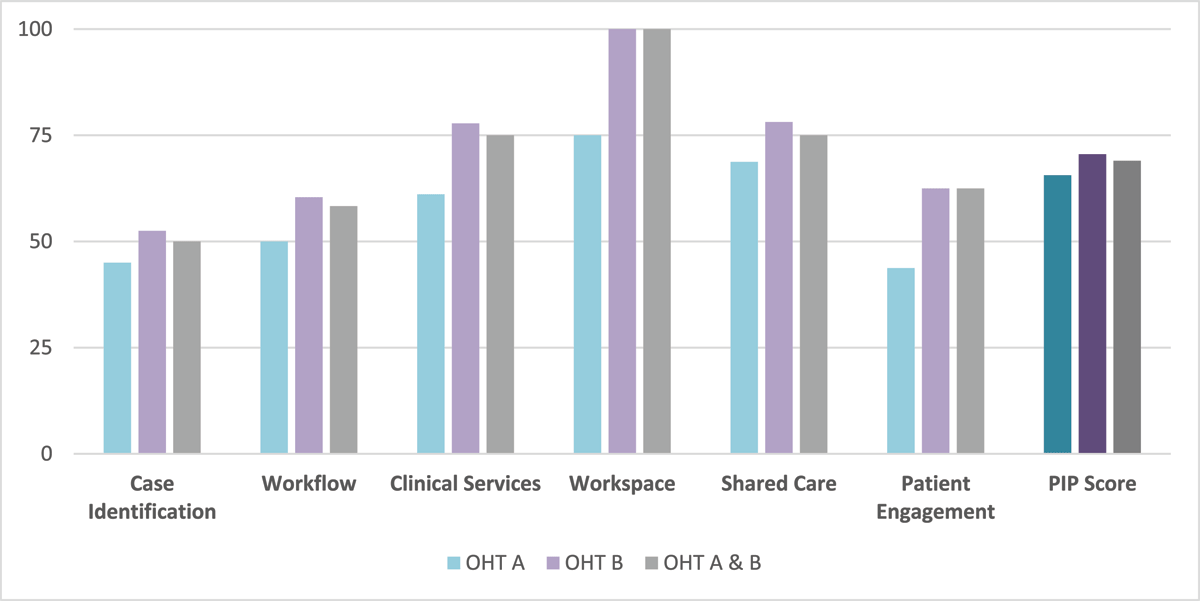
Figure 2
PIP Median Scores by Domain and Overall (N = 9).
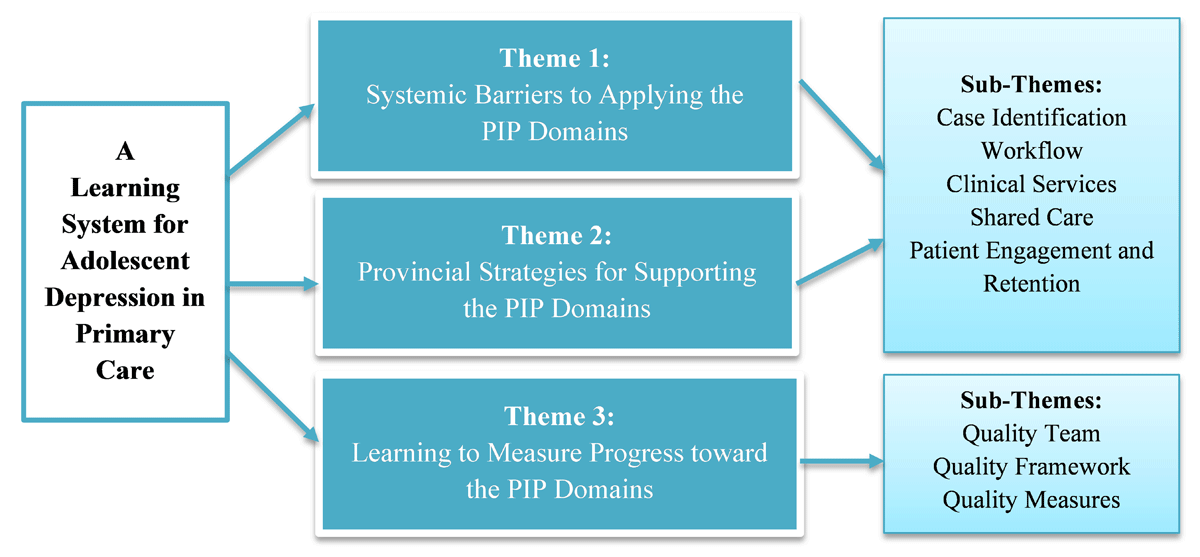
Figure 3
Conceptual Map of the Themes and Sub-Themes from the Focus Group Results.
Table 2
PIP Scores and Number of Focus Group Statements by Domain.
| PIP DOMAINS | MEDIAN SCORES | FOCUS GROUP STATEMENTS |
|---|---|---|
| Case Identification | 50.0 | 37/180 (20.6%) |
| Workflow | 58.3 | 59/180 (32.8%) |
| Clinical Services | 75.0 | 21/180 (11.7%) |
| Shared Care* | 75.0 | 19/180 (10.6%) |
| Workspace | 100.0 | 0/180 (0%) |
| Patient Engagement and Retention | 62.5 | 44/180 (24.4%) |
[i] *Revised definition from the PIP based on focus group results.
Table 3
Comparing PIP Scores of OHT A and OHT B to Focus Group Quotes.
| PIP ITEM | MEAN SCORE | FOCUS GROUP QUOTES |
|---|---|---|
| We have clinicians available on site who provide non-crisis focused mental health services (CS.1). | 3.8 | “So, I think that’s a whole barrier and sets an equity issue for kids that don’t have the opportunities as others for even treatment and care without psychiatry funded at an appropriate amount” (OHT A). |
| We offer prescription medications for routine mental health and substance abuse diagnoses (CS.7). | 3.6 | “You know, they have this limited insurance, so we really try and target treatment within what the parents can afford, because otherwise the options just don’t exist” (OHT B). |
| We have specific systems to identify and intervene on patients who did not initiate or maintain care (PE.3). | 1.3 | “I’ve had psychiatrists where if the patient isn’t willing to follow the medication recommendations that they’re getting, they discharge them. And like, there’s really no follow-up if they decide not to take the medication” (OHT A). |
[i] CS: Clinical Services/PE: Patient Engagement/OHT: Ontario Health Team.
Table 4
Comparing the PIP Mean Scores to the PIP Validation Study Results.
| PIP QUALITY | CASE STUDY | PIP VALIDATION STUDY | ||
|---|---|---|---|---|
| TEAM BASED PRIMARY CARE (n = 9) | PRIMARY CARE (n = 20) | TEAM-BASED PRIMARY CARE (n = 102) | EXEMPLARS (n = 8) | |
| Case Identification | 49 | 43 | 53 | 83 |
| Workflow | 61 | 31 | 55 | 80 |
| Clinical Services | 76 | 23 | 67 | 94 |
| Shared Care | 74 | 18 | 56 | 86 |
| Workspace | 94 | 21 | 77 | 98 |
| Patient Engagement and Retention | 59 | 27 | 51 | 73 |
| Overall | 69 | 27 | 60 | 86 |
Table 5
Key Learnings from the Multi-Case Study of OHTs.
| KEY LEARNINGS | |
|---|---|
| Systemic Barriers | Limited access to mental health expertise within the primary care team and in the community is contributing to the reliance on antidepressants because they’re the most accessible form of treatment, specifically for adolescents without access to private insurance. |
| Strategies | Comprehensive assessments of depressive symptoms, partnerships with high schools and social services in the community and investing in training opportunities for evidence-based therapies could help improve treatment options for adolescent depression. |
| Learning System | A combination of quantitative and qualitative data is needed to support quality integrated for adolescent depression grounded in the frontline experiences of clinicians and patients. |
