Table 1
Inclusion and exclusion criteria for study selection in scoping review.
| Inclusion criteria: |
|---|
|
| Exclusion criteria: |
|
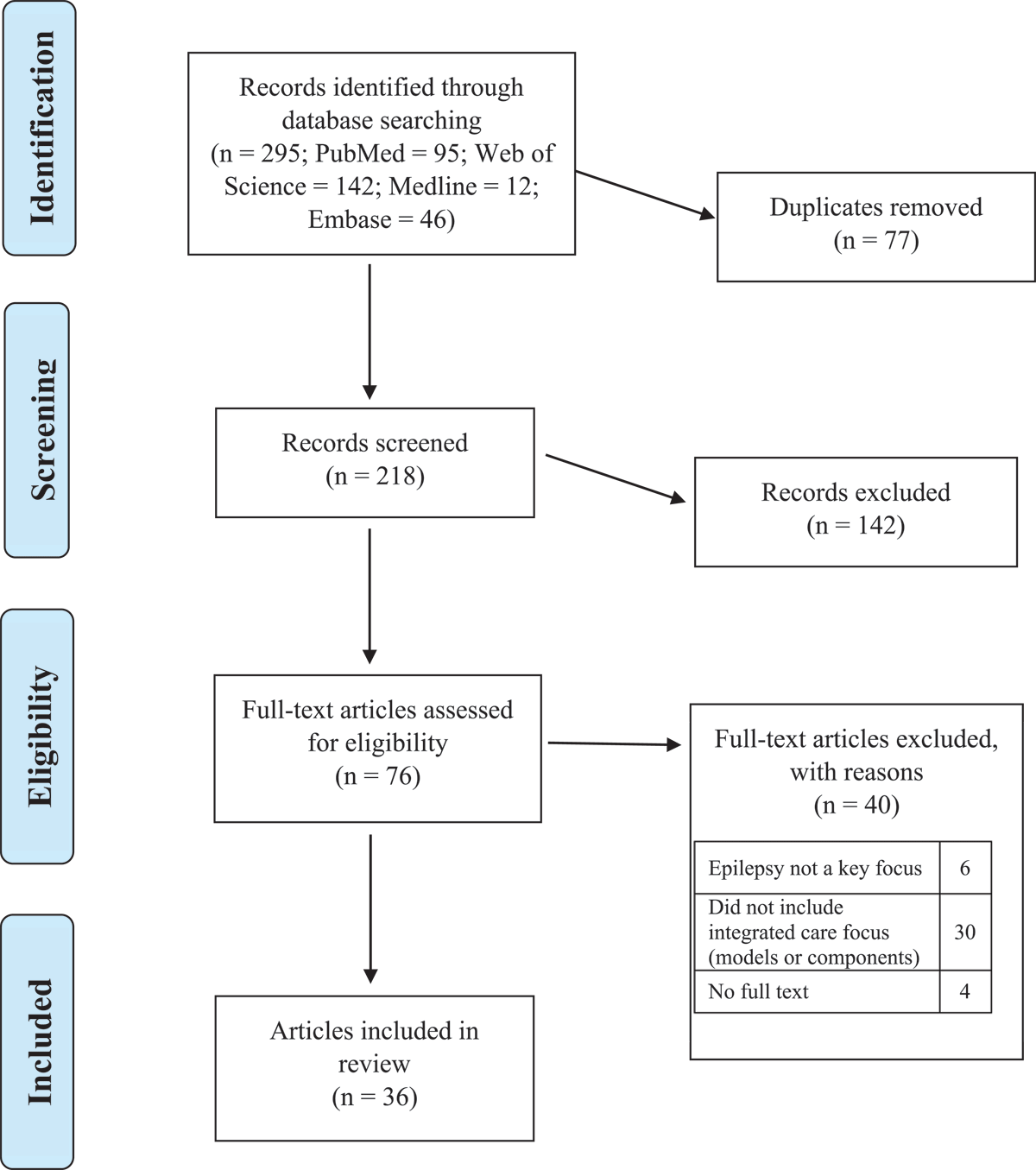
Figure 1
PRISMA flowchart displaying the process of identification and selection of included articles.
Table 2
Frequency of study characteristics included in scoping review.
| STUDY CHARACTERISTICS (N = 36) | n (%) |
|---|---|
| Publication year | |
| 2010–2013 | 6 (17) |
| 2014–2017 | 5 (14) |
| 2018–2022 | 25 (69) |
| Study location | |
| Europe | 21 (58) |
| North America | 11 (31) |
| Australia | 3 (8) |
| South America | 1 (3) |
| Article type or study design* | |
| Descriptive | 16 (44) |
| Literature review | 8 (22) |
| Retrospective cohort | 7 (19) |
| Prospective cohort | 2 (6) |
| Narrative review | 2 (6) |
| Synthesis of expert recommendations | 1 (3) |
| Delphi | 1 (3) |
| Case study | 1 (3) |
| Case series | 1 (3) |
| Implementation or recommendation focus | |
| Refers to implemented model of care | 10 (28) |
| Refers to implemented components, but not full models, of care | 9 (25) |
| Recommends new model of care that is not implemented | 5 (14) |
| Recommends new components, but not full models, of care, that are not implemented | 12 (33) |
| Components of integrated care | |
| Healthcare staff & pathways | |
| Multidisciplinary teams | 22 (61) |
| Cross-sector collaboration | 19 (53) |
| CPGs or care pathways | 13 (36) |
| Epilepsy nurses | 7 (19) |
| Tasks & services | |
| Psychosocial services | 19 (53) |
| Care coordination | 13 (36) |
| Care management plans | 11 (31) |
| Transition services | 5 (14) |
| Surgical evaluation | 3 (8) |
| Education & engagement | |
| Shared decision making | 19 (53) |
| Education for PLWE and families | 15 (42) |
| Education for HCPs | 13 (36) |
| Technology for diagnosis & communication | |
| Shared electronic medical records | 12 (33) |
| Telehealth | 8 (22) |
| Digital health tools | 5 (14) |
[i] N, total number of articles included in scoping review; n, number of articles included in the frequency analysis; CPGs, clinical practice guidelines; PLWE, people living with epilepsy; HCPs, healthcare professionals.
* Three articles utilised more than one type of study design.
Table 3
Implemented models of integrated care in epilepsy management.
| IMPLEMENTED MODEL | COMPONENTS* |
|---|---|
| National Clinical Programme for Epilepsy [424647484950] |
|
| Epilepsy nurse-led model [42] |
|
| Integrated care pathway for seizure management in emergency department [4647] |
|
| Integrated care pathway for homeless PLWE [41] |
|
| Urgent epilepsy clinic [43] |
|
| Neurocare service [44] |
|
| Children and Young People’s Health Partnership Evelina London Model [45] |
|
[i] *As reported within relevant articles; MDT, multidisciplinary team; PLWE, people living with epilepsy; HCP, healthcare professional; EN, epilepsy nurse; CPGs, clinical practice guidelines; CMPs, care management plans; SDM, shared decision-making; EMR, electronic medical record.
Table 4
Models of integrated care in epilepsy management that were recommended but not implemented.
| RECOMMENDED MODEL | COMPONENTS* |
|---|---|
| Hub-and-spoke [36] |
|
| Integrated care for children and young people [37] |
|
| Chronic disease management [38] |
|
| Paediatric acute seizure care pathway [39] |
|
| Model of transition (paediatric to adult) [40] |
|
[i] *As reported within relevant articles; HCP, healthcare professional; MDT, multidisciplinary team; PLWE, people living with epilepsy; EN, epilepsy nurse; CPGs, clinical practice guidelines; CMPs, care management plans; SDM, shared decision-making; EMR, electronic medical record.
Table 5
Integrated care components across implemented and recommended models.
| HEALTHCARE STAFF & PATHWAYS | TASKS & SERVICES | EDUCATION & ENGAGEMENT | TECHNOLOGY FOR DIAGNOSIS & COMMUNICATION | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDT | CROSS SECTOR COLLABORATION | CPG & CARE PATHWAYS | ENS | PSYCHOLOGICALSERVICES | CARE COORDINATION | CMPS | TRANSITION SERVICE | SURGICAL EVALUATION & SUPPORT* | SDM | EDUCATION FOR HCPS | EDUCATION FOR PLWE & FAMILIES | SHARED EMRS | TELEHEALTH | DIGITAL HEALTH TOOLS | |
| IMPLEMENTED | |||||||||||||||
| % models including relevant component | 100% | 71% | 43% | 29% | 43% | 57% | 71% | 0% | 0% | 57% | 43% | 57% | 57% | 57% | 0% |
| National Clinical Programme for Epilepsy [424647484950] | Y | Y | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | Y | N |
| Epilepsy nurse-led model [42] | Y | Y | N | N | Y | Y | Y | N | N | Y | N | Y | Y | Y | N |
| Integrated care pathway for seizure management in emergency department [4647] | Y | N | Y | Y | N | N | N | N | N | N | Y | N | N | N | N |
| Integrated care pathway for homeless PLWE [41] | Y | Y | Y | N | N | N | Y | N | N | N | N | N | Y | N | N |
| Urgent epilepsy clinic [43] | Y | N | N | N | Y | N | Y | N | N | N | Y | Y | Y | N | N |
| Neurocare service [44] | Y | Y | N | N | N | Y | Y | N | N | Y | N | Y | N | Y | N |
| Children and Young People’s Health Partnership Evelina London Model [45] | Y | Y | N | N | Y | Y | N | N | N | Y | N | N | N | Y | N |
| RECOMMENDED | |||||||||||||||
| % models including relevant component | 100% | 80% | 60% | 20% | 60% | 60% | 60% | 40% | 0% | 80% | 80% | 80% | 60% | 0% | 40% |
| Hub and spoke [36] | Y | Y | N | N | Y | Y | Y | Y | N | Y | Y | Y | N | N | N |
| Integrated care for children and young people [37] | Y | Y | N | N | N | N | Y | N | N | Y | Y | N | Y | N | Y |
| Chronic disease management [38] | Y | Y | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | N | N |
| Paediatric acute seizure care pathway [39] | Y | Y | Y | N | Y | Y | Y | N | N | N | Y | Y | Y | N | Y |
| Model of transition (paediatric to adult) [40] | Y | N | Y | N | Y | N | N | Y | N | Y | Y | N | N | N | |
[i] Y = Yes, N = No, MDT = multidisciplinary team, CPG = clinical practice guidelines, ENs = Epilepsy nurses, CMPs = care management plans, SDM = shared decision making, HCPs = healthcare professionals, PLWE = people living with epilepsy, EMRs = electronic medical records.
*Recommended component of integrated care but currently a stand-alone service and not included within a specific model of care.
