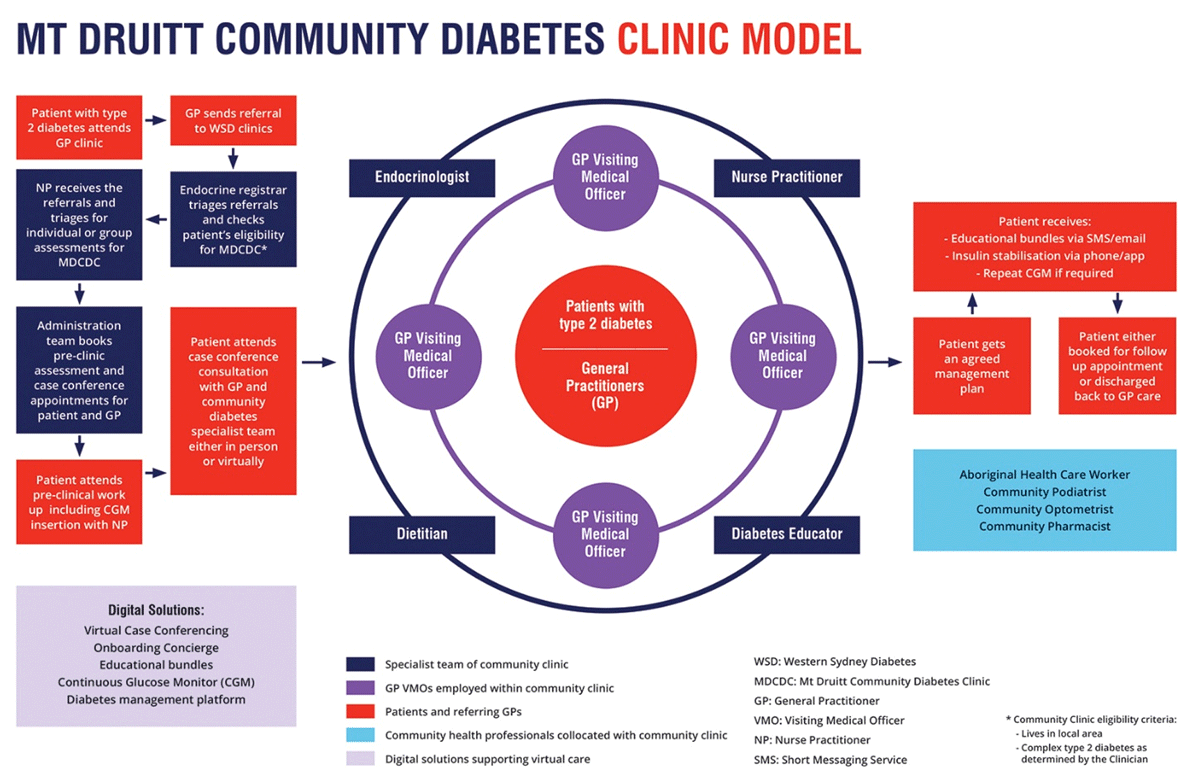
Figure 1
Mt Druitt Community Diabetes Clinic (Integrated care) model.
Table 1
Western Sydney Diabetes Virtual Care suite of digital solutions.
| INTERVENTION COMPONENT | DESCRIPTION |
|---|---|
| Diabetes Case Conference (DCC) including specialist team, referring GPs and patients using myVirtualCare platform (myVC) and new ‘concierge’ service. | DCC aims to build referring GPs’ capacity and agreement with the management plan. myVirtualCare platform, developed by NSW eHealth and Agency for Clinical Innovation, is a custom-built web-based videoconferencing platform that provides secure virtual consultation room and mimics the physical workflow of a clinical consultation. A new ‘concierge’ service to support patients and GPs to trial the myVC platform and be technically ready in joining the virtual waiting room. The concierge administration team send text messages confirming the appointment booking and the link to myVC for virtual consultations. It also supports onboarding of patients and GPs by testing the myVC link, audio-video settings and connections. |
| Education bundles | Short educational videos (2 minutes) created by WSD and fact sheets from nationally renowned bodies to enhance self-management for patients with diabetes |
| Continuous Glucose Monitoring (CGM) | Used for clinic patients to reveal detailed glycaemic profiles over two weeks showing glucose variability (especially hypoglycaemia), evidence of calorie intake and providing insight to patients and providers ways to better use medication and lifestyle changes |
| Diabetes Management platform | Sharing clinical information for care team and self-management application with patients |
Table 2
Interview participants characteristics.
| PATIENT CHARACTERISTICS (n = 10) | n | % |
| Gender | ||
| Male | 4 | 40 |
| Female | 6 | 60 |
| Age group | ||
| Less than 29 | 1 | 10 |
| 30–49 | 3 | 30 |
| 50–59 | 2 | 20 |
| 60 and above | 4 | 40 |
| Education | ||
| High school or less | 5 | 50 |
| Certificate or equivalent | 2 | 20 |
| Undergraduate degree or above | 3 | 30 |
| Country of birth other than Australia | 4 | 40 |
| Language spoken other than English | 4 | 40 |
| Indigenous community | 1 | 10 |
| GP CHARACTERISTICS (n = 5) | ||
| Gender | ||
| Male | 0 | 0 |
| Female | 5 | 100 |
| Country of birth other than Australia | 3 | 60 |
| Language spoken other than English | 3 | 60 |
| Indigenous community | 0 | 0 |
| Practising more than 10 years in Australia as provider | 5 | 100 |
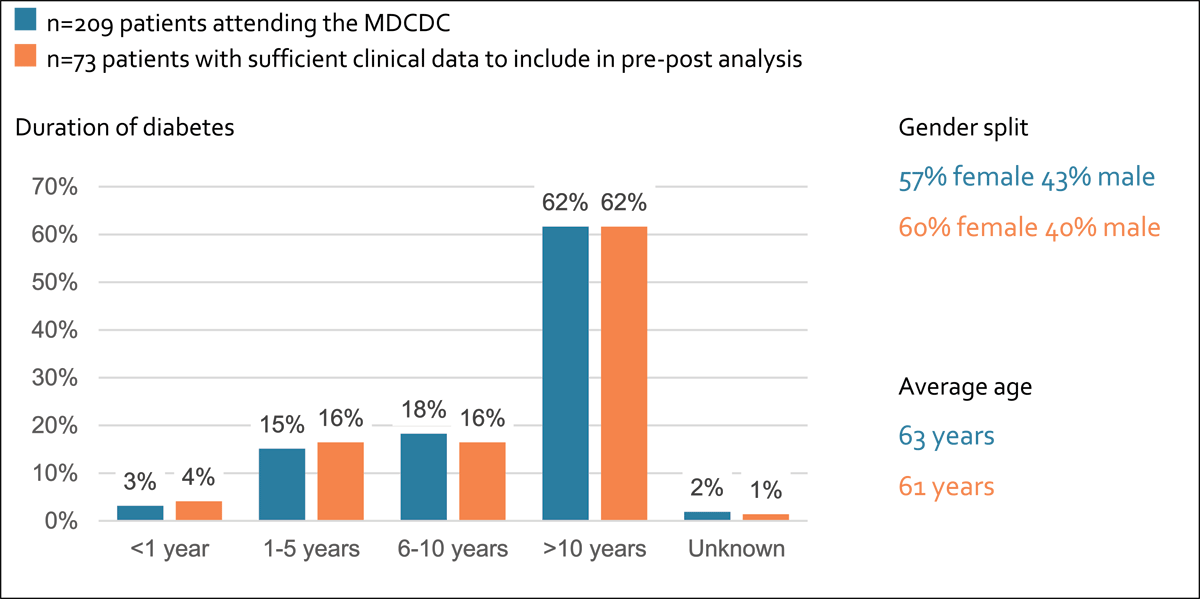
Figure 2
Patient characteristics of total pool and analysis sample.
Table 3
Themes from patients’ interviews.
| PATIENTS’ PERSPECTIVES | SUPPORTING QUOTES |
|---|---|
| THEME 1. PERCEIVED BENEFITS AND STRENGTHS OF THE COMMUNITY CLINIC | |
| “just directing me to the right people…Best for teamwork, team for the doctors, team for me” (Pt01). |
| “I’ve lived in Mount Druitt for 55 years and it’s the best thing that’s ever happened… it’s handy, very, very handy (Pt02). |
| “Anything to keep out of the COVID….I’m one of those ones that my immune system, I get attracted to something that I shouldn’t have…”(Pt02) |
| “they sent me a link and a time to the appointment. And I think, I think it was like a couple of days they rang, they contacted me on how to use it…they’d go through it step by step with me” (Pt06) |
| THEME 2. PERCEIVED CHALLENGES AND LIMITATION OF DELIVERY OF MODALITIES | |
| “I didn’t speak to the doctor face-to-face, because they take it to another level, who takes everything in, all the reports in. And then she comes back and says, ‘this is what the doctor said, and this is how you’ve got to do it” (Pt02). “face-to-face is better… well, then they can tell me what is wrong with me… then they can tell me what they’re talking about in plain English. Not doctor-doctor English” (Pt07). |
| “…I can’t sit in a car for too long…because sometimes I get anxiety…”(Pt02) |
| “maybe train the GPs before, because my GP didn’t know how to connect…she had to ring someone to see how to do it. I just thought maybe they should know before starting up on Virtual” (Pt01) |
| THEME 3. CONFIDENCE WITH DIABETES MANAGEMENT AFTER ACCESSING THE COMMUNITY CLINIC | |
| “they would tell me something and then they would ask, you know, what I thought and, did I understand” (Pt06). “I’ve got the information where I need it and also my doctor can, um, access it whenever” (Pt06) |
Table 4
Themes from providers interviews and focus groups.
| PROVIDERS’ PERSPECTIVES | SUPPORTING QUOTES |
|---|---|
| THEME 1. PERCEIVED STRENGTHS OF THE MODEL | |
| “A small multidisciplinary team is an effective way to deal with complex cases. We are all around the table and deliver the care instantly. Not reliant on email or mail – no bureaucratic hold ups. The group is small and can deliver all the care in one day.”(Clinic staff) |
| “Because you get the input and also get the education…that’s a really valuable thing for me as well, so that with my other patients with diabetes I’m getting much more comfortable using the newer types of medication and understanding where they fit” (GP02). |
| “If the patients goes out to see a specialist and then comes back the care’s much more fragmented, so this, this model provides more of the holistic care… and the patient as seen that the dieticians, or diabetes educator or spoken to them individually, but then they can see everyone working as a team. And I think that’s a positive thing for the patient” (GP02). |
| THEME 2. PERCEIVED CHALLENGES AND LIMITATION OF DELIVERY OF MODALITIES | |
| “I did first video conference for one of the patients, I can connect somehow, but it’s so hard, you know? So three-way conversation. Patient couldn’t hear. I couldn’t hear. Maybe you guys have special software” (GP05). |
| “With this model we are highly reliant on the referring GP. They usually are not expecting that they need to be present at the time. It’s probably 50–50 between GPs who contribute and those that don’t” (Clinic staff). |
| “Our client base is not really tech savvy. You have to call them, and they won’t answer private or blocked numbers. Texting first can really help. Rapport building is key” (Clinic staff). |
| THEME 3. PERCEIVED AREAS OF IMPROVEMENT/REQUESTED IMPROVEMENTS | |
| “The NDSS [National Diabetes Services Scheme] resources are very wordy. I use other ones – Bakers Institute, or ones from Queensland, or I’ve developed my own. Diabetes Australia have good resources. You need things that are visual rather than simple. There are some good exercise resources too” (Clinic staff). |
| “If we could have more of those [continuous] glucose monitors that would be great. They’re a really effective educational tool, raising awareness to trigger self-management and conversations about self-management. Otherwise, this cohort is pretty bad at doing the finger prick thing” (Clinic staff). |
