
Figure 1
Summary of the study design and questionnaires.
HCS, home care services; PHCs, primary health centers; SCS, social care services.
*SCS teams were asked to answer the individualized questionnaire together with PHC teams of their council to the extent possible.
Table 1
Indicators of the five core components of the model.
| COMPONENT 1: “INDIVIDUAL ASSESSMENT OF INTEGRATED SOCIAL AND HEALTH CARE” | |
|---|---|
| 1. | Values and preferences of the person |
| 2. | Functional and instrumental autonomy (basic ADLs, IADLs) |
| 3. | Need for support in decision making |
| 4. | Multidimensional assessment of the needs of the care recipient |
| 5. | Social and family situation and environment |
| 6. | Evaluation of the person’s health situation |
| 7. | Detection of risks related to the person |
| 8. | Protective and resilience factors |
| 9. | Screening for frailty |
| 10. | Safe use of medication at home |
| 11. | Safe use of equipment and other technology in the home |
| 12. | Support and occupational therapy resources |
| 13. | Evaluation of care providers |
| 14. | Conditions of the home |
| 15. | Use of resources and services in the home: remote assistance, home health workers, respiratory physiotherapy, physical/occupational therapy, home oxygen therapy, speech therapy, etc. |
| 16. | Primary support received by the person and family or care providing environment |
| 17. | Existence of an advanced care plan, especially in the case of ACPs |
| 18. | Ethical implications of the care process |
| 19. | Assessment of the person’s quality of life, conducted using a quality-of-life assessment tool or scale |
| 20. | The initial and subsequent assessments of the person meet timing and accessibility requirements |
| COMPONENT 2: “SINGLE INDIVIDUAL PLAN FOR INTEGRATED SOCIAL AND HEALTH CARE” | |
| 1. | The person’s care plan is unique |
| 2. | List of needs or problems that require intervention |
| 3. | Definition of objectives agreed upon with any care providers from other spheres |
| 4. | Specification of the interventions and strategies that will be carried out |
| 5. | Specification of the criteria that will be used to evaluate the results |
| 6. | The plan is jointly prepared with the person and the team |
| 7. | The plan is implemented from the very start of the care service, and it is reassessed within the first 6 weeks and at least once a year |
| 8. | The person can view the plan and keeps the current and up-to-date care plan |
| 9. | The plan includes actions by the professionals from the various disciplines and home services that visit the person at home |
| 10. | The plan is accompanied by a home information file specifying the key agreements and aspects to be taken into account in relation to the care recipient and their family |
| COMPONENT 3: “SHARED PROTOCOLS ACROSS HEALTH AND SOCIAL SERVICES” | |
| 1. | Definition of the systems for organizing the teams according to the territory of action |
| 2. | Collaborative planning of the service among the agents involved |
| 3. | Systems for allocating cases and assigning the workload |
| 4. | Interdisciplinary and multi-agency composition of the services included in the portfolio of the home care teams |
| 5. | Communication and messaging system for the practitioners involved in the care process |
| 6. | Assignment of lead and co-lead caregivers for the person |
| 7. | The team has access to the electronic case tracking system |
| 8. | Existence of agile mechanisms for resolving any differences or conflicts of criteria arising between professionals and organizations |
| 9. | Existence of shared protocols for HCS |
| 10. | Shared care routes for the integrated care service |
| COMPONENT 4: “COORDINATION BETWEEN SOCIAL AND HEALTH MULTIDISCIPLINARY TEAMS” | |
| 1. | Existence and application of a territorial functional plan that ensures the delivery of integrated care |
| 2. | Conducting case conferences planned jointly between the social and health care teams |
| 3. | Responses to enquiries raised between the different parties involved in the care process |
| 4. | Information provided in the person’s transitions between different services |
| 5. | Management of differences of opinion among the teams in accordance with established procedures |
| COMPONENT 5: “INTEGRATED PORTFOLIO OF SERVICES WITH JOINT SOCIAL AND HEALTH HCS PROJECTS” | |
| 1. | Existence of a portfolio of social and health HCS |
| 2. | Description of the catalog of services |
| 3. | Periodic assessment of the programs described in the catalog of services |
| 4. | Existence of a personal platform or folder where the person and caregiver can interact with the key professionals |
[i] ACPs, advanced chronic patients; ADLs, activities of daily living; HCS, home care services; IADLs, instrumental activities of daily living.
Table 2
Scores (0–5) of the screening questionnaire according to the five core components of integrated social and health HCS, answered by SCS and PHC social care professionals. Mean (SD).
| COMPONENTS | SCS (N = 105) | PHC (N = 94) |
|---|---|---|
| Individual assessment of integrated social and health care | 1.2 (1.2) | 2.3 (1.4) |
| Single individual plan for integrated social and health care | 1.2 (1.1) | 1.9 (1.4) |
| Shared protocols across health and social services | 1.3 (1.1) | 1.8 (1.3) |
| Coordination between social and health multidisciplinary teams | 2.0 (1.2) | 2.4 (1.4) |
| Integrated portfolio of services with joint social and health HCS projects | 1.4 (1.3) | 1.8 (1.3) |
[i] HCS, home care services; SCS, social care services; PHC primary health center.
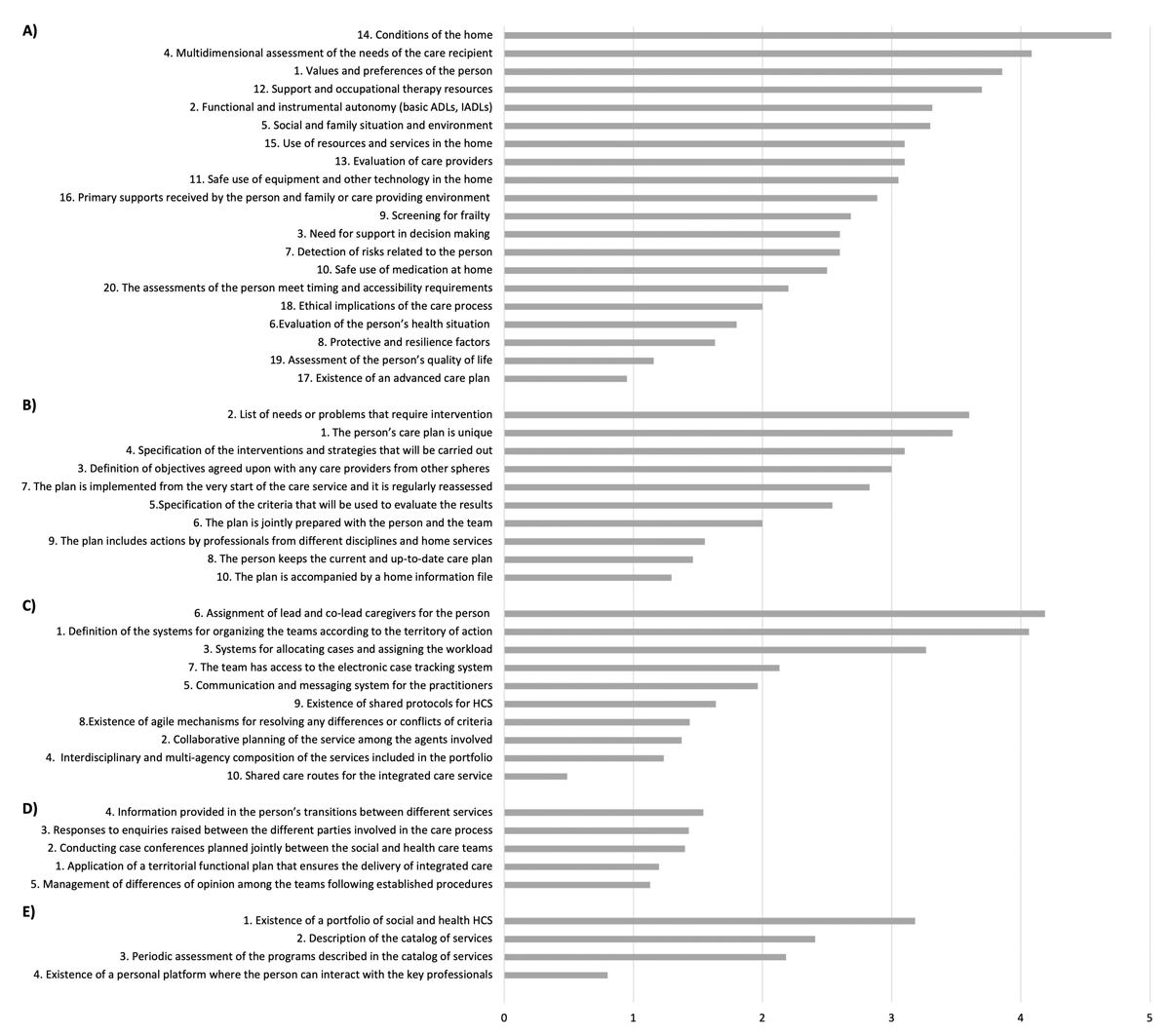
Figure 2
Mean scores of the indicators for each of the five core components of an integrated care model: A) “individual assessment of integrated social and health care” (n = 21); B) “single individual plan for integrated social and health care” (n = 18); C) “shared protocols across health and social services” (n = 17); D) “coordination between social and health multidisciplinary teams” (n = 19); E) “integrated portfolio of services with joint social and health HCS projects” (n = 11). Indicators are ordered from highest to lowest mean scores obtained from the individualized questionnaires answered by social care professionals.
Table 3
Main perceived barriers and facilitators of integrated HCS according to the responses of the screening and customized questionnaires by SCS (n = 105) and PHC (n = 94) social care professionals, N (%).
| BARRIERS | |
|---|---|
| Lack of shared protocols and culture of coordination between social and health care systems | 93 (46.7) |
| Lack of staff, leadership, and responsibility | 91 (45.7) |
| Lack of shared information procedures between social and health care systems | 60 (30.1) |
| Lack of agreement and differences between social and health care professionals; work pressure | 50 (25.1) |
| Fragmentation and different territorial organization between social and health care systems | 23 (11.6) |
| Services portfolio not shared between social and health care systems; HCS limitations | 22 (11.1) |
| Barriers for user assistance: duplicity, bureaucracy, complexity, and COVID-19 pandemic | 18 (9.0) |
| Lack of resources and services | 16 (8.0) |
| Data Protection issues that make difficult data collection and sharing | 12 (6.0) |
| Lack of training regarding the integrated care program; lack of importance of social assessment in the health care field | 9 (4.5) |
| FACILITATORS | |
| Good attitude, competence, and acknowledgment of the need for an integrated care approach by social and health care professionals | 162 (81.4) |
| Previous experience in collaboration and common methods for networking | 81 (40.7) |
| Small size of the territory of action and the community network | 33 (16.6) |
| Cooperation of the users and their family members; social and health systems work with the same persons | 12 (6.0) |
| Good attitude towards collaboration between social and health care systems | 12 (6.0) |
| Specific training on the integrated HCS program | 10 (5.0) |
| Technology tools that promote data sharing | 9 (4.5) |
| Increased funds and creation of spaces for HCS | 8 (4.0) |
| Regulation for the integration of social and health data | 4 (2.0) |
| Unification of HCS with shared funds between social and health care systems | 1 (0.5) |
[i] COVID-19, coronavirus disease 2019; HCS, home care services. SCS, social care services; PHC, primary health center.
