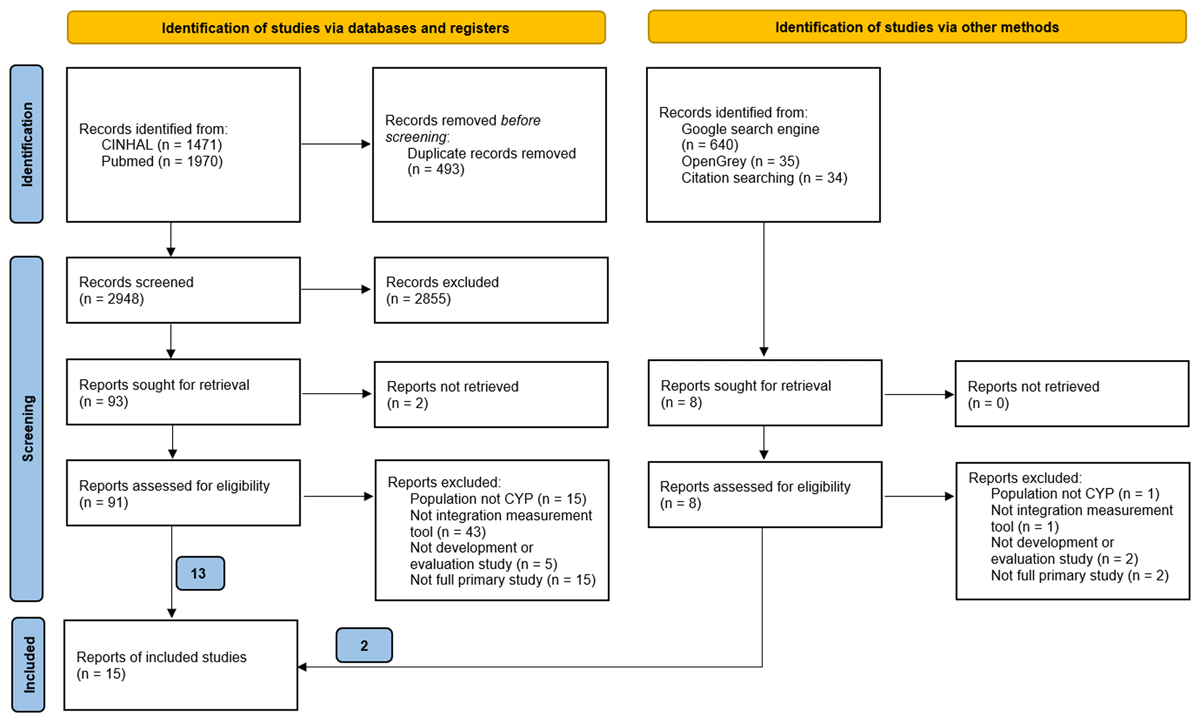
Figure 1
PRISMA diagram of the study selection process for instruments measuring integration within children and young people healthcare systems.
Table 1
Descriptions of instruments (n = 16) measuring integration within children and young people healthcare systems by outcomes measured.
| MEASUREMENT INSTRUMENTS | TYPE OF MEASUREMENT INSTRUMENT | DESCRIPTION OF MEASUREMENT INSTRUMENTS |
|---|---|---|
| Outcome: Quality of care coordination | ||
| Primary Care Assessment Tool (PCATool Brazil) [36]*† (Also measures Completeness of care and Structure of care) | Questionnaire (completed by HCPs) |
|
| Bice-Boxerman Continuity of Care index (indicator of quality of CC) [24] | Simple administration method (from visit records) |
|
| Caregiver’s survey [25]* | Questionnaire (completed by caregivers) |
|
| Care-coordination Measurement Tool (CCMT) [23] | Simple administration method (from visit records) |
|
| Family Experiences of Coordination of Care (FECC) [2628] | Questionnaire (completed by caregivers) |
|
| Framework for evaluating patient care communication [31]*† (Also measures Quality of communication) | Three stage process: 1) Questionnaire (completed by caregivers), 2) Interviews (with caregivers) and 3) Focus Groups (with HCPs) |
|
| The Paediatric Integrated Care Survey (PICS) [30]† (Also measures Completeness of care) | Questionnaire (completed by caregivers) |
|
| Outcome: Quality of collaboration | ||
| Collaborative Care for Attention-Deficit Disorders Scale (CCADDS) [27] | Questionnaire (completed by HCPs) |
|
| Perception of Interprofessional Collaboration Model Questionnaire (PINCOM-Q) [34] | Questionnaire (completed by HCPs) |
|
| Echelle De Confort Decisionnel-Partnenaire (ECD-P) [34] | Questionnaire (completed by HCPs) |
|
| Journey Tool [33] | Four stage process (conducted by child services evaluators) |
|
| Interprofessional collaboration competency scale [37] | Questionnaire (completed by health, medical, welfare and education professionals) |
|
| The Human Services Integration Measure Scale (HSIM) [35] | Questionnaire (completed by health, educational, social, justice, recreational, and cultural sector professionals) |
|
| Outcome: Continuity of care | ||
| Continuity of Care in Children’s Mental Health-Parent (C3MH-P) [29] | Questionnaire (completed by caregivers) |
|
| Continuity of Care in Children’s Mental Health-Youth (C3MH-Y) [29] | Questionnaire (completed by CYP) |
|
| Outcome: Completeness of care | ||
| Primary Care Assessment Tool (PCATool Brazil) [36]*† (Also measures Quality of care coordination and Structure of care) | Questionnaire (completed by HCPs) |
|
| The Paediatric Integrated Care Survey (PICS) [30]† (Also measures Quality of care coordination) | Questionnaire (completed by caregivers) |
|
| Outcome: Structure of care | ||
| Primary Care Assessment Instrument (PCAInstrument Brazil) [36]*† (Also measures Quality of care coordination and Completeness of care) | Questionnaire (completed by HCPs) |
|
| Outcome: Quality of communication | ||
| Framework for evaluating patient care communication [31]*† (Also measures Quality of care coordination) | Three stage process: 1) Questionnaire (completed by caregivers), 2) Interviews (with caregivers) and 3) Focus Groups (with HCPs) |
|
| Outcome: Local implementation of integrated care | ||
| Instrument to monitor the local implementation of Integrated Care for Childhood Overweight and obesity (TICCO) [32] | Questionnaire (completed by HCPs involved in project organisation) |
|
[i] *Study describes development of the measurement instrument only (not evaluated for feasibility, reliability or validity); †instrument measures more than one outcome.
Table 2
Summary of evaluation results of instruments (n = 13) measuring integration within children and young people healthcare systems.
| MEASUREMENT INSTRUMENT | FEASIBILITY | RELIABILITY | VALIDITY | ||
|---|---|---|---|---|---|
| CONTENT | CONSTRUCT | CRITERION | |||
| Care-coordination Measurement Tool (CCMT)[23]* | ✓ | ||||
| Bice-Boxerman Continuity of Care [24]* | ✓ | ||||
| Family Experiences with Coordination of Care (FECC) [2628] | ✓ | ✓ | |||
| Collaborative Care for Attention-Deficit Disorders Scale (CCADDS)[27] | ✓ | ✗ | |||
| Instrument to monitor the local implementation of Integrated Care for Childhood Overweight and obesity (TICCO) [32] | ✓ | ✓ | |||
| Perception of Interprofessional Collaboration Model Questionnaire (PINCOM-Q) [34] | ✓ | ✓ | |||
| Echelle de confort decisionnel-partenaire (ECD-P) [34] | ✓ | ✓ | |||
| Journey Tool [33] | ✗ | ||||
| Interprofessional collaboration competency scale [37]* | ✓ | ✓ | |||
| Continuity of Care in Children’s Mental Health-Parent (C3MH-P) [29]* | ✓ | ✓ | ✓ | ✓ | |
| Continuity of Care in Children’s Mental Health-Youth (C3MH-Y) [29]* | ✓ | ✓ | ✓ | ✓ | |
| The Human Services Integration Measure Scale (HSIM)[35]* | ✓ | ||||
| The Paediatric Integrated Care Survey (PICS) [30]* | ✓ | ✓ | |||
[i] ✓ = reasonable feasibility (quality of methods not assessed); ✓ = reasonable reliability or validity (methods very good); ✓ = reasonable reliability or validity (methods doubtful or inadequate); ✗ = inadequate validity (methods very good); ✗ = inadequate validity (methods doubtful or inadequate).
* Highlighted by authors as promising instruments based on of administration method and measurement properties, with consideration of the type of system that the instrument was designed for and evaluated in. Wider contextual factors may be considered when selecting instruments to be used in research and practice.
