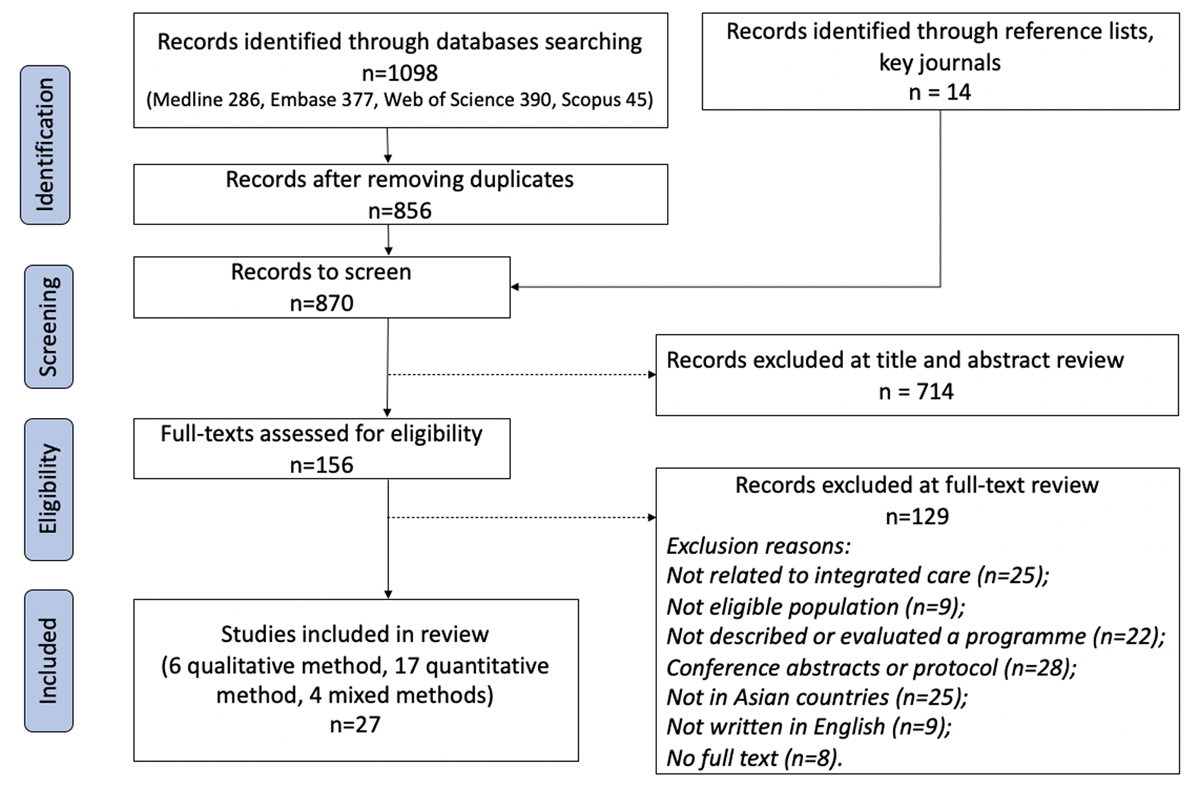
Figure 1
PRISMA flow diagram.
Table 1
Summary of characteristics of included studies and IC programmes.
| NO. OF STUDIES | REFERENCE | |
|---|---|---|
| Study design | ||
| Qualitative | 6 | |
| Descriptive study | 4 | [51706654] |
| Interviews and focus group discussions | 2 | [6364] |
| Quantitative | 17 | |
| Retrospective cohort study | 4 | [53486269] |
| Randomised controlled trial | 7 | [586157566071] |
| Quasi-experimental study | 2 | [4749] |
| Retrospective longitudinal study | 1 | [68] |
| Longitudinal and quasi-experimental study | 1 | [65] |
| Difference-in-difference design | 1 | [72] |
| Cross-sectional survey | 1 | [73] |
| Mixed methods | 4 | [67595055] |
| Reported quantitative outcome | ||
| Increase activities of daily life (ADL) | 1 | [67] |
| Increase health-related quality of life (HRQoL)/health utility | 3 | [575653] |
| Increase self-rated health | 2 | [6053] |
| Increase self-efficacy | 2 | [5760] |
| Increase patient satisfaction | 2 | [5752] |
| Reduce length of stay (LOS)a | 2 | [6158] |
| Reduce hospital admissions | 5 | [6158494862] |
| Reduce hospital readmission rate/30-day readmissionb | 5 | [5657605348] |
| Reduce outpatient attendancesc | 1 | [58] |
| Reduce emergency departments attendancesd | 3 | [534948] |
| Reduce cost | 3 | [585665] |
| Reduced Continuity of Care Index (COCI) | 1 | [72] |
| Low or moderate implementation fidelity | 1 | [50] |
| Increase cost | 1 | [47] |
| NO. OF PROGRAMMES | NAME OF PROGRAMMES | |
| Care setting(s) | ||
| Inpatient setting | 1 | Acute Medical Unit [51] |
| Community setting | 3 | Integrated Community Care System [68], Training Programmes for Primary Care Teams [73], mWellcare Programme – mHealth-based electronic decision support system [7071] |
| Home setting | 5 | home healthcare services provided with videophones [67], Health-Social Transitional Care Management Program [5657], Nurse-led Case Management Programme [60], Singapore General Hospital Transitional Home Care Programme [49], Transitional Home Care-Integrated Practice Units Programme [48] |
| Inpatient + ambulatory setting | 1 | The Reform of the Integrated County Healthcare Consortium [65] |
| Inpatient + ambulatory + community setting | 1 | Joint Health Centre pilot programme [63] |
| Inpatient + community setting | 2 | emergency physician–led frailty-care unit [62], discharge services [69] |
| Inpatient + community + home setting | 1 | Regional Health System [54] |
| Inpatient + home setting | 3 | The Aged Care Transition Program [53], National University Health System-Regional Health System Transitional Care Programme [50], National University Health System-Regional Health System Integrated Interventions and Care Extension programme [47] |
| Ambulatory + community setting | 3 | The Reform of Integrated Service Delivery Network-Luohu Hospital Group[6466], Family Doctor Plan [72], Right-Site Care program [55] |
| Ambulatory + home setting | 1 | Singapore General Hospital Transitional Care Programme [52] |
| Ambulatory + community + home setting | 1 | Targeted Case Management [5859] |
| Community + home setting | 1 | Case Management [61] |
| Target population | ||
| Elderly | 5 | Home Healthcare Services Provided with Videophones [67], Integrated Community Care System [68], Health-Social Transitional Care Management Program [5657], Hospital Discharge Services [69], Emergency Physician–led Frailty-care Unit [62] |
| Frail elderly | 2 | Case Management [61], Transitional Home Care-Integrated Practice Units Programme [48] |
| Multimorbidity | 8 | Targeted Case Management [5859], Taiwan’s Family Doctor Plan [72], Training Programmes for Primary Care Teams [73], The Aged Care Transition Program [53], Singapore General Hospital Transitional Home Care Programme [49], Nurse-led Case Management Programme [60], National University Health System-Regional Health System Transitional Care Programme [50], mWellcare Programme – mHealth-based electronic decision support system [7071] |
| Patients with a high risk of readmission | 2 | Singapore General Hospital Transitional Care Programme [52], National University Health System-Regional Health System Integrated Interventions and Care Extension programme [47] |
| Patients with chronic diseases | 3 | Joint Health Centre for chronic care [63], Right-Site Care program [55], The Reform of Integrated Service Delivery Network-Luohu Hospital Group [6466] |
| N/R | 3 | Regional Health System [54], Acute Medical Unit [51], The Reform of the Integrated County Healthcare Consortium [65] |
[i] a One article [49] reported a non-significant change in length of stay (LOS).
b Three articles [526269] reported non-significant changes in hospital readmission rate.
c One article [48] reported a non-significant change in outpatient attendances.
d One article [52] reported a non-significant change in emergency departments attendances.
Table 2
Description of integrated care programmes in the included studies.
| PROGRAMME NAME | PAPER TITLE | COUNTRY/REGION | PROGRAMME DESCRIPTION | POLITICAL BACKGROUND IN THE LOCAL CONTEXT | PROVIDER(S) INVOLVED |
|---|---|---|---|---|---|
| Home Healthcare Services Provided with Videophones (HHSPV programme, launched in 1991) | The effectiveness of videophones in home healthcare for the elderly [67]. | Japan | The programme provided medical consultation; comprehensive assessments; instructions for patients and healthcare workers; advice on the effective use of health and welfare resources; and emotional support for caregivers | The growth of the ageing population is rapid in Japan, and there are great demands on more professionals involved and coordinated services in homecare. Telecommunications between households and healthcare providers became available to meet the needs of the elderly. | physician; nurse; allied health professionals; social worker; home helpers |
| Case Management (CM programme, launched in 2000) | Cost-benefit analysis of a case management project for the community-dwelling frail elderly in Hong Kong [61]. | Hong Kong | The programme provided home visit and telephone follow-up; comprehensive geriatric assessment; care plan; coordination between health and social services; monthly monitoring via IT system; health and psychosocial counselling and health educational programmes | N/A | social worker; registered nurse (case manager); an interdisciplinary team |
| Targeted Case Management (TCM programme, launched in 2001) | Reducing utilisation of hospital services by case management: a randomised controlled trial [58]. Global case management: Hong Kong. Care for the hospital-discharged frail elders by nurse case managers: a process evaluation of a longitudinal case management service project [59]. | Hong Kong | The programme provided regular monitoring of subjects’ health status; daily phone assistance; home visits; community-based supportive services; access to medical support | Hong Kong is experiencing a growing ageing population. For post-hospital discharged elderly, access to different services is all the more daunting, given fragmented medical and social service structures and the disparate health and social care financing arrangements in Hong Kong. | nurse case managers; case geriatricians; a multidisciplinary team |
| Taiwan’s Family Doctor Plan (FDP programme, launched in 2006) | Impact of integrated healthcare: Taiwan’s Family Doctor Plan [72]. | Taiwan | The programme provided multidisciplinary teams; case management; integrated care pathways | The care delivery system in Taiwan lacks features or context of strong primary care. Taiwanese patients do not have family doctors and have access to hospital care without a referral. FDP pays office-based physicians under a national contract to provide pre-specified elements of integrated care to patients assigned to them. | physicians |
| Training Programmes for Primary Care Teams (TPPCT programme, launched in 2006) | Assessing system-based trainings for primary care teams and quality-of-life of patients with multimorbidity in Thailand: patient and provider surveys [73]. | Thailand | The programme provided integrated primary care systems management, including resource sharing; community participation and inter-sectoral collaboration; health information systems; management skills of the leaders; coordination and unity of teamwork; integrated service delivery | In Thailand, primary healthcare has long focused on national healthcare reforms and adopted a “task-shifting” strategy as a long-term approach to training health workers to work in primary care settings. Since 2006, a series of 11 training programmes for multidisciplinary primary care teams have been implemented nationwide. | physicians; a multidisciplinary team |
| The Aged Care Transition Program (ACTION programme, launched in 2008) | Effectiveness of a National Transitional Care Program in Reducing Acute Care Use [53]. | Singapore | The programme provided comprehensive assessment; medical services; social services; self-management support; care planning; follow-up through calls and home visits; coordination of referral | Singapore’s community and long-term care systems are less well developed than its acute care system. Care integration and enabling better and more-comprehensive chronic and long-term care in the nonacute sector is a priority for the Health Ministry. This gap results in a vicious cycle of discharge and readmissions to acute care hospitals. Thus, transitional care support is needed. | physicians; care coordinators; project director |
| Singapore General Hospital transitional home care programme (SGH-THC programme, launched in 2008) | Effectiveness of a transitional home care program in reducing acute hospital utilization: a quasi-experimental study [49]. | Singapore | The programme provided comprehensive medical and nursing assessment including optimising medical conditions in the home setting; education on self-management; reducing polypharmacy and medication conflicts; facilitating adherence to treatment; ensuring follow up by specialists; activating appropriate community services; care planning; telephone call reviews; early physician reviews | Singapore’s community and long-term care systems are less well developed than its acute care system. Care integration and enabling better and more-comprehensive chronic and long-term care in the nonacute sector is a priority for the Health Ministry. This gap results in a vicious cycle of discharge and readmissions to acute care hospitals. Thus, transitional care support is needed. | family physician; nurse case manager; physiotherapist; occupational therapist; speech therapist; medical social worker |
| Integrated Community Care System (ICCS programme, launched in 2009) | “Ageing in Place” Policy in Japan: Association Between the Development of an Integrated Community Care System and the Number of Nursing Home Placements Under the Public Long-Term Care Insurance Program Among Municipal Governments [68]. | Japan | The programme provided prevention of long-term care; support for case managers; case conference; discharge planning; home healthcare; end of life care at home; housing provision; improved home environment; prevention of social isolation; suicide prevention; disaster risk management; advocacy for elderly; elder abuse prevention and intervention | In 2000, a national long-term care insurance (LTCI) programme for the elderly was introduced to differentiate social care from healthcare and to help people age in place. In 2006, community-based care services and community general support centres in municipalities were introduced into the LTCI programme to establish one-stop home care services. The national government published a model of the “Integrated Community Care” system model. | care manager; home care service provider; community-based service provider; residential care service provider; housing service provider |
| Nurse-led Case Management Programme (NCM programme, launched in 2010) | A randomized controlled trial of a nurse-led case management programme for hospital-discharged older adults with co-morbidities [60]. | Hong Kong | The programme provided comprehensive pre-discharge needs assessment; development of goal and care plan with patients; analysis of performance barriers with patients; monitoring of system; home visit for post-discharge assessment; training of nursing students; support in maintaining self-management behaviours | N/A | nurse case managers; nursing students |
| Health-Social Transitional Care Management Program (HSTCM programme) | Effects of a health-social partnership transitional program on hospital readmission: A randomized controlled trial [57]. Cost-effectiveness of a health-social partnership transitional program for post-discharge medical patients [56]. | Hong Kong | The programme provided home visits; assessment in the holistic domains; relevant intervention; social support; follow-up telephone calls; social assessment and interventions; regular case reviews | N/A | nurse case manager; trained volunteers; social workers |
| Singapore General Hospital Transitional Care Programme (SGH-TC programme launched in 2011) | Transitional care for the highest risk patients: findings of a randomised control study [52]. | Singapore | The programme provided comprehensive assessment; post-discharge surveillance of the patient to ensure adherence to care plans; coordination of follow-up visits with specialist care providers; patient education and caregiver coaching; activation of community and social services | Singapore’s community and long-term care systems are less well developed than its acute care system. Care integration and enabling better and more-comprehensive chronic and long-term care in the nonacute sector is a priority for the Health Ministry. This gap results in a vicious cycle of discharge and readmissions to acute care hospitals. Thus, transitional care support is needed. | doctor; advance practice nurse; nurses; medical social worker; physical therapists; pharmacists |
| Regional Health System (RHS programme, launched in 2012) | Implementation of Integrated Care in Singapore: A Complex Adaptive System Perspective [50]. | Singapore | The programme provided a network led by a major public hospital, close partnership with other healthcare providers; social care providers within the same geographical region | As the demands for healthcare services increase with ageing, Singapore realised that a disease-centred provision of services within the hospitals is insufficient and unsustainable in the long term. The RHS model was introduced by the Ministry of Health in 2012 to foster integrated care within respective geographic regions. | major public hospital; primary care providers; community hospitals; nursing homes; home care; day rehabilitation providers; social care providers |
| National University Health System-Regional Health System Transitional Care Programme (NUHS-RHS TC programme, launched in 2012) | Implementation fidelity of a strategy to integrate service delivery: learnings from a transitional care program for individuals with complex needs in Singapore [47]. Retrospective evaluation of healthcare utilisation and mortality of two post-discharge care programmes in Singapore [54]. | Singapore | The programme provided needs assessments; development of personalised care plans; care coordination; case closure | The RHS in Singapore was designed to integrate hospitals with primary and community care partners within a geographical region. The National University Health System (NUHS) RHS is one of the RHS systems in Singapore and launched two programmes to improve post-discharge care and anchor care in the community and reduce healthcare utilisation in 2014: (1) NUHS-RHS Integrated Interventions and Care Extension (NICE) programme and (2) NUHS Transitional Care Programme (NUHS TCP). | care coordinators; multidisciplinary care team; medical care providers; social care workers |
| Joint Health Centre for chronic care (JHC programme, launched in 2013) | Integrated care reform in urban China: a qualitative study on design, supporting environment and implementation [63]. | China | The programme provided integrated care of primary health care and specialist; care in coordinated hospitals; referral to different levels of care facilities; follow-up by GPs | China initiated some pilot integrated care models between hospitals and community health centres (CHCs) in Henan Province, Qinghai Province, to develop a vertical referral system among health providers. As one of the pilots, the Hangzhou municipal government implemented some innovations. The integrated care model was created, namely the Joint Health Centre (JHC) for chronic care. | general practitioners; nurses; specialists (hospitals) |
| Hospital Discharge Services (HDS programme, launched in 2013) | Associations of Hospital Discharge Services with Potentially Avoidable Readmissions Within 30 Days Among Older Adults After Rehabilitation in Acute Care Hospitals in Tokyo, Japan [69]. | Japan | The programme provided discharge planning; rehabilitation discharge instruction on self-management and community care at discharge; coordination with long-term care | Japanese hospitals do not offer comprehensive transitional care programmes under the health insurance system. Some individual services such as discharge planning were covered by insurance and used a diagnosis procedure combination (DPC) system to enable case-mix adjustments for reimbursements. | nurses; medical social workers; doctors; allied health professionals; care manager |
| National University Health System-Regional Health System Integrated Interventions and Care Extension (NUHS-RHS NICE programme, launched in 2014) | Retrospective evaluation of healthcare utilisation and mortality of two post-discharge care programmes in Singapore [47]. | Singapore | The programme provided case management for patients and caregivers; follow-up home visits and telephone calls; community-based care management | The RHS in Singapore was designed to integrate hospitals with primary and community care partners within a geographical region. The National University Health System (NUHS) RHS is one of the RHS systems in Singapore and launched two programmes to improve post-discharge care and anchor care in the community and reduce healthcare utilisation in 2014: (1) NUHS-RHS Integrated Interventions and Care Extension (NICE) programme and (2) NUHS Transitional Care Programme (NUHS TCP). | case managers; social workers; volunteers |
| Right-Site Care (RSC program, launched in 2014) | Shifting care from hospital to community, a strategy to integrate care in Singapore: process evaluation of implementation fidelity [55]. | Singapore | The programme provided referral of suitable patients by specialists; coordination of care under one dedicated physician; stratification of care and care location; preparation of transition; support for primary and community care providers; multidisciplinary case conference to refine care plans | In 2013, within the NUHS RHS in Singapore, over 600,000 unique attendances at the SOCs in its primary acute hospital, rising from 500,000 in 2009. In response to this rapid increase in SOC utilisation, NUHS RHS imitated the Right-Site Care (RSC) programme to facilitate timely discharge and support the appropriate transition from the hospital to the community. | care coordinators; family physicians; a team of healthcare workers |
| Acute Medical Unit (AMU programme, launched in 2015) | Acute medical unit: experience from a tertiary healthcare institution in Singapore [51]. | Singapore | The programme provided early internist-led assessment and management; holistic management; active re-triaging of the patient; inpatient treatment triggered; allied health services; clinical management and services support | The care stratum of dealing with admitted patients with multiple diseases and complex conditions is not well established in the Singapore healthcare model. National University Hospital in Singapore collaborated with the emergency department to create an acute medical team and scaled it up to an acute medical unit. | internists; nurses; allied health professionals |
| Transitional Home Care-Integrated Practice Units Programme (THC-IPU programme, launched in 2015) | Transitional Home Care Program Utilizing the Integrated Practice Unit Concept (THC-IPU): Effectiveness in Improving Acute Hospital Utilization [48]. | Singapore | The programme provided comprehensive medical and nursing assessment; reconciliation; caregiver education; personal health record; multidisciplinary team meetings; telephone follow up; allied health services; home visits; readmissions review | In Singapore, nearly a quarter of semi-ambulant and non-ambulant Singapore elderly stay alone or with their elderly spouse. At the same time, primary care and home care in Singapore are relatively less developed than tertiary care. In 2016, the Ministry of Health decided to transit it to a new transitional care model named “Hospital to Home”. | junior physicians; home care nurses; allied health professionals; pharmacist; medical social worker; administrators; senior family physicians |
| The Reform of Integrated Service Delivery Network-Luohu Hospital Group (Luohu Group programme, launched in 2015) | The Luohu Model: A Template for Integrated Urban Healthcare Systems in China [66]. Building a People-Centred Integrated Care Model in Urban China: A Qualitative Study of the Health Reform in Luohu [64]. | China | The programme provided integrated health care with public health services and social services; merged resources of hospitals and community health centres; training providers; consolidated professional resources; a formal two-way referral system, timely decision support; shared information system; guide by a “health-centred” perspective; a shared goal | In 2016, the Chinese government proposed strengthening healthcare in China through a tiered health care delivery system following a People-Centred Integrated Care model. A guideline for constructing Medical Consortia suggested hospital groups in urban areas, medical associations in rural areas, cross-regional specialist alliances, and telecollaboration networks. In 2017, China’s National Health and Family Planning Commission introduced the Luohu model to achieve “less illness, fewer hospital admissions, lower financial burdens, and better services”. | the district government; the municipal government; hospitals; health workers in community health centres; family doctor team |
| The Reform of the Integrated County Healthcare Consortium (ICHC programme, launched in 2015) | Does capitation prepayment based Integrated County Healthcare Consortium affect inpatient distribution and benefits in Anhui Province, China? An interrupted time series analysis [65]. | China | The programme integrated high-quality healthcare resources in the county to provide integrated and continuous healthcare for residents and established capitation prepayment of the New Rural Cooperative Medical System (NRCMS) funds. | In 2002, the Chinese government established the New Rural Cooperative Medical System (NRCMS) to provide rural residents with outpatient and inpatient reimbursement for some compliance costs. As rural residents in China can freely choose hospitals, and three-tiered healthcare hospitals have yet to achieve a good cooperation relationship, patients tend to go to high-level hospitals for improved treatment, which increases healthcare expense and places tremendous pressure on the NCRMS funds. In 2015, Anhui Province launched the reform of the Integrated County Healthcare Consortium (ICHC) with capitation prepayment of the NRCMS funds following the principle of “exceeds expenditures does not make up, the balance holds for use”. | county-level hospitals (CHs); township-level hospitals (THs); village clinics |
| Emergency Physician–led Frailty-care Unit (EPFU programme, launched in 2015) | The effectiveness of an emergency physician-led frailty unit for the living-alone elderly: A pilot retrospective cohort study [62]. | Hong Kong | The programme provided a mandatory and complete input of electronic Patient Assessment Form; a comprehensive enquiry of social background; a mandatory bundled referral to the pre-discharge team; daily ward; management plan; a target of discharge within 72 h of admission | The Accident & Emergency Department of Queen Elizabeth Hospital in Hong Kong catered for 184,433 new case attendances in 2016/2017. To respond to this growing demand, a six-bed frailty-care unit dedicated to the community-dwelling elderly was established in 2015 within the Emergency Medicine Ward based on the British National Health Service (NHS) frailty model. It is the first of its kind in Hong Kong. | physicians; geriatricians; nurses; allied health professionals; social workers |
| mWellcare Programme – mHealth-based electronic decision support system (mWellcare programme, launched in 2016) | Development of mWellcare: an mHealth intervention for integrated management of hypertension and diabetes in low-resource settings [70]. Effectiveness of an mHealth-Based Electronic Decision Support System for Integrated Management of Chronic Conditions in Primary Care: The mWellcare Cluster-Randomized Controlled Trial [71]. | India | The programme provided a generation of EDS recommendations for the management of diseases; store electronic health records; long-term monitoring and follow-up; reminder message service for scheduled medication adherence and follow-up visits; training | The burden of non-communicable diseases (NCDs), population ageing, severe shortage of skilled healthcare providers, and inadequately developed health systems impose huge constraints on healthcare services in India. The 1979 Alma Ata declaration endorsed strengthening primary care to improve health outcomes. Innovations using mobile phone technologies and task sharing by trained nurses can empower and facilitate the care process. | Community Health Centre physicians; NCD nurses |
Table 3
Dimension and components of integrated care programmes.
| PROGRAMME NAME | TARGET POPULATION CARE SETTING | COUNTRY/REGION | DIMENSION OF INTEGRATED CARE | INTEGRATED CARE COMPONENTSA | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MACRO-LEVEL | MESO LEVEL | MICRO-LEVEL | HORIZONTAL IC | VERTICAL IC | MM | ENVIRONMENT | SERVICE DELIVERY | LEADERSHIP | WORKFORCE | FINANCING | TECHNOLOGY | INFORMATION | MONITORING | ||||
| HHSPV programme | elderly home setting | Japan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| CM programme | frail elderly home setting community setting | Hong Kong | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| TCM programme | multimorbidity ambulatory setting community setting home setting (mainly) | Hong Kong | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| FDP programme | multimorbidity ambulatory setting community setting | Taiwan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| TPPCT programme | multimorbidity community setting | Thailand | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| ACTION programme | multimorbidity inpatient setting home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| SGH-THC programme | multimorbidity home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| ICCS programme | elderly community setting | Japan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| NCM programme | multimorbidity home setting | Hong Kong | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| HSTCM programme | elderly home setting | Hong Kong | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| SGH-TC programme | patients with high risk of readmission ambulatory setting home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| NUHS-RHS TC programme | multimorbidity inpatient setting home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| RHS programme | N/R inpatient setting community setting home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| HC programme | patients with chronic diseases ambulatory setting inpatient setting community setting | China | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| HDS programme | elderly inpatient setting community setting | Japan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| NUHS-RHS NICE programme | patients with high risk of readmission inpatient setting home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| RSC program | patients with chronic diseases ambulatory setting community setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| AMU programme | N/R inpatient setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| THC-IPU programme | frail elderly home setting | Singapore | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Luohu Group programme | patients with chronic diseases ambulatory setting community setting | China | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| ICHC programme | N/R ambulatory setting inpatient setting | China | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| EPFU programme | elderly inpatient setting community setting | Hong Kong | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| mWellcare programme | multimorbidity community setting | India | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| No. of programmes per dimension/component | 6 | 7 | 20 | 23 | 14 | 11 | 14 | 23 | 23 | 23 | 9 | 12 | 11 | 15 | |||
[i] Abbreviations: MM = multimorbidity, N/R = Not reported, HHSPV = Home Healthcare Services Provided with Videophones, CM = Case Management, TCM = Targeted Case Management, FDP = Family Doctor Plan, TPPCT = Training Programmes for Primary Care Teams, ACTION = The Aged Care Transition, SGH-THC = Singapore General Hospital transitional home care, ICCS = Integrated Community Care System, NCM = Nurse-led Case Management Programme, HSTCM = Health-Social Transitional Care Management, SGH-TC = Singapore General Hospital Transitional Care, NUHS-RHS TC = National University Health System-Regional Health System Transitional Care, RHS = Regional Health System, JHC = Joint Health Centre, HDS = Hospital Discharge Services, NUHS-RHS NICE = National University Health System-Regional Health System Integrated Interventions and Care Extension, RSC = Right-Site Care, AMU = Acute Medical Unit, THC-IPU = Transitional Home Care-Integrated Practice Units, ICHC = Integrated County Healthcare Consortium, EPFU = Emergency Physician–led Frailty-care Unit.
a According to the SELFIE Conceptual Framework, integrated care for multimorbidity population includes nine components: (1) multimorbidity, (2) environment, (3) service delivery, (4) leadership and governance, (5) workforce, (6) financing, (7) technology and medical products, (8) information and research, (9) monitoring. Programmes were marked if the concerned component was mentioned or reported in the included studies regardless of emphasising any level (micro/meso/macro).
