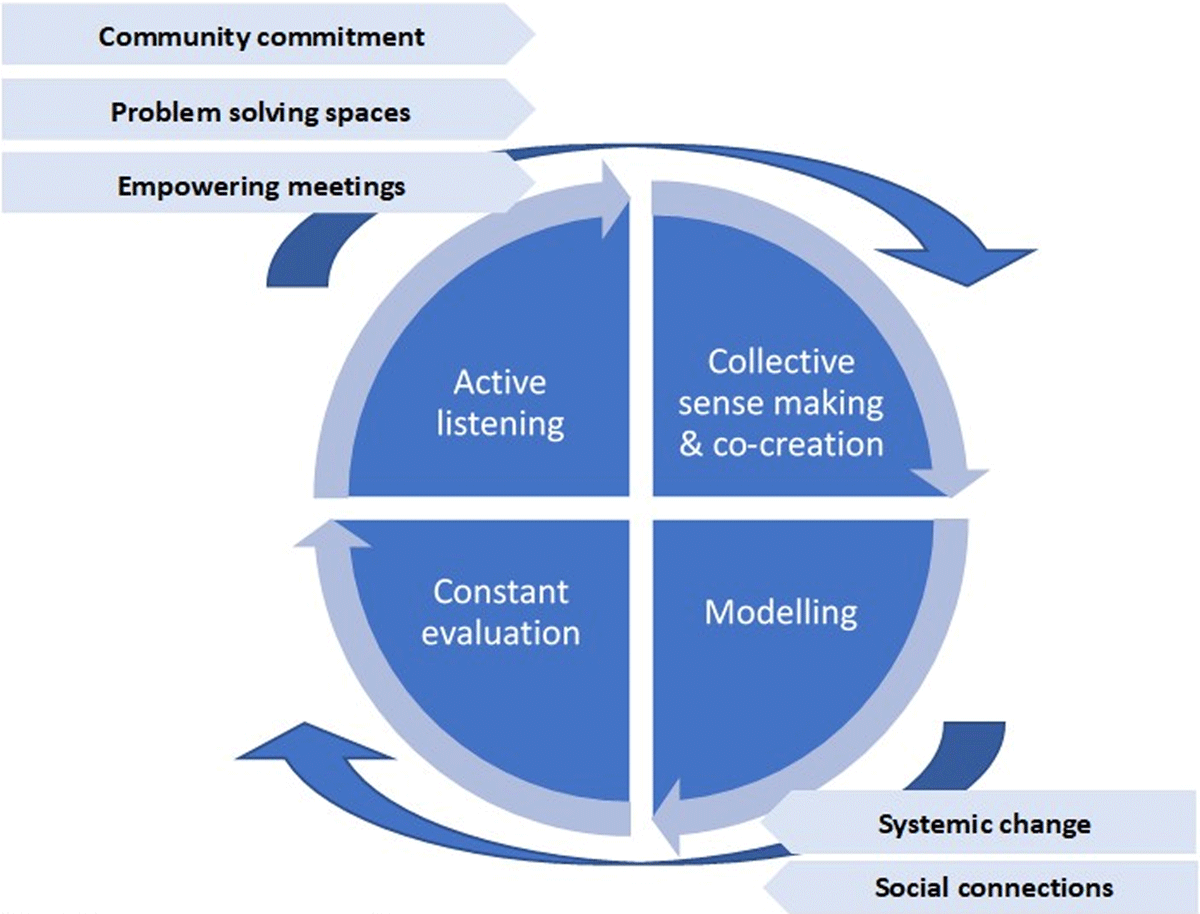
Figure 1
Social innovation process.
Source: Elaborated by authors.
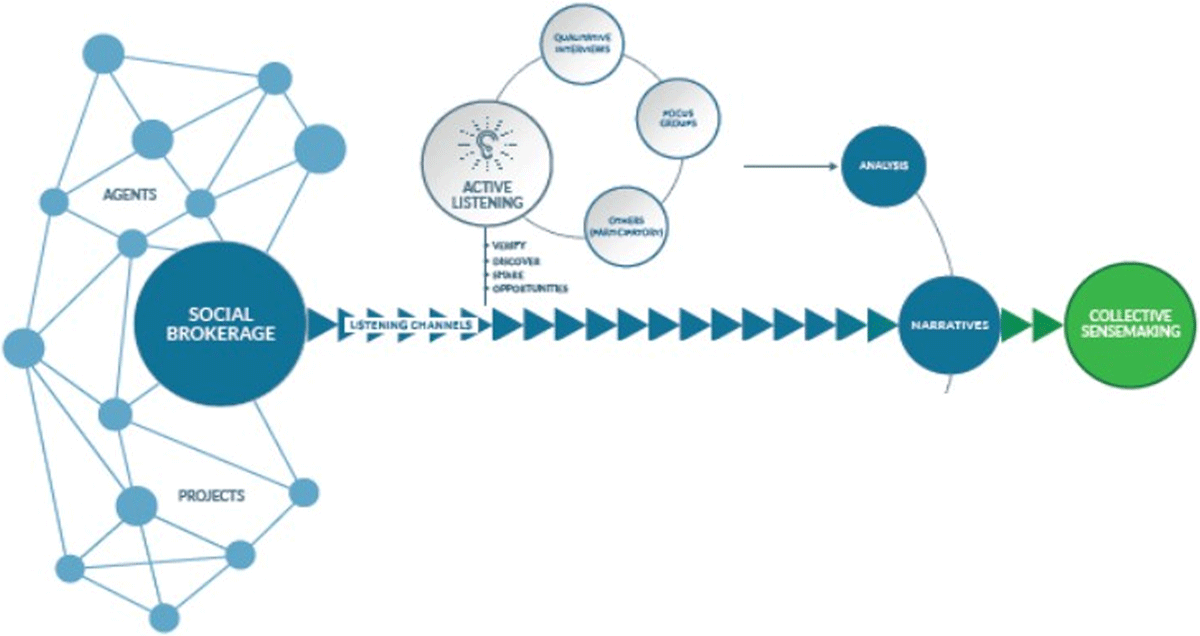
Figure 2
Iterative listening and co-creation phases for collective sense making.
Source: Adapted from Agirre Lehendakaria Center for social and political studies.
Table 1
Synthesis of main ideas from interviews: challenges and opportunities.
| PROFILE/ROLE | MAIN IDEAS AND RELATED QUOTATIONS |
|---|---|
| Government and social services managers | Lack of services for the demand with an increase of care needs for these people and families “The social services cannot cope with all the demands that need to be met. It is important that we recognize our weakness something that we find very difficult”. “The management of the social services is very complicated. It is not integrated and is not flexible”. “We are not taking into account the demographic changes, it is becoming increasingly difficult for us to identify the people”. |
| Health services professionals | Basque Health Services does not reach and cannot attend all needs of everyone in end-of-life situations “(…) The system helps me with chemo and surgery, but not with the other part – that is what I miss”. “There is an area of mental health care, but it is not enough for what we need”. Challenges for attending situations of end-of-life and dependency with home-care services “They are trying to tell us that looking after people at home is cheaper but that is not true. The reality is that it is way more expensive”. Health services professionals lack specific training to care and support people in end-of-life situations “There is no training for health care professionals to better care for people and their families in end of life”. “The medical reports do not represent the people’s reality at all, the person is dying and we know nothing about their social situation, we only know if they are getting worse o if they die without giving any detail to what happened, the process…”. Palliative care, end-of-life situations, and bereavement are not a priority for managers and governments “I would love to take some time out to be able to train better”. “Anything to do with education and free time seem to be the priority, however anything that has to do with bereavement, death, suffering is not a priority …”. Change should start from fiscal policy changes “Everyone knows that in order to change the system we must build a more balanced tax system”. “We have to start looking at out healthcare system in a different way. We need to see it as part of a system”. Social and health services quality varies according to the professional that looks after you “We need someone who can detect vulnerability. A professional who is trained and is flexible and has an integrated vision of how it should be. “ Economic inequalities have an impact on the quality of care you benefit from, public services do not cover all needs “With money everything is possible. I can get a lawyer to fight to show my level of dependency”. “(…) If you don’t have money, it is all too expensive, it can cause you to be completely broke”. Health and social services interaction are not dynamic “I have colleagues who will tell you that social needs are not their responsibility”. “The health sector and the social sector are completely separate, this is a complete disaster”. |
| Educational professionals | Teachers are not prepared for dealing with end-of-life situations or bereavement in schools “At the moment there is a level of sensitivity but it is not enough, we need more training”. “We are educating our children in a society that we only want to be happy; they have to be happy….but, life is not only that”. Professionals lack from tools and abilities to face these situations “People die often and yet we are not ready, we have to call a specialist when it happens, we don’t know what to do”. Not dealing correctly with end-of life situations may advocate children to academic failure at school “If you cannot deal with loss in life it is very difficult to move forward”. “(…)I was a failure at school because I had not been able to work through the loss of my mother”. |
| Culture and other community members | Support from social services is usually functional and supportive in their treatment “When you talk to someone by phone and just listen to them for half an hour you can see how their anxiety lowers. They feel less alone. But this happens once a month at the most. What do they do the rest of the time?”. People do not know what services exist and are available “People do not know who does what and where to call”. Administration and formal care services structures do not facilitate the promotion of compassionate communities “I have felt really bad. But I am not as badly off as others because in the end I am ok. I have a bit of get up and go still left in me, I still want to live life. But I have felt a bit left out people don’t know what to do with me, what to say….”. “Sometimes people call us because they feel we are closer to them and then the social services get annoyed and don’t understand why people don’t call them. But in the end of the day people see the social services as an agency to look for services both financially and logistics not so much for emotional needs”. Effective care and support need to be adequately resourced “To put into place community initiatives we need resources otherwise we have created an amazing network but there are no resources to do things”. Social care structures do not take advantage of the people in the community “The system of social protection treats the elderly like children. They are many retired people with free time, health and the desire to contribute and do things”. People tend to feel loss after dedicating years to care from their family members “There is a group of women who are 60+ and have spent all their lives caring for others, their families, their parents, and their children. When their children grow up they are at a loss they don’t know what to do with themselves and they become very isolated”. People in these situations used to be stigmatized “People are afraid to ask for help”. “We live in a society that gives when it feels it will get something back”. Human capital remains in associations, which compete sometimes amongst themselves “(…) in the associations and community, grassroots movements, there is competition between themselves. When a new movement is created the sensation is that here comes another that has to get part of the Kitty”. “Some associations have more privileges than others and no one seems to know why”. |
[i] Source: Prepared by authors.
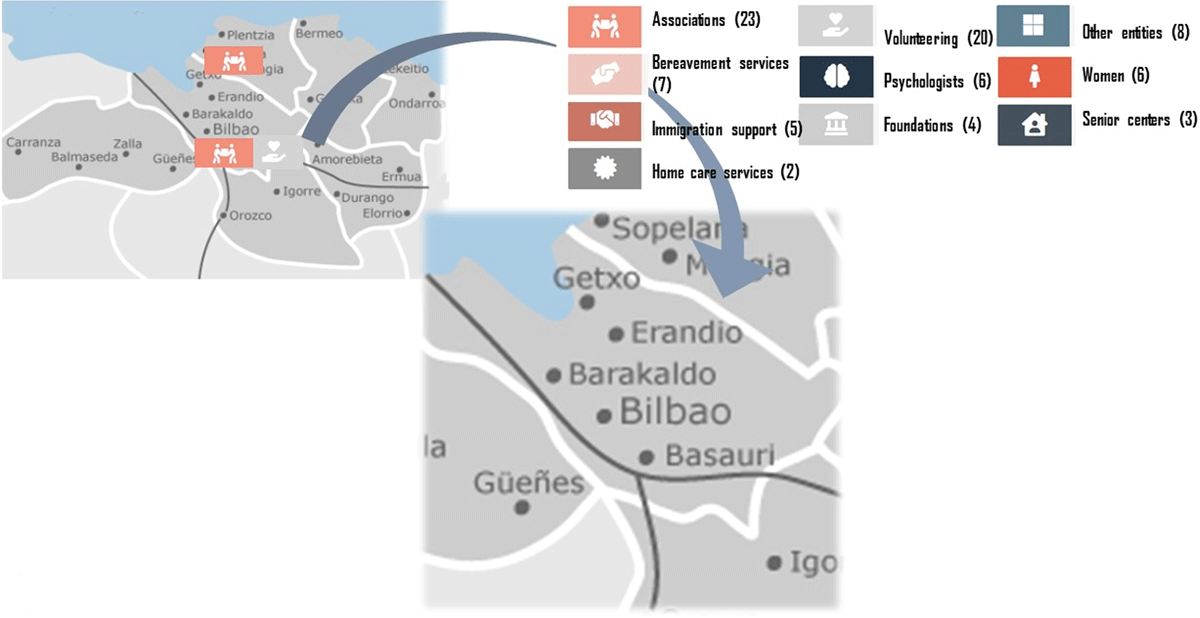
Figure 3
Community and institutional agents chart in Getxo Zurekin.
Source: Elaborated by authors from the compassionate chart at fundacionsonrisa.com/.
Table 2
Breakdown of profiles included in in-depth interviews.
Source: Elaborated by authors.
| N (% OF TOTAL) | |
|---|---|
| Sex | |
| Woman | 47 |
| Man | 23 |
| Age (variability) | 16-90 years old |
| Profession/role | |
| Primary care, palliative, HaH physician | 7 (9.85) |
| Nurse | 4 (5.63) |
| Psychologist | 2 (2.81) |
| Social worker | 1 (1.40) |
| Teaching professional | 4 (5.63) |
| Immigrant career | 6 (8.45) |
| Local business person | 10 (14.08) |
| Sick people | 4 (5.63) |
| Public administration representative | 2 (2.81) |
| Volunteer | 18 (25.35) |
| Informal career | 6 (8.45) |
| Funeral service/cemetery professionals | 3 (4.22) |
| Religious | 1 (1.40) |
| Student | 1 (1.40) |
| Journalist (with loss history) | 2 (2.81) |
| HaH: Hospitalization at Home | |
Table 3
Listening activities and outreach. 2017–2021.
| YEAR | TYPE OF ACTIVITY | NUMBER OF ACTIVITIES DONE | NUMBER OF PEOPLE REACHED |
|---|---|---|---|
| 2017 | Talks/Workshops | 3 | 145 |
| Death Cafés | 2 | 30 | |
| Training courses | 1 | 20 | |
| Conferences | 2 | 1,100 | |
| 2018 | Talks/Workshops | 23 | 847 |
| Death Cafés | 12 | 199 | |
| Training courses | 6 | 230 | |
| Conferences | 6 | 2.680 | |
| 2019 | Talks/Workshops | 6 | 250 |
| Death Cafés | 10 | 94 | |
| Training courses | 11 | 207 | |
| Conferences | 2 | 1,240 | |
| 2020 | Talks/Workshops | 8 | 200 |
| Death Cafés | 5 | 64 | |
| Training courses | 4 | 40 | |
| Virtual seminars | 2 | 120 | |
| Individual telephone support (COVID derived) | 18 families with care responsibilities, in charge of dependant members or oncology processes. |
[i] Source: Prepared by authors.
