Table 1
Description of the implementation planning process.
* For the purpose of the study, the term analysis of actual practices has been used instead of analysis of actual performance (per Grol & Wensing’s model) to better reflect our qualitative perspective.
PCN = primary care nurse, GP = general practitioner, FMG = family medicine group, CCM = collaborative care model.
| STEPS | GOAL | SUMMARY OF MAIN ACTIVITIES | PERIOD |
|---|---|---|---|
| 1) Proposal for change |
|
| Jan. 2017–Jan. 2019 |
| 2) Analysis of actual practices* |
|
| Dec. 2018–Apr. 2019 |
| 3) Problem analysis |
|
| Jan. 2019–May 2019 |
| 4) Selection of strategies and development of a plan |
|
| June 2019–Jan. 2020 |
Table 2
Main characteristics of FMGs.
| FMG01 | FMG02 | FMG03 | |
|---|---|---|---|
| Years since its creation | 15 | 16 | 12 |
| Number of sites | 1 | 1 | 2 |
| Number of patients registered (~) | 30,000–35,000 | 30,000–35,000 | 10,000–15,000 |
| TYPE AND NUMBER OF PROFESSIONALS | |||
| General practitioners | 25–30 | 30–35 | 10–15 |
| Primary care nurses | 6 | 5 | 3 |
| Nurse practitioners | 3 | 0 | 2 |
| Social workers | 3 | 3 | 1 |
| Psychologist | 1 | 1 | 1* |
| Pharmacists | 2 | 1 | 1 |
[i] * The psychologist in FMG03 had a teaching mandate rather than providing direct care to patients.
Table 3
Participants’ profile.
| LOCAL WORKING GROUP MEMBERS | |||
|---|---|---|---|
| TYPE OF PARTICIPANTS | FMG01 | FMG02 | FMG03 |
| Clinicians | N = 4 | N = 3 | N = 7 |
| 1 PCN with expertise in mental health 1 GP with expertise in mental health (lead GP) 1 nurse practitioner 1 nurse manager from the regional health center | 1 PCN (leader) 1 GP with expertise in mental health (lead GP) 1 nurse manager from the regional health center (same as FMG01) | 2 PCNs 1 quality improvement agent 2 GPs (including the lead GP) 1 social worker 1 psychologist | |
| INTERVIEW AND/OR OBSERVATION PARTICIPANTS | |||
| Clinicians | N = 9 | N = 8 | N = 7 |
| 5 PCNs 1 GP 1 social worker 1 nurse practitioner 1 pharmacist | 5 PCNs 1 GP 1 social worker 1 psychologist | 3 PCNs 2 GPs 1 social worker 1 nurse practitioner 1 psychologist | |
| Patients* | N = 3 | N = 3 | N = 2 |
| Had two or more long-term physical conditions (e.g., hypertension, diabetes, cholesterol). Two reported both substance use disorder and depression, one an anxiety disorder. | Had at least two long-term physical conditions. Two reported both anxiety and depressive disorders, one an anxiety disorder. | Had at least two long-term physical conditions. Both reported comorbid substance use, depressive, and anxiety disorders. | |
Table 4
Contextual factors taken into account when formulating strategies.
| FMG01 | FMG02 | FMG03 |
|---|---|---|
| OUTER SETTING | ||
| External mental health service offers and patient needs* | ||
| Patients’ expectation of close monitoring of their condition by a competent professional whom they trust and can refer to when dealing with mental health problems General difficulty accessing non-pharmacological treatments and services for CMDs | ||
| INNER SETTING | ||
| Gapsbetween current practices and care manager activities | ||
| Varying degree of PCN involvement in the continuum of care and services for people with CMDs Lack of collaboration between GPs, NPs, and PCNs for the management of CMDs Lack of a clear definition of the role of PCNs for people with CMDs | Limitation of PCNs to short-term involvement in the management of CMDs, or to medication and health status monitoring when providing follow-up No tangible description regarding the clinic’s actual procedure/care trajectories and the role of PCNs for people with CMDs and long-term physical conditions | Lack of collaboration between PCNs and GPs in the management of CMDs General lack of collaboration between PCNs, GPs, and SWs Lack of a clear definition of the role of PCNs in general PCNs were not involved in the detection of anxiety and depressive symptoms in people with long-term physical conditions |
| Access to knowledge and information | ||
| Uncertainty whether PCNs were comfortable enough and had sufficient knowledge to provide care manager activities for people with CMDs to implement changes in their practices | Uncertainty among working group members about how PCNs can be involved in psychosocial interventions | Uncertainty among PCNs about the feasibly of integrating care manager activities into their current workload (had to follow several chronic disease monitoring protocols for various clienteles) Lack of awareness among GPs and PCNs about an existing internal care protocol for depression, which the medical team had not approved Lack of training among PCNs to implement the existing depression care protocol |
| Available resources | ||
| Not reported | Low nurses-to-physicians ratio (5 to 25) limiting PCNs’ ability to collectively care for the population of patients with anxiety and/or depressive disorders | Unstable roster of PCNs (maternity leaves, the arrival of new nurses) |
| Compatibility | ||
| Not reported | Uncertainty with the respective role and responsibilities of PCNs and SWs regarding psychosocial interventions and follow-up | Not reported |
| Relative priority | ||
| Not reported | Uncertainty whether adopting care manager activities was a priority for PCNs not on the working group | Uncerainty whether providing care manager activities to patients with CMDs was a perceived need for the entire medical team and nurses |
[i] CCM = collaborative care model, PCN = primary care nurse, GP = general practitioner, FMG = family medicine group, SW = social worker, CMD = common mental disorder.
* Emerged from patients interviews in the three FMGs and from patient partners in the advisory committee, shared by the first authors during local working groups meetings.
Table 5
Formulation of strategies to improve the adoption of care manager activities by PCNs.
| FMG01 | FMG02 | FMG03 | |
|---|---|---|---|
| Train and educate stakeholders | Conduct educational meetings to train PCNs on care manager activities for people with CMDs Shadow other experts to offer clinical support to PCNs (potentially including coaching and case discussions with NPs) Make training dynamic by involving NPs Screen current training programs and develop or adapt educational materials with the regional health center (P) | Conduct educational meetings to inform PCNs on existing self-management support tools and on low-intensity psychosocial interventions that they can provide as part of a follow-up Develop educational materials in collaboration with the research team to facilitate the training of newly hired nurses in the clinic’s care trajectories and the role of PCNs for people with CMDs and long-term physical conditions (P) | Conduct educational meetings to train PCNs in screening anxiety and depressive symptoms (P) |
| Support clinicians | Revise PCNs’ professional role and responsibilities regarding care for CMDs Develop resources sharing agreements between the FMG and regional health center to ensure that PCNs have time available for training (P) | Revise PCNs’ professional role and responsibilities regarding the follow-up of people with anxiety or depressive disorders and clarifying the complementarity of the SW and PCN roles | Revise PCNs’ professional role in the follow-up of people with CMDs and long-term physical conditions (P) Remind PCNs managing long-term physical conditions of their role in screening for anxiety and depressive symptoms by adding a section on this topic in clinical protocols (P) |
| Develop stakeholder interrelationships | Obtain formal commitment from all PCNs to ensure readiness to change their practices (P) Capture local knowledge from FMG02 by consulting PCNs’ about their current practice for people with mental health problems (P) | Obtain formal commitment from all PCNs to ensure readiness to change their practices and consult them on strategies to prioritize for implementation (P) | Conduct local consensus discussion to evaluate the feasibility of optimizing the role of PCNs in providing care manager activities for people with CMDs and long-term physical conditions and to improve collaboration between PCNs, GPs, and SW during clinical follow-up Use a workgroup to clarify the role of PCNs and the local care trajectory for people with CMDs (P) |
| Use evaluative and iterative strategies | Conduct small trials cyclically with some GPs to test the implementation of change (P) |
[i] CMD = common mental disorder, GP = general practioner, PCN = primary care nurses, NP = nurse practitioner, SW = social worker.
(P) indicates strategies that were prioritized for implementation.
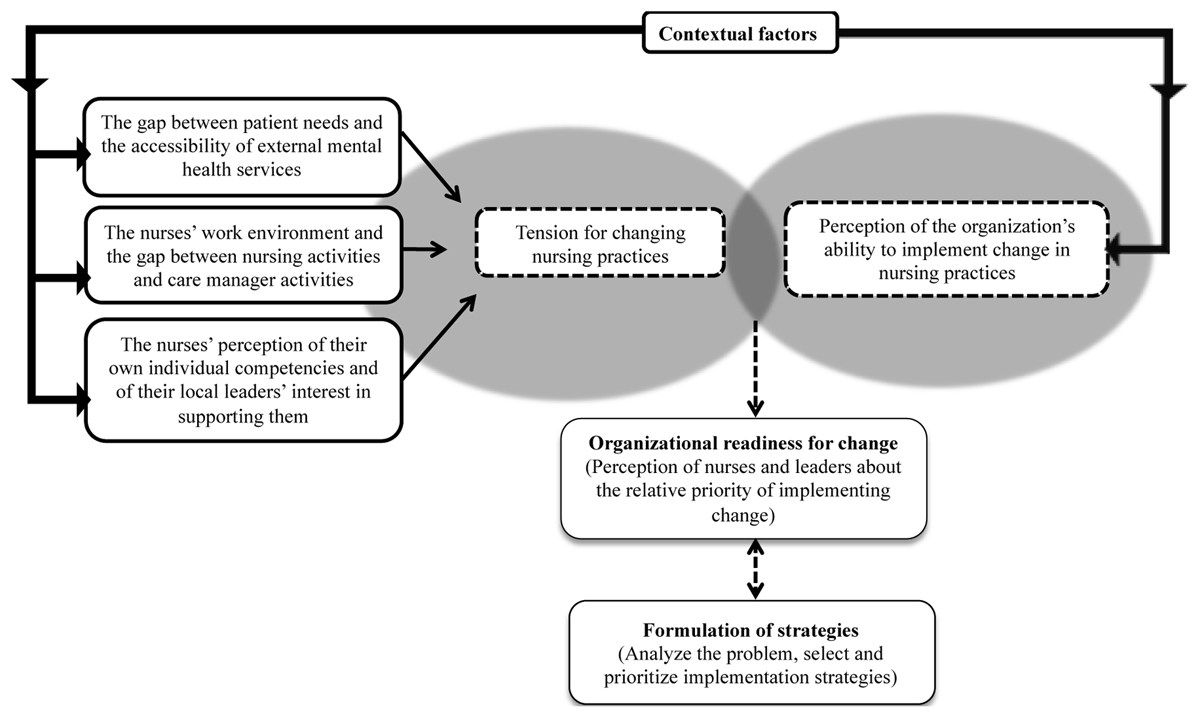
Figure 1
Influence of contextual factors on the formulation of implementation strategies to improve the adoption of care manager activities by primary care nurses.
