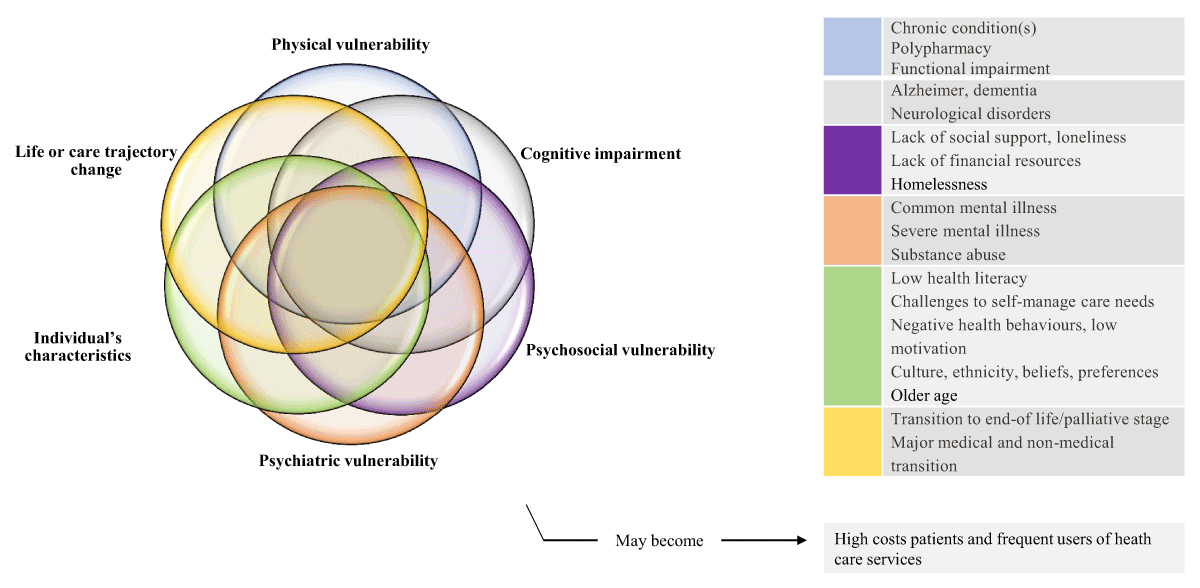
Figure 1
Complex health and social care needs.
Source: Authors’ own elaboration. Key articles that guided this illustration include Garcia ME et al. 2018 [40]; Grembowski D, et al. 2014 [42]; Kuluski K, et al. 2017 [14].
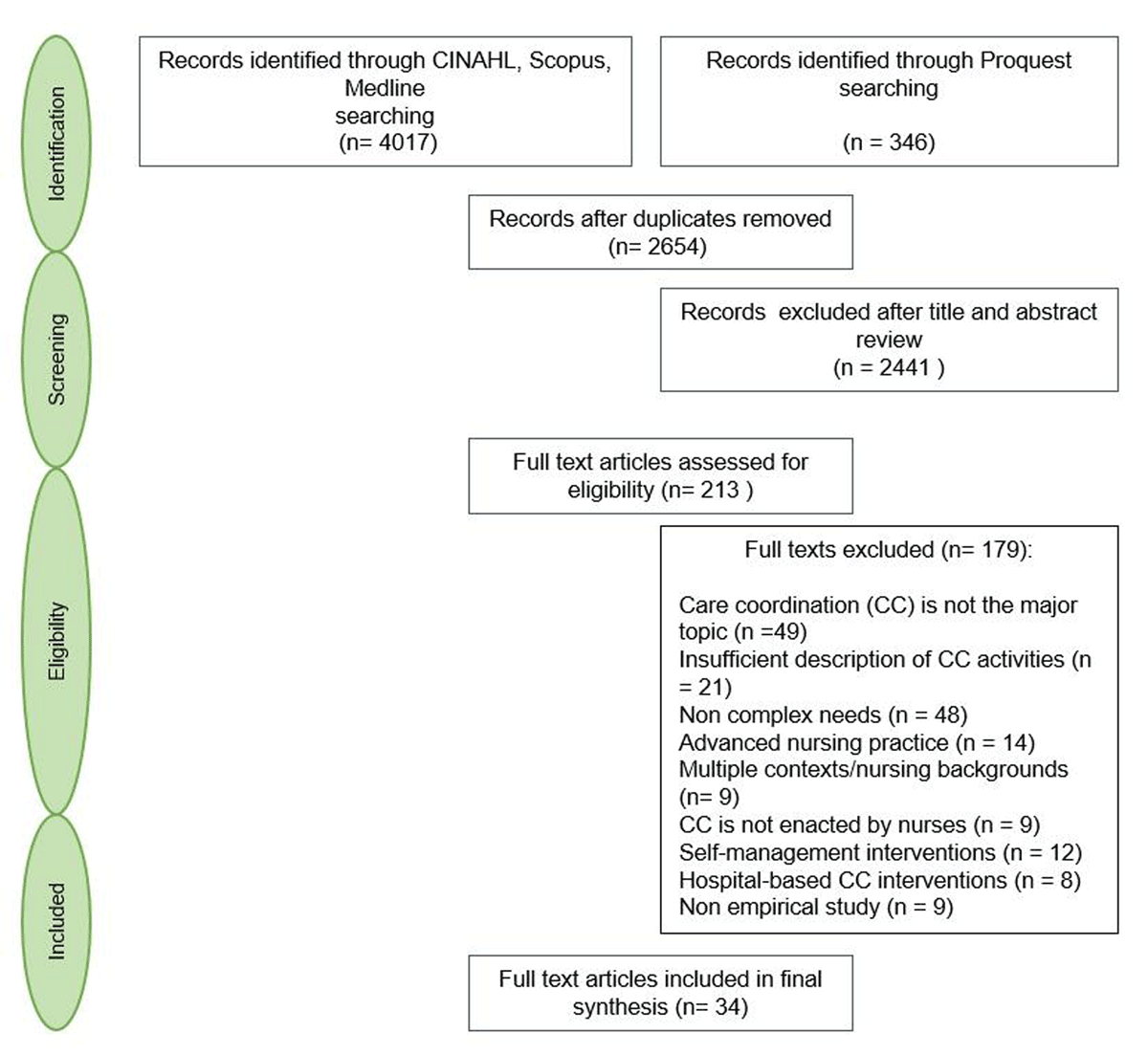
Figure 2
Flow diagram detailing search results and study selection.
Table 1
Included studies that address nursing care coordination for patients with complex needs in primary healthcare.
| AUTHORS, YEAR OF PUBLICATION | STUDY DESIGN/OBJECTIVES | CARE COORDINATION INTERVENTIONS | TARGET POPULATION | NURSE’S EMPLOYMENT ARRANGEMENT, LOCALISATION, CONTEXT | SUMMARY OF CARE COORDINATION ACTIVITIES |
|---|---|---|---|---|---|
| Aragonès & al; 2012 | Cluster RCT/Assess the effectiveness of a multi-component programme to improve the management of depression | Case management | Patients with moderate to severe depression | Exclusive case management role; Primary care centres, Catalonia, Spain | Provide self-management, psychological and emotional support; encourage and monitor adherence to treatment; monitor side effects and clinical results; improve social support; coordinate care between patient, primary care and specialized care providers; document information and transfer to GP |
| Berra & al; 2007 | Clinical trial and program dissemination project/Reflect on lessons learned in developing the “Heart to Heart” program | Case management | Low-income, ethnically-diverse populations at elevated risk of cardiovascular disease events | Exclusive case management role; Primary care clinics, California, USA | Provide intensive and individualized care and guideline-based pharmacotherapy; provide education and counseling; support behavior change; coordinate access to community resources; link and partner with GP and specialty services |
| Bleijenberg & al; 2016. (intervention described in Bleijenberg 2013) | Cluster RCT/Determine the effectiveness of a primary care program on the daily functioning of older people | Nurse-led care intervention | Community-dwelling frail people aged 60 and older | Exclusive care coordination role; General practices, the Netherlands | Assess patient’s needs at home; develop care plans; monitor and follow up; support caregivers; promote self management; coordinate care with GP and health care teams |
| Boyd & al; 2007 (same intervention as in Boyd 2008; Boult 2008; Boult 2011; and Boult 2013) | Pilot test and preliminary results of an RCT/Test the feasibility of a new model of health care designed to improve the quality of life and the efficiency of resource use | Guided care | Older patients with multimorbidity and functional disability and who had generated high insurance expenditures for health care | Exclusive care coordination role; Non-academic urban primary care practice, Baltimore, USA | Assess the global patient’s status at home; develop a plan of care; monitor, follow up and respond to change; communicate and coordinate the efforts of all involved health care professionals; support patient and caregivers’ activation, engagement and self-management using motivational interviewing; facilitate access to community resources; facilitate care transition |
| Coburn & al; 2012 | RCT/Evaluate the Health Quality Partners program’s effect on mortality | Community based nurse care management | 65 years of age and older with multimorbidity | Exclusive care management role; A network of primary care practices, eastern Pennsylvania, USA | Target eligible patients; visit at home when necessary; assess patient’s needs; develop a care plan; monitor, follow up and respond to change; support self management and behavior change; assess and promote patient adherence to treatment; reconcile errors/omissions with the GP; coordinate care with health and social care providers and family members; facilitate care transition; manage advance directives; document in patient records |
| Ekers & Wilson; 2008 | Audit of symptom outcome and satisfaction/Examine the impact of interventions delivered in routine primary care clinics by nurses | Case management | Patients with moderate to severe depression | Case management with other primary care duties; General practitioner practices, the North East of England | Assess patient’s symptoms and risk factors; manage medication; support behavioral activation; discuss cases with psychiatric nurse and GP; respond to changes |
| Friedman & al; 2009 | RCT/Report the impact of a primary care health promotion nurse intervention | Disease management | High risk patients with disability (or their caregiver) and recent significant (or expected) health care utilization | Exclusive disease management role; Home visits, counties in western New York, in West Virginia, and in Ohio, USA | Visit patient at home; assess their status; monitor medication list; provide education and support for self management and behavior change and maintenance; facilitate communication between patient and family and GP |
| Gabbay & al; 2013 | RCT/Determine whether the addition of nurse case managers to usual care would result in improved outcomes | Case management | Diabetic patients at high risk for complications, in an underserved Hispanic population | Exclusive case management role; Primary care clinics within two health systems in Central Pennsylvania, USA | Monitor and follow-up; provide counseling and enhance motivation to change and medication adherence; engage in phone and email conversations with patient between visits when needed; make referrals to specialty services when necessary; discuss medication list with GP |
| Hudon & al; 2015 (same intervention as in Hudon 2018) | Qualitative study/Examine the experience of patients and their family members with care integration in a case management program by primary care RN | Case management | Frequent users of health care services who had chronic diseases | Case management role with other primary care duties; Family medicine groups, Province of Quebec, Canada | Assess patient’s needs and resources; develop a personalized care plan; involve patient in decision-making; provide education, counseling, self management support; build trust through interpersonal communication; improve transition, communication and coordination with and among healthcare and community partners |
| Jansen & al; 2011 | RCT/Compare the effects of case management and usual care | Case management | Community-dwelling older adults with dementia symptoms and their informal caregivers | Exclusive case management role; Home visits, West-Friesland, the Netherlands. | Visit patient at home; assess patient and caregiver situation; formulate a care plan with them; provide them education; improve their social support; refer them to relevant healthcare professionals; monitor and follow-up; provide phone consultations; inform the GP; discuss cases with peers; document and share information |
| Katon et al; 2012 (same intervention as in Trehearne 2014) | RCT/Evaluate the cost-effectiveness of a collaborative treatment program | Collaborative care management | Patients with poorly controlled diabetes mellitus, CHD, or both and comorbid depression | Exclusive care management role; Primary care clinics of an integrated healthcare system, Washington State, USA. | Visit patient at home; identify clinical goals; develop individualized care plans; monitor, follow up and respond to change; provide patient education and support for self management; review and discuss cases with GP and specialists |
| Mastal & al; 2007 | Case study/Explore innovative practices in two disability care coordination programs | Care management | Adults with severe and persistent mental illness who had developed type II diabetes | Care management role with leadership responsibilities; Home visits, RN is located in both the community mental health center and the primary care center, Vermont, USA | Visit patient at home; assess their health; accompany them in their trips out of their home if desired; provide education and self management support; link the mental health and primary care systems; interact with, educate and learn from mental health providers; serve as a resource to patient and providers |
| McNab & Gillespie; 2015 (same nurses’ role as in McNab &al; 2016) | Case study/Report on a program that aims to improve coordination and integration of services, and reduce unnecessary hospital readmissions | Integrated care | Older people with chronic and complex illness who are at risk of further exacerbation and/or hospitalisation | Exclusive role of liaison nurse; Within the larger Mount Druitt Community Health Centre; in homes; and at general practitioner practices, West of Sydney, Australia | Visit patient at home; identify their needs; initiate care planning; support self-management, provide a single point of contact and a familiar face for patient and teams; manage communication, case conferencing and care coordination between professionals involved in patient’s care; make referrals into health and social care |
| Meng & al; 2009 | RCT/Evaluate the effect of a primary care nurse intervention on paid personal assistance use and expenditures | Disease management-health promotion | Community dwelling older people with disabilities and recent significant health care utilization | Exclusive role of disease management-health promotion; Home visits, New York, West Virginia, and Ohio, USA | Visit patient at home; co-create goals; collaborate with patient, GP and MDT to create care plans, support behavior change, medication management and treatment adherence; provide education and support for self management to patient and caregivers; facilitate transition and communication between the GP, patient and caregivers |
| Metzelthin & al; 2013 | Mixed methods/Examine the implementation of the interdisciplinary care approach and participants experiences | Case management | Community-dwelling frail older people (> 70 years) | Case management role with other primary care duties; General practices, the south of the Netherlands | Contribute to patients targeting; visit patient at home; perform a comprehensive assessment; inform and cooperate with patient, caregivers and MDT for the formulation and execution of a treatment plan; monitor and follow up; facilitate the protocol implementation |
| Newcomer & al; 2004 | RCT/Present patient outcomes after 12 months of participation to the preventive case management program | Case management | Older people with chronic condition | Exclusive case management role; Primary care medical groups within Sharp HealthCare of San Diego, California | Perform health risk screening and contribute to triage; formulate multidimensional care plan interventions; provide education; assist patient in preparing their appointments with the GP; monitor and facilitate treatment adherence; reconcile medication; provide referrals and assistance with services access; communicate with GP; facilitate health plan processes navigation; coordinate with the hospital discharge planners; monitor and adapt risk status |
| Roth & al; 2012 | Study cohort/Examine Community Care Managers’ assessments and interventions compared with PCP care | Care management | The most vulnerable older adults enrolled in a community Special Needs Plan (based on patient’s categories of diagnoses and disease severity to predict medical expenditures) | Exclusive care management role; Evercare Special Needs Plan site located in central Florida, USA | Visit patient at home; assess their needs; develop a personalized care plan; promote preventive services; engage with GP; provide health education and caregiver support; coordinate services; facilitate transitions and communication between all parties including the patient |
| Ruikes & al; 2016 | Cluster Controlled Trial/Evaluate the effectiveness of a general practitioner–led program integrating cure, care, and welfare for the prevention of functional decline | Case management | Community-dwelling frail older people (> 70 years) | Unclear*; General practices, Nijmegen, the Netherlands | Visit patient at home; involve them in setting goals based on the assessment of their needs; formulate individualized care plans; ensure patient acknowledges these plans; review medication with GP and pharmacist and document decisions in the care plan; maintain treatment contact with patient and caregivers; organize and participate to team meetings |
| Schraeder & al; 2008 | Non-randomized comparison/Test the effectiveness of a management intervention on healthcare utilisation and cost | Case management | Chronically ill community dwelling older people at high-risk for mortality, functional decline, or increased health services use | Exclusive case management role; Primary care practice, East central Illinois (intervention); West central Illinois (comparison), USA | Visit patient at home; perform a comprehensive assessment and integrate it with the GP’s; develop a care plan with the GP; adjust it when necessary; monitor and follow up; provide patient education and support for self management and behavioral change; monitor the need for educational interventions; visit patient during transitional periods and provide ongoing monitoring and assessment; build a personal relationship with patient; communicate with and transfer information to GP and team; coordinate supportive services |
| Scrymgeour & al; 2013 | Mixed methods/Assess the effectiveness of the Continuity of Cancer Care pilot | Care coordination | Patients with varying stages of cancer progression | Exclusive care coordination role; General practices in New Zealand | Provide emotional support, verbal guidance and support for self management to patient and family; include patient and family in care; respect patient’s values and beliefs; serve as a main point of contact available when needed; advocate on behalf of patient with other healthcare providers; link patient with GP, MDT and services |
| Spencer; 2019 | Quasi-experimental uncontrolled before and after design involving a retrospective review/Evaluate a quality improvement project | Care coordination | Underserved, uninsured community with Type II diabetes | Exclusive care coordination role; Community Health in Partnership Services (CHIPS) clinic, St. Louis City, Missouri, USA | Form a meaningful relationship with patient and providers; clarify roles and responsibilities with patient; act as a resource for the team; assist patient and family completing the plan of care; document; provide technical support; make referrals when necessary |
| Suijker & al; 2016 | Cluster Randomized Trial/Evaluate the effects of nurse-led multifactorial care to prevent disability | Care coordination | Patients aged 70 years and over at increased risk of functional decline | Exclusive care coordination role; General practices, north-west of the Netherlands | Visit patient at home; conduct a comprehensive assessment; co-construct care plan with patient and GP where roles are clearly defined; monitor and follow-up; collaborate with patient, GP and MDT |
| Thyrian & al; 2017 | Cluster Randomized Trial/Test the effectiveness and safety of Dementia Care Management | Care management | Patients aged 70 years and over, living at home, and diagnosed as having dementia | Exclusive care management role; General practices, municipalities of Mecklenburg-Western Pomerania, Germany | Visit patient at home; conduct a comprehensive assessment; discuss intervention tasks with MDT; inform the GP and establish an individualized care plan with them; cooperate with the caregiver, GP, and health and social care providers; manage treatment, care and medication; provide caregiver support and education; monitor and follow-up |
| Unutzer & al; 2008 | Prospective pilot study (mixed methods)/Test the feasibility of and generate preliminary evidence for the efficacy of a care management program | Care management | Patients aged 60 years and over with depression and osteoarthritis pain | Exclusive care management care; Primary care clinics, University of Washington’s Practice Network, Washington, USA | Conduct a comprehensive assessment; manage medication; support activation; provide education and support for self management; coordinate with GP and specialist; monitor and follow-up and respond to change |
| Van Leeuwen & al; 2015 | Economic evaluation and a stepped-wedge cluster-RCT/Evaluate the cost-effectiveness of the Geriatric Care Model | Integrated care | Frail persons aged 65 years and over at increased risk of functional decline | Exclusive care coordination role; Primary care practices, two regions in the Netherlands | Visit patient at home; conduct a comprehensive assessment; establish a care plan with GP; discuss it with patient; inform and involve patient in decision making; document; monitor and follow up; coordinate care with MDT and community network professionals |
| Yuille; 2015 | Qualitative descriptive study/Identify, from the perspective of RNs, the strengths, gaps, barriers, and opportunities for optimizing nursing roles in the delivery of cancer survivorship care in primary settings | Chronic disease management | Patients with varying stages of cancer progression | Chronic disease management with other primary care duties; Local Health Integration Networks across Ontario, Canada. | Establish a long standing and trusting relationship with patient; serve as their “go to” person; provide emotional support; provide education and support for self management; manage care; assist patient and family navigate through the healthcare system; arrange and coordinate services for them; facilitate access to community resources; facilitate transitions. |
[i] *Although the care coordination role is clearly described, it is unclear if the nurses are employed to carry out this role exclusively or combine care coordination with other primary care duties.
Legend:
CHD = Coronary heart disease
GP = General practitioner
MDT = Multidisciplinary teams
RN = Registered nurses
Table 2
Categories of identified patient populations with complex health and social needs.
| CATEGORIES OF PATIENT POPULATIONS WITH COMPLEX NEEDS | IDENTIFIED TARGET POPULATIONS IN INCLUDED STUDIES |
|---|---|
| 1. Patients with severe mental illness | Patients with moderate to severe depression [4352] |
| 2. Patients with common or severe mental illness + chronic condition(s) | Adults with severe and persistent mental illness who had developed type II diabetes [55] Patients with poorly controlled diabetes mellitus, coronary heart disease or both and comorbid depression [53] Patients aged 60 years and over with depression and osteoarthritis pain [58] |
| 3. Patients with social vulnerability + chronic condition | Low-income, ethnically diverse populations at elevated risk of cardiovascular disease events, including those with existing coronary heart disease or diabetes [44] Diabetic patients at high risk for complications, in an underserved Hispanic population [45] Underserved, uninsured community with type II diabetes [70] |
| 4. Older people with physical, cognitive, psychosocial or psychiatric vulnerabilities (+ significant healthcare use) | Community-dwelling frail people aged 60 and older [72] Community-dwelling frail older people (> 70 years) [4951] Patients aged 70 years and over at increased risk of functional decline [71] Frail persons aged 65 years and over at increased risk of functional decline [68] Older patients with multimorbidity and functional disability and who had generated high insurance expenditures for health care [32] Community dwelling older people with disabilities and recent significant health care utilization [60] High risk patients with disability (or their caregiver) and recent significant (or expected) health care utilization [59] The most vulnerable older adults (based on patient’s categories of diagnoses and disease severity to predict medical expenditures) [56] Chronically ill community dwelling older people at high-risk for mortality, functional decline, or increased health services use [50] |
| 5. Old age people + chronic condition(s) | Older people with chronic and complex illness who are at risk of further exacerbation and/or hospitalisation [66] 65 years of age and older with multimorbidity [33] Community-dwelling older adults with dementia symptoms and their informal caregivers [47] Patients aged 70 years and over, living at home, and diagnosed as having dementia [57] Older people with chronic conditions [48] |
| 6. Patients living a transition to end-of life/palliative stage | Patients with varying stages of cancer progression [6169] |
| 7. High costs and frequent users of health care services | Frequent users of healthcare services who had chronic diseases [46] |

Figure 3
A model of nursing care coordination activities for patients with complex needs.
Legend:
COC = Continuity of care
GP = General practitioner
MDT = Multidisciplinary teams (including health and social care professionals).
