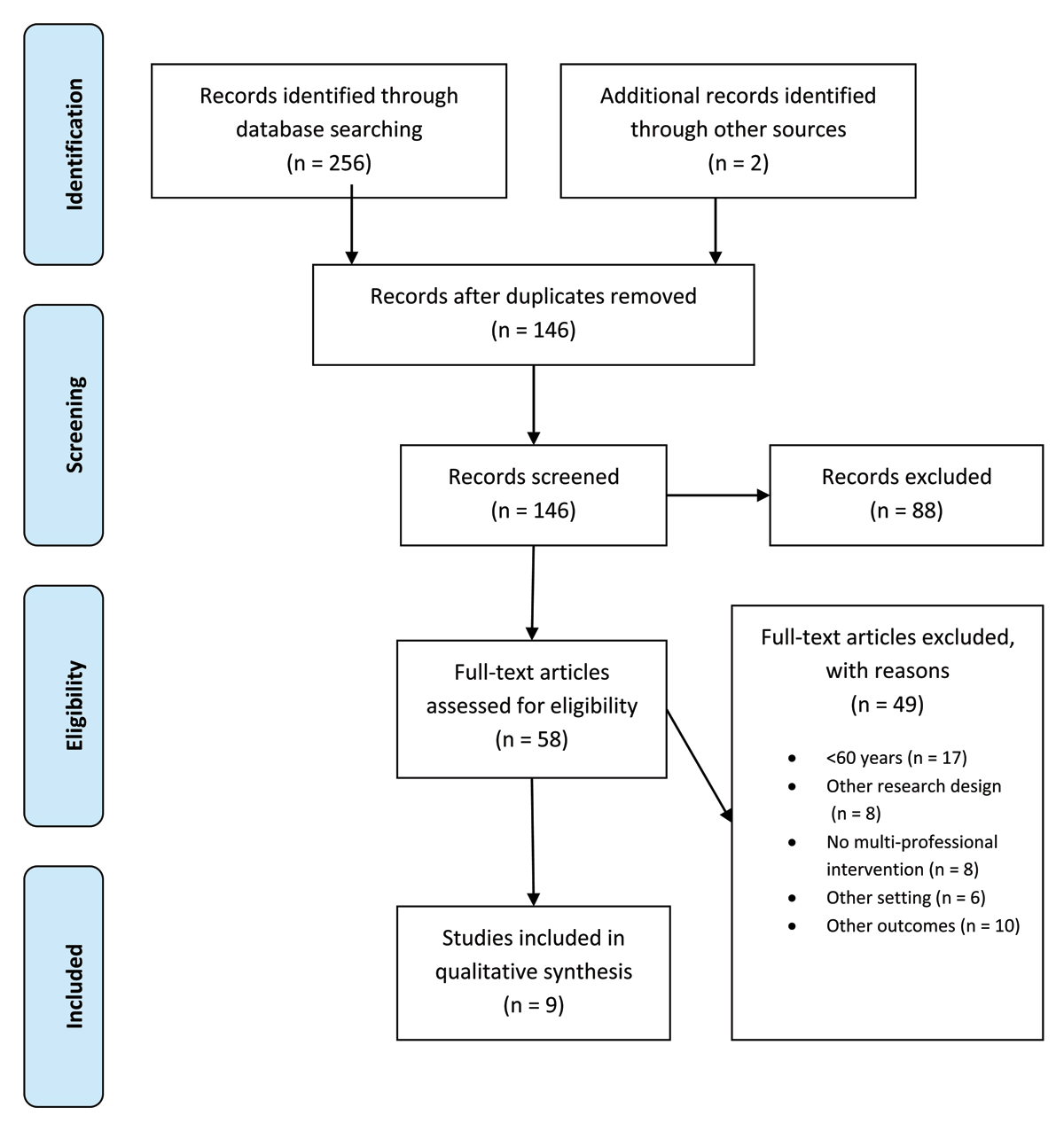
Figure 1
Flow chart. The flowchart illustrates the search strategy applied to answer the research question outlined. In total 258 studies were identified during the systematic data search (256 in scientific literature, two additional publications by hands-on search). Following qualitative evaluation and screening full text, only nine studies fulfilled predefined inclusion criteria of the study and were further processed in the review process.
Table 1
Summary of the risk of bias using Critical Appraisal for Therapy Articles Worksheet [14].
| Oxford Critical Appraisal | Azad et al. 2008 | Beck et al. 2015 | Courntey et al. 2009 | Deschodt et al. 2011 | Gillespie et al. 2009 | Hendriks et al. 2008 | Shyu et al. 2010 | Shyu et al. 2013 | Trombetti et al. 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Selectionbias | |||||||||
| Was the assignment of patients to treatments randomised? | Yes | Yes | Yes | Yes | yes | yes | yes | Yes | no |
| Were the groups similar at the start of the trial? | Yes | Yes | yes | Yes | yes | yes | yes | Yes | yes |
| Performancebias | |||||||||
| Aside from the allocated treatment, were groups treated equally? | Yes | Yes | no | yes | yes | yes | unclear | unclear | yes |
| Attritionbias | |||||||||
| Were all patients who entered the trial accounted for? Were they analysed in the groups to which they were randomised? | Yes | Yes | yes | yes | unclear | yes | yes | Yes | unclear |
| Observerbias | |||||||||
| Were measures objective or were the patients and clinicians kept “blind” to which treatment was being received? | No | No | yes | no | no | no | yes | no | yes |
[i] The critical appraisal was performed with the Critical Appraisal for Therapy Articles Worksheet – Centre for Evidence-based Medicine, University of Oxford 2005. Possible answers were “yes”, “no” and “unclear”.
Table 2
Study characteristics.
| Patients (n) | Intervention (n) | Comparison (n) | Mean age (years) | Country | |
|---|---|---|---|---|---|
| Azad et al. 2008 | 91* | 45 | 46 | 75,0 | Canada |
| Beck et al. 2015 | 71 | 34 | 37 | 85,0 | Denmark |
| Courntey et al. 2009 | 122 | 58 | 64 | 78,8 | Australia |
| Deschodt et al. 2011 | 171 | 94 | 77 | 80,8 | Belgium |
| Gillespie et al. 2009 | 368 | 182 | 186 | 86,75 | Sweden |
| Hendriks et al. 2008 | 333 | 166 | 167 | 74,85 | Netherlands |
| Shyu et al. 2010 | 162 | 80 | 82 | 78,15 | Taiwan |
| Shyu et al. 2013 | 299 | CC (99) IC (101) | 99 | 76,51 | Taiwan |
| Trombetti et al. 2013 | 122 | 92 | 30 | 84 | Switzerland |
[i] Abbreviations: CC= Comprehensive Care, IC= Interdisciplinary Care; * women only.
Table 3
Multi- and inter-professional team composition.
| Physician | Nurse | Physio-therapist | Dietician | Occupational-therapist | Pharmacist | Psychiatrist | Social-worker | Additional partners of care | Inter-disciplinary | Multi-disciplinary | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Azad et al. 2008 | X | X | X | X | X | X | X | X | X | ||
| Beck et al. 2014 | (x) | X | X | X | X | X | |||||
| Courtney et al. 2009 | X | X | X | ||||||||
| Deschodt et al. 2011 | X* | X* | X* | X* | X* | X | |||||
| Gillespie et al. 2009 | X | X | X | ||||||||
| Hendriks et al. 2008 | X* | X* | X | X | |||||||
| Shyu et al. 2010 | X* | X* | X | X | |||||||
| Shyu et al. 2013 | X* | X* | X | X | (X) | X | |||||
| Trombetti et al. 2012 | X | X | X | X | X | (X) | X | X |
[i] * With expertise in geriatric care, (X) can be consulted if necessary.
Table 4
Multi-professional and inter-professional interventions and strategies.
| Clinical setting | |||||
|---|---|---|---|---|---|
| Author | Design | Strategy | Components of the intervention | CG | Frequency |
| Deschodt et al. 2011 | RCT | Inpatient Geriatric consultation [24] | CGA from nurse to detect potential problems. In-depth multidisciplinary evaluation of assessed problems. Formal clinical advice and recommendations documented in electronic form and discussed in health care team. In-hospital follow-up to check for new problems and if team’s advice were implemented or needed more clarification. | UC | during hospital stay |
| Gillespie et al. 2009 | RCT | Comprehensive pharmacist intervention | After admission the pharmacist summarized patient’s medication list and conducted an interview to give advices for medication intake. During inpatient stay, the pharmacist performed a comprehensive drug review [25], discussed drug related problems with health care team during ward rounds and give advices to patient’s physician. At Discharge the pharmacist provided medication counselling as a complement to the physicians discharge information. A comprehensive discharge letter was faxed to patients GP. To ensure adequate medication home management and record any changes in medication, the pharmacist contacted patients by telephone 2 months after discharge. | UC | Admission to discharge, 2-month telephone follow-up to ensure home management of medications |
| Trombetti et al. 2013 | CT | Multi-disciplinary multifactorial intervention program | Multidisciplinary comprehensive assessment to define fall and fracture risk factors. Followed by an individually tailored intervention this included targeted rehabilitation therapy (physician, physiotherapist, occupational therapist, dietician, nurse, social worker). Additional physiotherapeutic group sessions, eurhythmics workshops and workshops with an occupational therapist. A systematic battery of tests and multidisciplinary team meetings were performed weekly to review and adopt rehabilitation program. Whenever required, a home visit was undertaken before patient’s discharge to assess environmental hazards and facilitate modifications. | UC | 5 weekly group sessions (a 60 min) and 3 to 5 individually tailored sessions of 30–45 min. Home visit when required. |
| Clinical setting and home based intervention | |||||
| Author | Design | Strategy | Components of the intervention | CG | Frequency |
| Azad et al. 2008 | RCT | Structured multi-disciplinary pathway | Group and home based exercise program (Physiotherapist), nutrition counselling (dietician), energy and stress management (occupational Therapist), counselling patients & families (social worker), CHF education of patients and caregivers (clinic coordinator). | UC | 12 visits over 6 weeks and home based exercise program |
| Beck et al. 2014 | RCT | Multidisciplinary discharge liaison-Team with dietician | Discharge Liaison-Team (nurse, occupational Therapist, physiotherapist) test and install aids, review discharge letter, contact GP if relevant and organise home care.. Additional home visits from a dietician to develop and implement individual care plan. | DL | home visits from a dietician at discharge, and after 3 and 8weeks |
| Courtney et al. 2009 | RCT | Discharge Planning and In-home follow-up Protocol (OHP-DP) | Physical exercise intervention from a physiotherapist included muscle stretching, balance training and walking. A nurse developed a transitional care plan including need for assistance, post discharge treatments, follow-up care, social support, chronic disease and medication management. Nurse and physiotherapist combined their visits when panning, explaining and demonstrating exercise program. 48h after discharge, home visit from the nurse to provide and advice support and ensure that exercise program could be safely undertaken at home. Additional home visits were provided if required. Weekly telephone follow-up calls for 4 weeks, followed by monthly calls for 5 months. Contact nurse was possible from 9am to 5pm on weekdays. | UC | Start within 72h after admission and continued through hospitalization. A home visit from a nurse within 48 hours and telephone follow-up for 6 months |
| Hendriks et al. 2008 | RCT | Multidisciplinary fall-prevention program[26] | Structured medical assessment of risk factors for new falls from physician included for example standard examination, vision, sense of hearing, locomotor apparatus, feet and footwear as balance and mobility and the affect (in hospital) Home based assessment from an occupational therapist included functional assessment, environmental hazards and psychological consequences of the fall. Finally a summary of the results were sent to the participant’s GP with recommendations and referrals. | UC | Medical and home based assessment After 2,5–3,5 months all recommendations had to be implemented |
| Shyu et al. 2010 | RCT | Interdisciplinary Intervention for Hip Fracture | Geriatric assessment and consultation from a geriatric nurse and a geriatrician. Inpatient rehab program from physio therapist, geriatric nurse and rehabilitation physician. Continuous rehab included inpatient rehab (nurse, physio therapist, rehab physician) and individual at home rehab program (nurse, physio therapist) At discharge planning a geriatric nurse did predischagre assessment (resources, self-care ability needs, long term care service, and referrals) home environmental modifications. A telephone call was done to remind follow up visits. | UC | 2x CGA and Home visits from a geriatric nurse und physio therapist |
| Shyu et al. 2013 | RCT | Interdisciplinary care model and Comprehensive care model | 1 interdisciplinary care model: geriatric consultation with medical supervision (nurse and geriatrician), rehab program focused on relieving pain, muscle strength and endurance, discharge planning with post-hospital service (discharge assessment, referrals and reminders for clinical follow-up) 2 Comprehensive care model: included the components of the interdisciplinary care model and additional assessment of nutritional status, depression and fall before discharge. Those with a risk of malnutrition, depression and fall received additional services. The rehab protocol was same for both groups. | UC | Rehab program (4 months in group 1, 6 months in group 2) with home visits from nurse and physio therapist |
[i] Abbreviations: CG = control group, RCT = randomised controlled trial, CT = controlled trial, UC = usual care, DL = discharge liaison team, CGA = comprehensive geriatric assessment, CHF = chronic heart failure.
