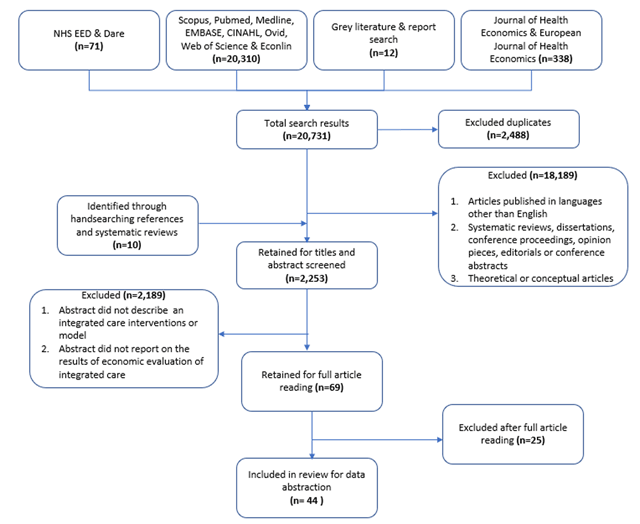
Figure 1
Flowchart of study inclusion at various stages of the selection process.
Table 1
Description of study, patient and intervention characteristics.
| Study characteristics | Patient characteristics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Country | Study design | Type of economic evaluation | Pers-pective | Inter-vention Size | Control Size | Observation period | Target population | Intervention description | Setting | Study objective(s) | Measures |
| Zulman et al. (2017) | USA | RCT | Cost-consequence | Health care payer | 150 | 433 | 17 months | High healthcare users (top 5%) | The ImPACT multidisciplinary team addressed health care needs and quality of life through comprehensive patient assessments, intensive case management, care coordination, and social and recreational services | Primary care medical home | To evaluate the impact of augmenting the Veterans Affairs’ medical home and multidisciplinary team with an intensive management program | Outcomes: 1) patient satisfaction, 2) patient activation measures; Cost: inpatient and outpatient services |
| Weisner et al. (2001) | USA | RCT | Cost-effectiveness | Health care payer | 285 | 307 | 6 months | Adults with alcohol and drug dependence | Patients received treatment through an integrated model, in which primary health care was included within the addiction treatment program | Primary care within substance abuse program | Examine differences in treatment outcomes and costs between integrated and independent models of medical and substance abuse care | Outcomes: 1) alcohol and drug abstinence rate, 2) healthcare utilization; Cost: inpatient, outpatient and treatment costs |
| Weeks et al. (2009) | USA | Cross-sectional | Cost-comparison | Health care payer | 63,647 | 677,901 | NA | Individuals 65 years and older under Medicare | The intervention group was assignment to a large multispecialty group practice in accountable care organizations. Each beneficiary was assigned to a unique primary care physician for a 2-year period. | Multispecialty primary care group practice | Compare the costs and quality of care provided to Medicare beneficiaries by physicians who worked within large multispecialty physician group practices | Outcomes: 1) outpatient clinical measures, 2) ambulatory care-sensitive hospitalisations; Cost: inpatient, long-term and home care |
| Weaver et al. (2009) | USA | Cluster RCT | Cost-consequence | Health care payer | 232 | 199 | 12 months | Individuals with HIV, mental illness and substance abuse disorders | Integrated HIV primary care, mental health, and substance abuse services among triply diagnosed patients. | Outpatient multidisciplinary mental health, substance abuse and case management services | Evaluate the cost-effectiveness of integrating HIV primary care, mental health, and substance abuse services amongst triply diagnosed patients | Outcomes: 1) quality of life, 2) mental health scores; Cost: 1) inpatient, outpatient, rehabilitation, home care, alternative, primary care, long-term care; 2) out-of-pocket expenses |
| Van Orden et al. (2009) | The Netherlands | Cluster RCT | Cost-consequence | Health care payer | 102 | 63 | 12 months | Adults with mental illness | Patients with mental illness were assigned to collaborative care program in a primary care setting through traditional referral of patients to mental health services | Primary care and specialized mental health care | Compare the effect of introducing collaborative care on the attached mental health professional model in a primary care setting | Outcomes: 1) quality of life, 2) satisfaction with care, 3) mental health score; Costs: treatment costs |
| Olsson et al. (2009) | Sweden | Pre-post cohort | Cost-effectiveness | Health care payer | 56 | 56 | 18 months | Community dwelling older adults 65 years and older, with hip fracture | Patient centered integrated care pathway for patients admitted with hip fracture. | Multidisciplinary orthopedic hospital ward | Compare costs and consequences of integrated care pathways for patients admitted with acute hip fractures | Outcomes: 1) activities of daily living score; Cost: 1) intervention and operational costs, 2) implementation costs, 3) inpatient costs |
| Leeuwen et al. (2015) | The Netherlands | Cluster RCT | Cost-utility | Societal perspective | 456 | 691 | 24 months | Community dwelling older adults with frailty | The Geriatric Care Model combined regularly scheduled in-home comprehensive geriatric assessments by practice nurses followed by a customized care plan management and training of practice nurses by a regional geriatric expert team | Multidisciplinary geriatric primary care team | Evaluate the cost-effectiveness of the Geriatric Care Model compared to usual primary care | Outcomes: 1) quality adjusted life years, 2) activities of daily living; Costs:1) inpatient, primary, outpatient, home and long-term care & medication costs, 2) informal care giver costs |
| Lanzeta et al. (2016) | Spain | Cluster RCT | Cost-utility | Health care payer | 70 | 70 | 12 months | Individuals with multimorbidity | An integrated healthcare model comprising an assigned internist and a hospital liaison nurse for patients with multimorbidity | Primary and hospital-based care | Examine the effectiveness of an integrated model for patients with multimorbidity, based on an assigned internist and a hospital liaison nurse | Outcomes: 1) quality adjusted life years, 2) health resource utilization; Costs: 1) acute, specialists, primary and home care, 2) treatment costs |
| Goorden et al. (2013) | The Netherlands | RCT | Cost-utility | Societal perspective | 65 | 61 | 12 months | Employees sick-listed due to major depressive disorder | Collaborative care for major depressive disorder in an occupational healthcare setting | Occupational health setting and consulting specialist care | Evaluate the cost-utility of a collaborative care intervention in sick-listed employees with major depressive disorder | Outcomes: 1) quality adjusted life years, 2) health care utilization; Costs: 1) primary, specialist care and intervention costs, 2) productivity loss |
| Boland et al. (2015) | The Netherlands | Cluster RCT | Cost-utility | Societal perspective | 554 | 532 | 24 months | Patients with chronic obstructive pulmonary disease | A multidisciplinary team was trained in motivational interviewing, setting up individual care plans, exacerbation management, implementing clinical guidelines and redesigning the care process | Multidisciplinary primary care teams | Examine the cost-effectiveness of a disease management program for patients living with chronic obstructive pulmonary disease | Outcomes: 1) quality adjusted life years, 2) symptom improvement; Costs: 1) acute, primary, rehabilitation and home care, 2) productivity loss and travel costs |
| Donohue et al. (2014) | USA | RCT | Cost-utility | Health care payer | 150 | 152 | 12 months | Patients with depression following coronary artery bypass graft (CABG) surgery | Patients who screened positive for depression after CABG surgery received an 8-month centralized, nurse-provided and telephone-delivered CC intervention for depression | Primary care and specialized outpatient mental health care | Examine the impact of telephone-delivered collaborative care of treating post-CABG surgery depression compared to usual care | Outcomes: 1) quality adjusted life years, 2) depression free days; Costs: acute and outpatient costs |
| Cohen et al. (2012) | Canada | Pre-post cohort | Cost-consequence | Societal perspective | 81 | Self-comparator | 12 months | Children with medically complex chronic conditions | Clinics at two community hospitals distant from tertiary care were staffed by local community pediatricians with the tertiary care center nurse practitioner and linked with primary care providers | Outpatient clinics within community-based hospitals with pediatricians, linked with primary care | Evaluate the effectiveness of a community–based complex care clinic integrated with a tertiary care facility | Outcomes: 1) health related quality of life; 2) perceptions of care; Cost; 1) inpatient, primary, outpatient and home care. 2) Out-of-pocket expenses for health and social care |
| Wise et al. (2006) | USA | Cohort | Cost-comparison | Health care payer | 2010 | 30,360 | 12 months | Older adults, 65 years and older, with chronic conditions | A prospective health risk assessment, point-of-care information management, clinical decision support, multidisciplinary clinical oversight, and a clinical “Health Navigator” to deliver integrated health care | Multidisciplinary primary care teams | Assess the impact of an integrated set of care coordination tools and chronic disease management interventions on utilization and cost | Cost: adjusted acute, primary care and drug costs |
| McCall et al. (2010) | USA | Cohort | Cost-consequence | Health care payer | 2,619 | 2490 | 36 months | Older adults, aged 65 and older who are high cost Medicare users | The intervention was a practice-based care management services to high-cost Medicare beneficiaries. Case managers, who were assigned to each physician office, developed relationships with program participants to provide support across the continuum of care | Multidisciplinary colocated primary care teams with linkages to home and long-term care | Evaluate whether the Massachusetts General Hospital and its case management program can meet targeted cost-savings compared to control | Outcomes: 1) comorbidity score, 2) care experience and satisfaction; 3) healthcare utilization; Cost: 1) covered inpatient, primary, outpatient and home care |
| Simon et al. (2001) | USA | RCT | Cost-effectiveness | Health care payer | 110 | 109 | 6 months | Primary care patients with major depressive episode | Stepped collaborative care for patients with persistent depressive symptoms after usual primary care management. Patients received collaborative care with liaison psychiatrist and primary care physician. | Large primary care clinics part of a health cooperative | Evaluate the incremental cost-effectiveness of stepped collaborative care for patients with persistent depressive symptoms after usual primary care management | Outcome: 1) depression-free days; Costs: outpatient, primary, specialists and inpatient care |
| Hebert et al. (2008) | Canada | Pre-post cohort (D-in-D) | Cost-consequence | Health care payer | 501 | 419 | 48 months | Older adults aged 65 living with frailty and disability | Integrated Service Delivery System developed to improve continuity and increase the efficacy and efficiency of services, especially for older and disabled populations | Population level health and social care including: acute, home, long term, rehab and social services | Evaluate the impacts of integrated care model for older adults on the use of services and on costs in the experimental zone, compared with the comparison zone | Outcomes: 1) functional and mental health scores; 2) care satisfaction; 3) care giver burden; Costs: 1) implementation and operation costs, 2) primary, specialist, acute and outpatient costs |
| Vroomen et al. (2012) | The Netherlands | Cluster RCT | Cost-utility | Societal perspective | 201 | 136 | 6 months | Older adults living in residential homes | The intervention consisted of quarterly in-home assessment of residents, multidisciplinary team meetings with primary care physicians, nurse and physiotherapists, and multidisciplinary consultations | multidisciplinary residential home care linked with primary care | Evaluate the cost-effectiveness of a multidisciplinary integrated care in residential homes | Outcomes: 1) quality adjusted life years, 2) functional status, 3) quality of care scores; Costs: 1) acute, primary, outpatient/specialist care, 2) operational/implementation costs; 3) informal caregiver productivity loss |
| Salmon et al. (2012) | USA | Pre-post cohort | Cost-comparison | Health care payer | 39,982 | Self-comparator | 12 months | Patients enrolled in collaborative accountable primary care organizations | A collaborative accountable care model with registered nurses who served as care coordinators were a central feature of the initiative. They used patient-specific reports and practice performance reports to improve care coordination, identify gaps, and address opportunities for quality improvement | primary care physician group practice | Examine the impact of accountable coordinated care initiative in three diverse provider practices before and after implementation | Outcomes: 1) Outpatient/primary care clinical measures; Cost: 1) Inpatient and primary care, 2) intervention cost |
| Looman et al. (2016) | The Netherlands | Pre-post cohort | Cost-utility | Societal perspective | 254 | 249 | 12 months | Community dwelling older adults with frailty | Primary care physician served as the care coordinator and single-entry point for the elderly. Nurse practitioner visited patients for cognitive, mental and functional assessment who also provided case management. A multidisciplinary treatment plan was then developed. | Multidisciplinary primary care team linked with nursing home and outpatient/specialist care | Examine the impact of integrated model for community-dwelling older adults with frailty | Outcome: 1) quality adjusted life years; Cost: 1) inpatient, primary, home, outpatient and nursing home care, 2) intervention operational costs, 3) Informal care giver costs |
| Celano et al. (2016) | USA | RCT | Cost-utility | Health care payer | 92 | 91 | 6 months | Patients hospitalized for cardiovascular illness with mental illness | Psychiatric treatment in the intervention was provided in concert with the patients’ primary medical clinicians—within a framework supervised by a psychiatrist | Inpatient care followed by with telephone outpatient follow up, with primary care linkages | Examine the cost-effectiveness and differences in healthcare utilization and cost between collaborative depression and anxiety program with usual care | Outcomes: 1) quality adjusted life years, 2) mental health status; Costs: 1) acute, primary, outpatient/specialist care |
| Markle-Reid et al. (2010) | Canada | RCT | Cost-consequence | Societal perspective | 55 | 54 | 6 months | Community dwelling older adults, 75 years and older, at risk for falls | A six-month multifactorial and evidence based falls prevention strategy involving a multidisciplinary team | Multidiscplinary home care linked with primary care and community services | Determine the effects and costs of a multifactorial, multidisciplinary team approach to falls prevention compared with usual home care services. | Outcomes: 1) falls; 2) clinical outcomes (functional, mental and cognitive scores); 3) quality adjusted life years; Cost: 1) Acute, home, primary and community care, 2) out-of-pocket indirect medical expenses |
| Pozzilli et al. (2002) | Italy | RCT | Cost-consequence | Health care payer | 133 | 68 | 12 months | Patients diagnosed with multiple sclerosis | The home-based multidisciplinary team collaborated with the patient, physician, and caregiver in designing individualized clinical care and in coordinating home services with hospital care | Multidisciplinary home care with specialists linkages | Compare the effectiveness and the costs of multidisciplinary home-based care in multiple sclerosis with hospital care | Outcomes: 1) quality of Life, 2) health resource utilization; Costs: 1) inpatient, outpatient and home care, 2) intervention costs |
| Tzeng et al. (2007) | China | RCT | Cost-consequence | Health care payer | 257 | 247 | 6 months | Individuals diagnosed with schizophrenia | A network of mental health services was created by coordinating a general acute care hospital, a day hospital, a psychiatric rehabilitation institution, a community rehabilitation center, home visit providers, a specialized psychiatric hospital, and local clinics | Network of acute care, day hospital, rehabilitation, home care providers and local clinics | Compare the cost-effectiveness of an integrated model of schizophrenia treatment with those of the traditional treatment model provided by acute care | Outcomes: 1) quality of life, 2) care giver burden, 3) health service utilization, Costs: inpatient, outpatient, rehabilitation and home care |
| Bergmann et al. (2017) | Malawi and Mozambique | Pre-post cohort (D-in-D) | Cost-effectiveness | Health care payer | Not reported | Not reported | 24 months | Children under 5 years with HIV who were underweight | Integration of health and nutrition program areas identified as important in reducing the vulnerability of children impacted and infected by HIV/AIDS: infant and young child feeding, prevention of mother-to-child transmission of HIV, pediatric HIV care and treatment, and community-based management of acute malnutrition | Community based health workers and community clinics for HIV and acute under-nutrition | To estimate the impact and cost-effectiveness for integrated HIV and nutrition service delivery in sub-Saharan Africa | Outcomes: 1) HIV infections averted, 2) undernutrition cases cured, 3) disability adjusted life years; Cost: 1) intervention costs, 2) operational/implementation costs, 3) life long HIV treatment cost |
| Koch et al. (2017) | USA | Pre-post cohort (D-in-D) | Cost-comparison | Health care payer | 2.5 million per year | 2.5 million per year (their own control) | 15 months | Patients served by hospital and physician groups merged as part of horizontal integration of care | Vertical integration through a set of physician acquisitions by hospital systems | Hospital, primary and specialist care physicians | Assess how (financial) vertical integration affects volume and cost of services provided by acquired physicians and hospitals | Outcome: health care utilization; Cost: acute, primary and outpatient/specialist care |
| Rosenheck et al. (2016) | USA | Cluster RCT | Cost-utility | Health care payer | 223 | 181 | 24 months | Individuals aged 15-40 in treatment for first episode of psychosis | A multidisciplinary, team-based treatment approach for first episode psychosis. This included: personalized medication management, family psychoeducation, individual, resilience-focused illness self-management therapy, and supported education and employment | Multidisciplinary community mental health treatment clinics | Compare the cost-effectiveness of a comprehensive, multidisciplinary, team-based treatment approach for first episode psychosis to usual community care | Outcomes: 1) quality adjusted life years, 2) health service utilization; Costs: 1) inpatient, outpatient, residential and nursing home care and medication costs, 2) implementation and operational costs |
| Sahlen et al. (2016) | Sweden | RCT | Cost-utility | Health care payer | 36 | 36 | 6 months | Patients diagnosed with congestive heart failure | The patients were offered structured person-centered palliative care at home with easy access to care, and the team was responsible for the total care, including co-morbidities | Multidisciplinary palliative home care team linked with specialist care | To assess the cost-effectiveness of person-centered integrated heart failure and palliative home care | Outcomes: 1) quality adjusted life years; Costs: 1) acute, home, primary and specialist care, 2) intervention cost |
| Blom et al. (2016) | Netherlands | RCT | Cost-consequence | Societal perspective | 3145 | 4133 | 12 months | Community-dwelling older adults, 75 and older living with complexity | The general practitioner (GP) or the practice nurse (under supervision of the GP) made an integrated care plan for participants with complex problems. Other care professionals were involved where needed through multidisciplinary consultations | General Practice with geriatric assessment training | Assess the effectiveness and cost- effectiveness of a monitoring system to detect the deterioration in somatic, functional, mental or social health | Outcomes: 1) quality of life, 2) activities of daily living, 3) satisfaction with care 4) Informal care giver time; Cost: 1) acute, primary, outpatient, nursing home and medication 2) intervention costs, 3) implementation costs, 4) informal care costs |
| Pimperl et al. (2017) | Germany | Pre-post cohort | Cost-consequence | Health care payer | 5411 | 5411 | 48 months | Individuals enrolled with the accountable care organization insurance scheme | Accountable care organization focused on population health management with a Triple Aim framework | Cross-sectoral cooperation of physicians, hospitals, social care, nursing staff, therapists, and pharmacies | Identify an appropriate study design for evaluating population health outcomes of accountable care organization such as based on shared savings contract | Outcomes: 1) survival, 2) comorbidity score; 3) Costs: outpatient physician and specialist care, hospital, rehabilitation, medication costs |
| Schellenberg et al. (2004) | Tanzania | Cohort | Cost-consequence | Societal perspective | 100,000 | 100,000 | 24 months | Children with malaria, pneumonia, malnutrition and diarrhea | The intervention was designed to increase children’s survival at household, community, and referral levels, with three components: improvements in case-management, improvements in health systems, and improvements in family and community practices | Family and community primary care practices and hospitals | Assess the effectiveness of facility- based integrated management of childhood illness in rural Tanzania | Outcomes: 1) child health outcomes, 2) household health behavior 3) children’s mortality; Costs: 1) drugs and vaccines, 2) implementation costs & operational costs, 3) intervention costs, 4) out-of-pocket expenses, 5) acute, primary and community care costs |
| Bird et al. (2012) | Australia | Pre-post cohort | Cost-consequence | Health care payer | 223 | Self-comparator | 36 months | Children with asthma that presented frequently at the emergency department | Patients received care facilitators who provided assistance in the promotion of carer/self-management, education and linkage to an integrated healthcare system, comprising of acute and community-based healthcare providers. | Acute, primary and other community-based care | Assess a model of care for pediatric asthma patients aimed to promote health and reduce their acute care utilizations | Outcomes: 1) activity limitation and emotional function, 2) acute care utilizations; Cost: 1) intervention costs; 2) acute care costs |
| Goltz et al. (2013) | Germany | Cohort | Cost-consequence | Health care payer | 2455 | 2455 | 36 months | Patients with osteoporosis who experienced index fractures | Patients received multidisciplinary cooperation between different sectors of the health care system, improved diagnostics, optimized drug therapy as well as encouraging lifestyle changes such as adequate nutrition and exercise. | Ambulatory care | Evaluate the outcomes of patients participating in a program of integrated care for osteoporosis in terms of medication supply, fracture incidence and expenses | Outcomes: 1) fracture Incidence, 2) occurrence of pain; Costs: 1) acute care costs, 2) treatment costs, 3) medication costs |
| Steuten et al. (2007) | Netherlands | pre-post cohort | Cost-utility | Societal perspective | 2455 | 2455 | 60 months | Patients 18 years and older with GP diagnosis of asthma | Care was delivered by a collaborative practice team consisting of a pulmonologist, primary care physician, and respiratory nurse specialists. The respiratory nurse specialists act as liaison between primary and secondary care | primary care collaborating with specialists | Assess long-term cost-utility of a disease management program for adults with asthma was assessed compared to usual care | Outcomes: 1) quality adjusted life years, 2) asthma related exacerbations/control; costs: 1) acute, primary and outpatient/specialist care costs, 2) medication costs 3) treatment costs, 4) implementation and operational costs, 5) patient productivity loss |
| Wiley-Exley et al. (2009) | USA | Cluster RCT | Cost-utility | Societal perspective | 1257 | 1948 | 6 months | Older adults, 65 years and older with major depressive disorder in primary care | Patients required referral to a behavioral health provider outside the primary care setting, and the behavioral health provider had primary responsibility for the mental health/substance abuse needs of the patient | Multidisciplinary specialist team colocated in primary care | Compare the cost-effectiveness of integrated care in primary care to enhanced specialty referral for older adults with behavioral health disorders | Outcomes: 1) depression free days, 2) quality adjusted life years; Costs: 1) inpatient, emergency room use, nursing home, rehabilitation care. 2) medication costs, 3) caregiver and patient indirect costs (transportation, productivity loss) |
| Karow et al. (2012) | Germany | Cohort | Cost-utility | Health care payer | 64 | 56 | 12 months | Adults patients diagnosed with first or multiple-episode schizophrenia | Patients receive a multidisciplinary team with a small client/staff ratio, home-treatment, high-frequent treatment contacts, no dropout policy and 24-hour availability | Inpatient, outpatient/specialists and occupational therapy care | To compare the cost effectiveness of therapeutic assertive community treatment with standard care in schizophrenia. | Outcomes: 1) quality adjusted life years, Costs: 1) inpatient care, day-clinic care, outpatient and specialist care costs, 2) medication costs |
| Renaud et al. (2009) | Burundi | Cohort | Cost-effectiveness | Health care payer | 149 | Self-comparator | 60 months | People living with HIV who initiated antiretroviral treatment | Care was given in primary health care facilities, which favours a more personal link with patients. Secondly, these health facilities delivered integrated care for people living with HIV. | Primary care based on non-for-profit organization delivering care for individuals living with HIV | Calculate the incremental cost effectiveness of an integrated care package for people living with HIV/AIDS in a not-for-profit primary health care centre. | Outcomes: 1) disability adjusted life years; Cost: 1) outpatient, acute and home care costs 2) medication costs 3) intervention costs, 4) food support costs |
| Tanajewski et al. (2015) | United Kingdom | RCT | Cost-utility | Health care payer | 205 | 212 | 3 months | Older people at risk of adverse outcomes after acute care discharge | This intervention comprised geriatrician assessment of patients on the acute medical unit and further short-term community follow-up to continue the assessment and oversight of the delivery of medical and non-medical community interventions | Multidisciplinary acute care team and links to primary care | To examine the cost-effectiveness of a specialist geriatric medical intervention for frail older people in the 90 days following discharge from an acute medical unit | Outcomes: 1) quality adjusted life years; Costs: 1) acute, primary and specialist care; 2) intervention costs |
| Lambeek et al. (2010) | Netherlands | RCT | Cost-utility | Health care payer | 66 | 68 | 12 months | Individuals visiting outpatient clinic due to low back pain | Integrated care consisted of a workplace intervention based on participatory ergonomics, with involvement of a supervisor, and a graded activity programme based on cognitive behavioural principles | Occupational health setting linked with multidisciplinary outpatient team | To evaluate the cost effectiveness of an integrated occupational health programme for sick listed patients with chronic low back pain | Outcomes: 1) duration until sustainable return to work; 2) quality adjusted life years; Costs: 1) primary and secondary care, home care, and drugs. 2) Out of pocket expenses for additional and informal care; 3) patient productivity loss |
| Bertelsen et al. (2017) | Denmark | RCT | Cost-utility | Societal perspective | 106 | 106 | 12 months | Adult patients admitted to the hospital with acute coronary syndrome | A model of shared care cardiac rehabilitation that included general practitioners and the municipality | Shared care between primary care and outpatient public health centers, with multidisciplinary teams | To assess the cost-utility of shared care cardiac rehabilitation versus hospital-only cardiac rehabilitation from a societal perspective | Outcomes: 1) quality-adjusted life years; Costs: 1) intervention cost/formal and informal staff time; 2) primary and secondary care; 3) productivity loss |
| Camacho et al. (2018) | United Kingdom | Cluster RCT | Cost-utility | Health care payer | 191 | 196 | 24 months | Patients with depressive symptoms and a record of diabetes and/or coronary heart disease | Participants attending primary care physician practices allocated to the collaborative care group received up to eight face-to-face sessions of brief psychological therapy delivered by a case manager over 3 months | General practices with case managers co-located with multidisciplinary team | To assess the cost-effectiveness of collaborative care for people with depression in the context of multimorbidity | Outcomes: 1) depression severity; 2) quality adjusted life years; 3) health care utilization; Costs: 1) inpatient; 2) outpatient; 3) emergency; 4) primary/community care; 5) intervention costs; 6) Implementation and training costs |
| Everink et al. (2018) | The Netherlands | Cohort | Cost-utility | Societal perspective | 113 | 49 | 9 months | Community-dwelling older patients who were admitted to a geriatric rehabilitation facility | The integrated care pathway comprised of cross-organizational agreements on coordination and continuity of care for older patients who transfer between the hospital, the geriatric rehabilitation facility and primary aftercare in the home context | Coordination between the hospital, the geriatric rehabilitation and primary care and home care | To determine the cost-effectiveness of receiving usual care compared to receiving care in the integrated care pathway | Outcomes: 1) dependence in activities of daily living; 2) quality adjusted life years; Cost: 1) intervention costs; 2) implementation costs; 3) primary, home care, long-term care, acute care and allied professionals; 4) patient out-of pocket expenses; 5) informal caregiving |
| Wong et al. (2018) | China | RCT | Cost-utility | Health care payer | 43 | 41 | 24 months | End-stage heart failure patients referred to in-hospital palliative care services | Patients received a transitional homebased palliative end-stage heart failure program delivered by nurse case managers who were trained specialist palliative care home care nurses with experience in heart failure management | Transitional care between hospital to home care delivered by case manager and multidisciplinary home care team | To evaluate the cost-effectiveness of a transitional home-based palliative care program | Outcomes: 1) quality adjusted life years; Costs: 1) acute, home and emergency care; 2) intervention cost; 3) training cost |
| Uittenbroek et al. (2018) | The Netherlands | RCT | Cost-utility | Societal perspective | 747 | 709 | 12 months | Older adults, aged 75 and over with primary care providers | A primary care physician-led Elderly Care Team was assembled for each participating practice, which also consisted of an elderly care physician, a community nurse, and a social worker | General practitioner-led elderly multidisciplinary care team in primary care with case manager | To assess the cost-effectiveness of integrated geriatric care team in primary care | Outcomes: 1) quality adjusted life years; 2) number of days older adult was able to age in place (i.e. no nursing home stays); Costs: 1) primary, acute, medication and paramedical care; 3) social and home care; 4) informal caregiving |
| Tsiachristas et al. (2015) | The Netherlands | Cohort | Cost-utility | Societal perspective | 1034 | 1034 | 24 months | patients diagnosed with or at risk of cardiovascular disease and chronic obstructive pulmonary disorder | Programs focused on improving the collaboration between different disciplines of health care professionals and redesigning the care giving process toward proactive, patient-centered care. | Disease management programs implemented through collaborations between general practices and hospitals, primary care practices (including physiotherapists and dieticians), or primary and community settings | To evaluate the cost-effectiveness of disease management programs for patients diagnosed with or at risk of cardiovascular disease and chronic obstructive pulmonary disorder | Outcomes: 1) quality adjusted life years; 2) level of physical activity; 3) proportion of smokers; Costs: 1) health care utilization costs; 2) travel costs; 3) productivity loss; 4) development costs; 5) implementation costs |
Table 2
Checklist assessing the quality of economic evaluations.
| Category | Item Description | Zulman et al. (2017) | Weisner et al. (2001) | Weeks et al. (2009) | Weaver et al. (2009) | Van Orden et al. (2009) | Olsson et al. (2009) | Leeuwen et al. (2015) | Lanzeta et al. (2016) | Goorden et al. (2013) | Boland et al. (2015) | Donohue et al. (2014) | Cohen et al. (2012) | Wise et al. (2006) | McCall et al. (2010) | Simon et al. (2001) | Hebert et al. (2008) | Vroomen et al. (2012) | Salmon et al. (2012) | Looman et al. (2016) | Celano et al. (2016) | Markle-Reid et al. (2010) | Pozzilli et al. (2002) | Tzeng et al. (2007) | Bergmann et al. (2017) | Koch et al. (2017) | Rosenheck et al. (2016) | Sahlen et al. (2016) | Blom et al. (2016) | Pimperl et al. (2017) | Schellenberg et al. (2004) | Bird et al. (2012) | Goltz et al. (2013) | Steuten et al. (2007) | Wiley-Exley et al. (2009) | Karow et al. (2012) | Renaud et al. (2009) | Tanajewski et al. (2015) | Lambeek et al. (2010) | Bertelsen et al. (2017) | Camacho et al. (2018) | Everink et al. (2018) | Kam et al. (2018) | Ulttenbroek et al. (2018) | Tsiachristas et al. (2015) | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study design | 1. Design was experimental (e.g. RCT or cluster-RCT) or quasi experimental design (e.g. used propensity score matching, pretest-posttest design)? | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | 75 |
| 2. Random allocation into intervention and control groups | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | 57 | |
| 3. The study population consist of an intervention and control group | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | Y | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 91 | |
| 4. Relevant baseline characteristics are comparable | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | NA | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 72 | |
| 5. The interventions or strategies being compared are described | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 98 | |
| 6. Included more than just baseline and follow up period | ✓ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | 61 | |
| 7. Clear description of inclusion and exclusion | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 86 | |
| 8. Clear description of drop-outs | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 70 | |
| Intervention setting | 9. Stated relevant aspects of the system(s) in which intervention takes place | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | 84 |
| 10. Co-interventions or contamination are avoided | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | 32 | |
| Measurement of costs & outcomes | 11. Describe the perspective of the study and relate this to the outcomes and costs being evaluated. | ○ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 75 |
| 12. Described which outcomes were used as the measure(s) of benefit in the evaluation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 | |
| 13. Inclusion of development and implementation cost | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | 34 | |
| 14. Inclusion of cost & utilization from across all relevant health and social sectors | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | 66 | |
| 15. Inclusion of direct non-medical and indirect costs | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | 39 | |
| 16. Justification for omitting costs categories | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ✓ | N/A | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ✓ | NA | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | NA | ○ | ✓ | ○ | ○ | NA | ○ | ○ | ✓ | ○ | ○ | NA | ○ | ✓ | ✓ | ○ | NA | 29 | |
| 17. The sources of resource utilization and cost are described | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | 91 | |
| 18. The resource utilization and costs are reported separately | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | 75 | |
| 19. Reports the (adjusted) dates of estimated resource quantities and unit costs | ○ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Y | Y | Y | Y | Y | 73 | |
| 20. Discounting of outcomes and costs performed | ○ | NA | ○ | NA | ○ | ○ | Y | NA | ○ | ○ | NA | NA | NA | ○ | ○ | ○ | Y | NA | NA | NA | NA | NA | NA | ○ | ○ | ○ | NA | NA | ○ | ○ | ○ | ○ | Y | NA | NA | Y | NA | N/A | NA | ○ | NA | NA | NA | ○ | 18 | |
| Statistical analysis | 21. Data analysis is performed according intention-to-treat principle | ✓ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | 39 |
| 22. Dealt adequately with missing observations | ✓ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | 59 | |
| 23. Appropriate statistical methods for analysing skewed data | ○ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 68 | |
| 24. Report the values, ranges, references, and if used, probability distributions for all parameters. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 91 | |
| 25. Analysed cost-effectiveness using the incremental cost- effectiveness ratio (ICER) method | ○ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 55 | |
| 26. Analysed cost-effectiveness using the incremental net- monetary or health benefit (INB) regression method | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 7 | |
| 27. Performed sub group analysis to examine heterogeneity of results | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ○ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | 48 | |
| 28. Analysed the uncertainty in the estimates of the costs and effects | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 64 | |
| Presentation of data | 29. A decision criteria is applied to determine whether to reject or accept intervention (e.g. willingness-to-pay vs. cost effectiveness threshold) | ○ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ○ | ✓ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ○ | ✓ | ○ | ✓ | ○ | ○ | ○ | ○ | ✓ | ✓ | ✓ | ○ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ○ | 43 |
| 30. The study discusses the generalizability of the results to other context and/or patient groups | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 98 |
[i] Legend: yes ✓, no ○.
