
Figure 1
Map of Central Coast (red dashed circle), within New South Wales Australia (A), within the Hunter New England Central Coast Primary Health Network jurisdiction (B, grey shaded area) and the Central Coast Local Health District (C, grey shaded area).
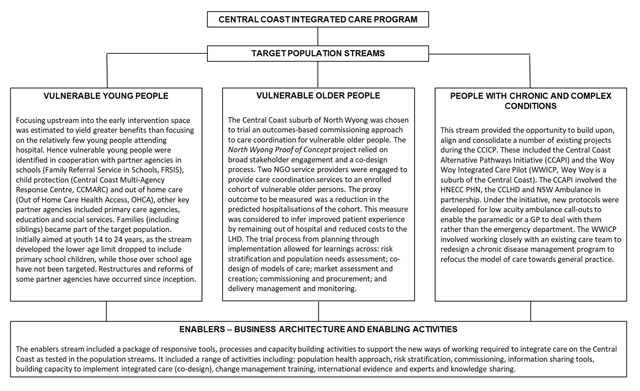
Figure 2
Central Coast Integrated Care Program Overview.
Table 1
Program stream project characteristics.
| Vulnerable Youth | Vulnerable Aged | Complex & Chronic Care | ||||
|---|---|---|---|---|---|---|
| FRS in Schools | CCMARC | OHCHA | NWPOC | CCAPI | WWICCP | |
| Full name | Family Referral Service in Schools | Central Coast Multi-Agency Response Centre | Out of Home Care Health Access | North Wyong Proof of Concept | Central Coast Alternate Pathways Initiative | Woy Woy Integrated Care Coordination Pilot |
| General description | An opportunity to develop Communities of Care around vulnerable families by creating an early intervention program, working upstream to impact health and social vulnerabilities. | The first NSW co-located multi-agency child protection information exchange and triage service. | Integrated multi-agency responses to assessment and management of the health needs of children and young people in out of home care | North Wyong Care coordination trial, uses NGO employed care coordination of vulnerable older person cohort, under novel outcomes based commissioning contracts, wherein reduction in unplanned hospital bed days are the target outcomes. Service is free to clients, with providers paid on outcomes. | NSW Ambulance Paramedics trained to implement low acuity protocols to manage alternate pathway referrals for appropriate patients. | Testing transition from the Chronic Disease Management Program (CDMP) to a model focused on General Practice |
| Objectives | To work with families, reduce their barriers to engaging with services and to prioritise actions that will support young people to engage with learning. | To define health’s role in interagency responses to child protection. Increase effective information exchange between health and Department of Family and Community Services (FACS). Support multiagency quality initiatives that enable early intervention responses for children at risk of significant harm (ROSH) | To better understand the pathways into out of home care, and identify opportunities for better-integrated service delivery To provide a better, integrated approach to health assessment and treatment of young people in this region. | To improve care coordination for enrolled cohort and reduce unplanned hospital bed days. To trial care coordination delivered by non-health providers To trial outcomes based funding model To keep older people healthy and at home for longer | To reduce unnecessary hospital transports of low acuity patients and to reduce ambulance turnaround time at hospitals. | To transition and improve care coordination for complex clients within the community |
| Date | October 2016–present | November 2015–to present | January–December 2016 | January 2017–present, Commissioning cycle initiated July 2014 (needs assessment) | Proof-of-concept–January 2014. Paramedic training December 2015, June 2016 | April 2016 to March 2017 |
| Size | 3 school learning communities–10,790–5 high schools, 13 primary schools, 2 providers | Central Coast, NSW population | >1000 young people (30–50 new to care each month) | 440 patients, 4 general practices, 2 NGO providers | 108 NSW Ambulance paramedics Central Coast NSW population | 109 patients, 2 care coordinators, 8 general practices, 39 GPs |
| Target Population | Students and their families where there is an identified risk of disengagement from learning and school attendance. | Children and young people at risk of significant harm who live on the Central Coast, NSW | Children and young people in out of home care are a high-risk group for health and social care vulnerabilities. 30% Indigenous and 117 in kinship placements | North East Wyong region. People identified as having high health need, low socioeconomic status and ageing–likely to benefit from care coordination. | Patients assessed by qualified paramedics as suitable for alternative referral options do not require transport to the ED via ambulance. | Woy Woy, NSW chronic care population |
| Single point of referral | Yes (schools) | Yes | Yes | Not applicable, cohort identified by Central Coast LHD and referred to providers | Triage via telephone contact with the ambulance service | Identified through Central Coast LHD Connecting Care Program |
| Risk Stratification | Yes | Yes–ROSH screening tool used by FACS | Yes | Yes | Yes | Yes |
| Inclusion criteria | Primary and high school students and their families Geographically defined | Vulnerable families in the Central Coast region | Young people (0–18 years) in out of home care in the Central Coast region | Aged 65 or over 1 unplanned admission over the last year 2+ chronic conditions Geographically defined | NSW Ambulance patient transportations of triage categories 4/5 | Identified through Central Coast LHD Connecting Care Program |
| Partners | Family Referral Service, Central Coast LHD, Department of Education (DoE), Local School Principals, HNECC PHN, FACS | CCLHD, FACS, DoE, The Benevolent Society, Family Referral Service | Central Coast LHD, HNECC PHN, FACS | HNECC PHN ADSSI Home Living Kincare Health Services | HNECC PHN Central Coast LHD NSW Ambulance | Central Coast LHD GPs |
| Community & Primary Care focus | Yes | Yes | Yes | Yes | Yes | Yes |
| Co-design | Yes | Yes | Yes, with respect to establishing three working groups for priority action. | Yes | Yes | No |
| Care-coordination | Yes | Limited to coordination of referrals | Yes | Yes | Limited to coordination of alternative referrals. | Yes |
| Key facilitators | Family Engagement Workers, local school Principals, finding alignments with partner agencies goals and frameworks to progress work (aligned values) | Colocation of multiagency staff with formal structured collaboration meetings for information exchange and quality improvement | Collaboration and strong leadership. Clear common goals defined by FACs and Health Policy objectives | Evidence-informed planning, Outcomes Based Commissioning cycle, strong leadership, NGO market appetite to undertake work | Cooperative patients, usual care providers or available GP practices | Early implementer of the state-wide redesign on CDMP |
| Key challenges | Adequate needs assessment of families and their cooperation, support from local school Principals, restricted ability to fully partner with HNECCPHN, identification of systemic gaps in services (e.g. under 12s mental health, housing and accommodation, services to support behavioural issues for students) | Rigorous quality improvement framework, consistent approach of adoption and monitoring of changes Unclear goals from outset | Formal and informal partnership agreements, framework design with partners State-based review (Their Futures Matter review) and reform overrode the activities, limiting ability to go forward with planned changes at the time. | New ways of working for NSW Health: contracts, procurement procedures (different to commissioning), time pressures, privacy and ethics concerns, sharing the risk between Central Coast LHD and providers, contracts based 100% on outcomes, restricted ability to fully partner with HNECC PHN | New way of working for NSW Ambulance paramedics, collaboration with patients, usual care providers or available GP practice, restricted ability to fully partner with HNECCPHN | Implementing new model of care within existing program and workforce with entrenched ways of working. |
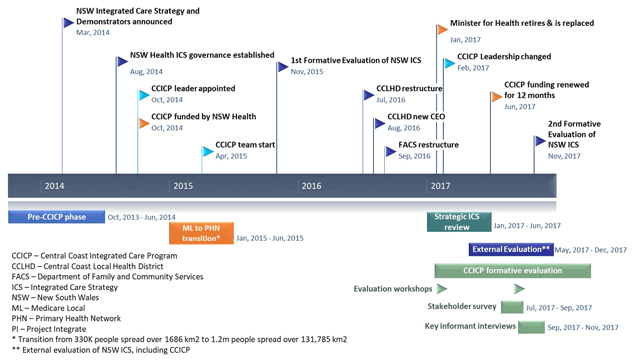
Figure 3
Key events and changes over the CCICP planning and implementation period.
