| History and nature in the health system |
|
| Provision of asthma care – guidelines |
|
Table 1
Interviewees’ characteristics, according to awareness narrative.
| Pseudonym | Age | Educational level | Household members | Diagnosis | Asthma in the family |
|---|---|---|---|---|---|
| Narrative of minimization | |||||
| Ana | 61 | Elementary | Husband | Adulthood (at 60) | Yes (son and brother) |
| Graça | 45 | Elementary | Husband | Adulthood (at 39) | Yes (mother, husband) |
| Maria | 58 | Elementary | Husband | Adulthood (at 46) | No |
| Cristina | 34 | High | Husband and son | Adulthood (at 27) | Yes (sister) |
| Filipa | 59 | High | Husband | Adulthood (at 56) | Yes (husband) |
| Sebastião | 54 | Elementary | Wife | Adulthood (at 51) | Yes (mother, daughter) |
| João | 45 | Elementary | Wife | Adulthood (at 42) | No |
| Elsa | 46 | Secondary | Husband and son | Adulthood (at 41) | Yes (father and son) |
| Joana | 53 | Elementary | Husband | Adulthood (at 39) | No |
| Júlia | 21 | Secondary | Husband and son | Adulthood (at 19) | Yes (father) |
| Manuela | 65 | Elementary | Son | Adulthood (at 61) | Yes (mother and sister) |
| Ema | 62 | Elementary | Husband | Adulthood (at 57) | No |
| Narrative of disruption | |||||
| Laura | 68 | Elementary | Mother and husband | Adulthood (at 58) | No |
| Olinda | 65 | Elementary | Alone | Childhood | Yes (grandmother) |
| Rita | 52 | Elementary | Husband | Adulthood (at 32) | Yes (grandmother) |
| Helena | 66 | Elementary | Husband | Childhood | Yes (aunt) |
| Anabela | 31 | High | Husband and son | Childhood | Yes (sister recently diagnosed) |
| António | 22 | Secondary | Parents | Childhood | Yes (sister) |
| Idalina | 70 | Elementary | Alone | Adulthood (at 65) | Yes (grandmother) |
| Isabel | 30 | Secondary | Boyfriend | Childhood | Yes (son) |
Table 2
Representative quotes of the main themes – narrative of minimization.
| 1.1 Dealing with an asthma diagnosis (low impact; family condition; importance of the diagnostic consultation) | |
| [1.1a] | Elsa: “I was not surprised (when diagnosed with asthma) … My son has asthma since a child, my father also had it. It is in the family.” |
| [1.1b] | Júlia: “I didn’t worry (about asthma diagnosis). Because I was always feeling bad (…) and then I saw the problem solved.” |
| [1.1c] | Filipa: “I already knew that he [family doctor] was also asthmatic (…) and he said: “don’t be afraid, because when I was in college I already had asthma and I am still around.” To have heard this was reassuring.” |
| [1.1d] | Filipa: “I already knew that he [family doctor] was also asthmatic (…) he said to me: ‘don’t be afraid, because when I was in college I already had asthma and I am still around.’” |
| 1.2 Self-management skills (avoidance of major crises; control of symptoms by SOS medication) | |
| [1.2a] | Elsa: “I know that if I am in some bad environment, with smells, of course I will be attacked. But I know what to do (SOS medication).” |
| [1.2b] | Júlia: “It is more at night that I have more asthma, (…) and when I am attacked, I take my SOS pump and I immediately get better.” |
| [1.2c] | Maria: “My doctor prescribed me a medication, and I started doing it. But then, my mother-in-law, who suffers from bronchitis and used to take the same medication, told me: ‘don’t take that, then you get used to it and can’t walk anymore’: So I stopped. But then I went to a pharmacy and he (pharmacist) told me to do it, and I did; but later another pharmacist, in another pharmacy, told me to leave it. And now I don’t take it.” |
| 1.3 Health literacy mediators (dense network) | |
| 1.3.1 Family and friends (close family members; emotional and pragmatic support) | |
| [1.3.1a] | Filipa: “The medication was the same as my husband, and sometimes we shared. (…) When we go on vacations, his last question before leaving home (…) is if I have brought the pumps.” |
| [1.3.1b] | Manuela: “I went there 42 because they (siblings) told me that he (a doctor) was great! (…) He did an exam that nobody here in Portugal told me to do.” |
| [1.3.1c] | Graça: “If I’m having a crisis, (…) my daughters (…) know exactly what to do: one of them goes right away search for my inhaler/pump. They know that I always carry one in my bag or in my pocket.” |
| [1.3.1d] | João: “If I am a little ‘attacked’ my wife immediately says: “you will have a crisis!”. (…) She always ensures that I take it (medication).” |
| [1.3.1e] | João: “Once, my friends and I went to ride in karts. The building, completely indoor, was full of smoke from the karts. I felt bad, completely short of breath (…) My friends came with me outside, to breathe.” |
| [1.3.1f] | Filipa: “I have friends calling me, saying: “So, did you go to that doctor?” (…) They worry.” |
| 1.3.2 Health professionals (PCP; instrumental support) | |
| [1.3.2a] | Sebastião: “I go there (primary care center) often (…) usually I have two consultations a year.” |
| [1.3.2b] | Ema: “I don’t like to go to different doctors, because they all say different things.” |
| [1.3.2c] | Cristina: “My doctor is great. She really worries about us; we can feel it is genuine. She has a very close relationship with me, my son… I already told my sister [also asthmatic] she should move to this primary care center and be patient of my doctor.” |
| 1.3.3 Media (not always reliable) | |
| [1.3.3a] | Cristina: “I also go to the internet (…), but I think that sometimes it is bad, because they give opinions, but they are not experts.” |
| [1.3.3b] | Graça: “If people say things differently from the doctors, it is wrong, I don’t trust it. Not everybody can write about this (asthma); it must be a doctor.” |
Table 3
Representative quotes of the main themes – narrative of disruption.
| 2.1 Dealing with an asthma diagnosis (disruptive impact; feelings of stigma; to hide asthma) | |
| [2.1a] | Isabel: “Asthma did change my life and the way I see life… At least when I’m attacked.” |
| [2.1b] | António: “When practicing swing, soccer, running, and other sports, it (asthma) does not allow us to be as resistant as other persons.” |
| [2.1c] | Rita: “I want to do things, but I’m not able to do so (…) and people sometimes do not understand. Sometimes I feel people are saying: ‘she is faking it.’ (…) It is very upsetting.” |
| [2.1d] | Idalina: “It’s hard! People stay disgusted, with a weird face (when seeing an asthma attack).” |
| [2.1e] | Isabel: “He (participant’s son, also asthmatic) does not take it (the pump) to school (…) (because) he does not like to say he has asthma, since very little.” |
| [2.1f] | Laura: “Causes? I think it was from tobacco (her husband smokes). And I don’t smoke! Do you believe? It is so frustrating.” |
| 2.2 Self-management skills (reactive approach; alternative solutions; feelings of personal guilt) | |
| [2.2a] | Rita: “I feel anxious and in panic [when having a crisis]. (…) Oh my God, if I use the pump and it does not work, I panic, and I just pray to pass.” |
| [2.2b] | Anabela: “Yes, I have searched for other options, such as, acupuncture. And it was good, I felt some benefits.” |
| [2.2c] | Helena: “I have the pump. My doctor told me to use it every day, but I only do it once in a while. Because I like to read patient information leaflet, and if everybody read that, people would not take medications. Because what it is written there, it really might happen.” |
| [2.2d] | Anabela: “I don’t know, maybe I’ve been lazy…The pediatrician of my son told me my medication (for asthma) was totally outdated and I should start a new treatment. I really have to convince myself and have a medical consultation about this.” |
| [2.2e] | Isabel: “People say that the beach is bad for the lungs, and when I’m attacked I don’t go to the beach. I’m afraid.” |
| [2.2f] | António: “The last couple of years, (…) I take medication more regularly (…) and I go to the emergency rooms quite often (…) It already happened go to the hospital twice a month.” |
| [2.2g] | Anabela: “Usually, when I’m attacked I take Ventilan in SOS, and it is effective. However, since last month I have been taking Ventilan 3 to 4 times a day, and it is not working, I still have the symptoms.” |
| 2.3 Health literacy mediators (restricted network) | |
| 2.3.1 Health professionals (PCP; communication issues) | |
| [2.3.1a] | António: “Sometimes I need to know something quite specific – for instance why my crisis are more regular – and I just ask to the doctor. But actually, nowadays, we don’t need to come here to know something, I go online or to the medical leaflets.” |
| [2.3.1b] | Rita: “I’m from the opinion that explaining things helps a lot. For instance, last month I went to do some exams at the hospital, and during the exam I asked a lot of things to the nurse. She was very nice, and answered me. But her colleague told me: ‘you don’t need to know! It’s the doctor that must know everything!’. But that’s wrong. We are the patients, we should know.” |
| [2.3.1c] | Ema: “I think the hardest part is the language, I think it is. Because doctors speak for each other’s, not for the patient. Once I was hospitalized, and a group of doctors just came to my room, they spoke for each other’s, and I didn’t understand a thing.” |
| 2.3.2 Media (Internet; not reliable) | |
| [2.3.2a] | Anabela: “Once I was having cramps, so I went online to search something about what was causing me that, and read that people with asthma tend to have more cramps than usual. But I don’t know if it is true, I only find that in one website. No where else.” |
| 2.3.3 Family and friends (lack of support) | |
| [2.3.3a] | Helena: “My husband usually tells me: ‘Calm down’! (…) When he tells me that, I got much worse. Oh my God, I can’t hear that. (…) I know that my husband just wants to help me, but I can’t avoid this.” |
| [2.3.3b] | Idalina: “Nobody helps or anything. I am the one who have to help the others.” |
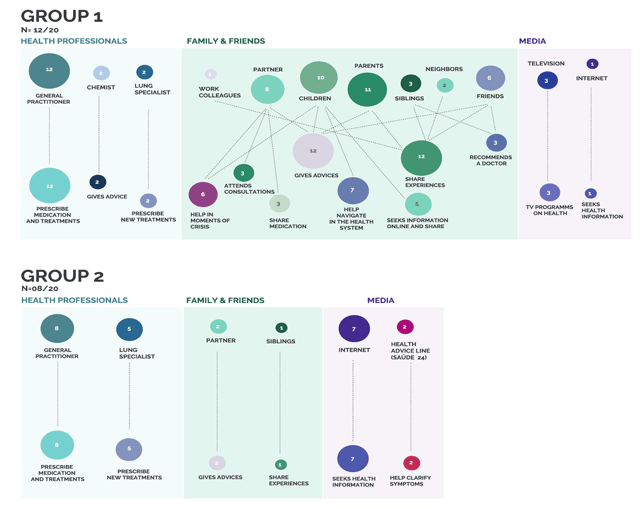
Figure 1
Map of health literacy mediators and practices according to awareness narratives.
1 Circles are the frequency that each mediator was mentioned and lines are the association to different health literacy practices.
