Table 1
Elements key to meso level organisations working together [36].
| Element | Interventions shown to be effective |
|---|---|
| 1. Joint planning | Working together agreements to support joint strategic focus for future work between stakeholders focusing on the continuum of care. |
| 2. Integrated information communication technology | Systems designed to support shared clinical exchange, such as, Shared Electronic Health Record, and tools to support systems integration linking clinical processes, outcomes and financial measures. |
| 3. Change management | Bilateral support for an agreed change process which is managed locally, and has demonstrated leadership, vision and commitment. |
| 4. Shared clinical priorities | Target areas for redesign are agreed and multi-disciplinary pathways across the continuum supported. |
| 5. Incentives | Funding mechanisms are provided to strengthen care co-ordination and there are incentives to innovative. |
| 6. Population focus | Geographical population health focus. |
| 7. Measurement – using data as quality improvement tool | Shared data is used for planning, measurement of utilisation focusing on quality improvement and redesign and a collaborative approach to measuring performance provides transparency across organisational boundaries. |
| 8. Continuing professional development supporting the value of joint working | Inter-professional and inter-organisational learning opportunities provide training to support new ways of working and align cultures. |
| 9. Patient/community engagement | Involve patients and communities in developing the outcome they want. |
| 10. Innovation | Resources are available and innovative models of care are supported. |
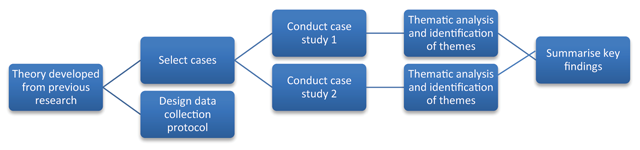
Figure 1
Case study methodology.
Table 2
Semi-structured questions asked of each element identified in systematic review [36].
| Key research question for each element |
|---|
|
Table 3
Thematic framework and subthemes identified.
| Major themes title | Focus | Q1: How is the element supported, or not, in the current practice? | Q2: How will/could this element be used in the future? | a. What are key enablers? | b. What are key barriers? | |
|---|---|---|---|---|---|---|
| Supports (✓) | Does not support (×) | |||||
| 1. Organisational versus system focus | Structures support an organisational not system focus | × No system accountability × Funding method prescriptive × Planning not strategic × No team across the continuum × Lack of innovation and focus on the process of change | ✓ Accountability for outcomes, joint key performance indicators (KPIs) ✓ Funding reform to allow flexibility and change ✓ Vision for a health system and long term strategy agreed ✓ Focus on care for the population and care across the continuum based on needs | + Patient-focused care + Change supported, measured and evidence provided | – Short term strategy & policy cycles – Drivers - financial, political, and cultural - not aligned – No joint accountability for population health planning, performance or outcomes | |
| Access to quality and useful data across the system is essential | × Poor data quality × Data rich, information poor | ✓ One central national repository for all data ✓ Needs to be broken down into geographical areas for use locally ✓ Data governance agreed | + Sharing data across the continuum is key | – Lack of access to quality data – Legal issues – who owns the data, political risk, consent and privacy – Cost | ||
| 2. Leadership and culture | Leadership skills to develop a ‘system’ approach is essential | ✓ Goodwill at executive level ✓ See the need for change | × Lack of leadership, trust and commitment | ✓ Boards have to operate in honest and transparent environment and value working in partnership ✓ Board’s commitment demonstrated with joint MOU to support structural alignment | + Board agreement on common purpose + Determine priorities + Dedicated resources to facilitate under CEO direction | – Lack of leadership and commitment to change – No central co-ordination at government level |
| Clinician engagement across the continuum is key | ✓ Roles working across the continuum have brought change | × Lacking at senior level × Inadequate resources to support engagement | ✓ Clinician leaders identified and supported to lead the way ✓ Use of boundary spanners | + Clinician leadership - joint clinical governance board to agree protocols across the continuum + Facilitate communication, build goodwill | – Overcoming vested interests to keep things the way they are – Clinician leaders risk-adverse rather than allowed to be sensible risk takers | |
| Cultural barriers exist | × Risk-averse rather than risk-aware × Perceptions hospitals have the most to gain | ✓ Value working together, mutual respect and understanding articulated throughout the sectors | + Build relationships and professional respect | – Decades of bureaucratic control to overcome – ‘Master/servant’ relationship – Lack of communication and collaboration across the system before decisions are made | ||
| Workforce capacity building is needed | × Seen as operational not strategic | ✓ Support interprofessional learning opportunities ✓ Need a driver tasked with this – boundary spanner | + Shared KPIs for outcomes + Requires strategic support + Requires strategic support | – How do we educate across the continuum? No KPIs for this | ||
| 3. Community (dis) engagement | Overcoming perceptions | × Not using the community × Preconceived ideas | ✓ Need to bring the community on the journey | + Agreed mandate for engagement across the system | – Perceptions hospital care is best – How do we educate across the continuum? No KPIs for this | |
| Requires greater priority | × Not a priority | ✓ Need a vision to keep people well, not focus on illness | + Policy directive + Requires designated resources | – Lack of focus on this at Board and Executive level | ||
