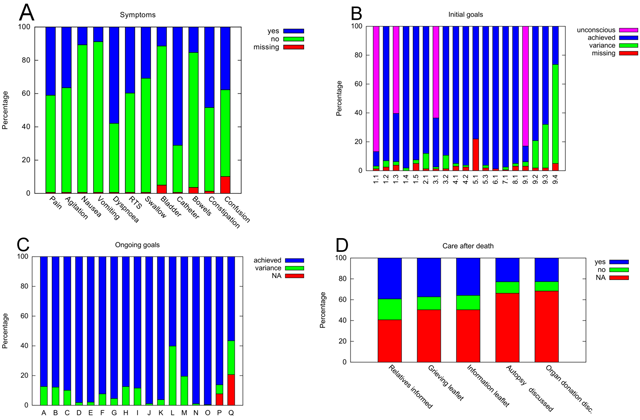
Figure 1
Results from auditing of 159 cases. (A) Initial assessment of symptoms (RTS, respiratory tract secretions). (B) Initial goals according to the LCP manual [8]. The areas comprise communication (goals 1.1–1.5), facilities (goal 2.1), spirituality (goals 3.1 and 3.2), medication (goals 4.1 and 4.2), current interventions (goals 5.1 and 5.3), nutrition and hydration (goals 6.1 and 7.1), skin care (goal 8.1) and explanation of the plan of care (goals 9.1–9.4) as follows: goal 1.1, The patient is able to take a full and active part in communication; goal 1.2, The relative or carer is able to take a full and active part in communication; goal 1.3, The patient is aware that they are dying; goal 1.4, The relative or carer is aware that the patient is dying; goal 1.5, The clinical team have up to date contact information for the relative or carer; goal 2.1, The relative or carer has had a full explanation of the facilities available for them and a facilities leaflet has been given; goal 3.1, The patient is given the opportunity to discuss what is important to them at this time, e. g., their wishes, feelings, faith, beliefs, values; goal 3.2, The relative or carer is given the opportunity to discuss what is important to them at this time, e.g., their wishes, feelings, faith, beliefs, values; goal 4.1, The patient has medication prescribed on a pro re nata basis for all of the following five symptoms which may develop in the last hours or days of life: pain, agitation, respiratory tract secretions, nausea/vomiting, dyspnoea; goal 4.2, Equipment is available for the patient to support a continuous subcutaneous infusion of medication where required; goal 5.1, The patient’s need for current interventions has been reviewed by the multidisciplinary team; goal 5.3, Implantable cardioverter defibrillator is deactivated; goal 6.1, The need for clinically assisted (artificial) nutrition is reviewed by the multidisciplinary team; goal 7.1, The need for clinically assisted (artificial) hydration is reviewed by the multidisciplinary team; goal 8.1, The patient’s skin integrity is assessed; goal 9.1, A full explanation of the current plan of care (LCP) is given to the patient; goal 9.2, A full explanation of the current plan of care (LCP) is given to the relative or carer; goal 9.3, The LCP coping with dying leaflet or equivalent is given to the relative or carer; goal 9.4, The patient’s primary health care team/GP practice is notified that the patient is dying. NB: goal 5.2 (The patient has a Do Not Attempt Cardiopulmonary Resuscitation Order in place) was a requirement for all patients on the SPCU and therefore not recorded. (C) Achieved goals and variances during ongoing assessments (4 hours per visit). The letters indicate the goals according to the LCP manual [8]. Goal A, The patient does not have pain; goal B, The patient is not agitated; goal C, The patient does not have respiratory tract secretions; goal D, The patient does not have nausea; goal E, The patient is not vomiting; goal F, The patient is not breathless; goal G, The patient does not have urinary problems; goal H, The patient does not have bowel problems; goal I, The patient does not have other symptoms; goal J, The patient’s comfort and safety regarding the administration of medication is maintained; goal K, The patient receives fluids to support their individual needs; goal L, The patient’s mouth is moist and clean; goal M, The patient’s skin integrity is maintained; goal N, The patient’s personal hygiene needs are met; goal O, The patient receives their care in a physical environment adjusted to support their individual needs; goal P, The patient’s psychological well-being is maintained; goal Q, The well-being of the relative or carer attending the patient is maintained. NA, not applicable. (D) Care after death (disc., discussed). NB: Some items of this section, such as the time of death, are recorded in other sections of the electronic hospital information system and thus not included here.
