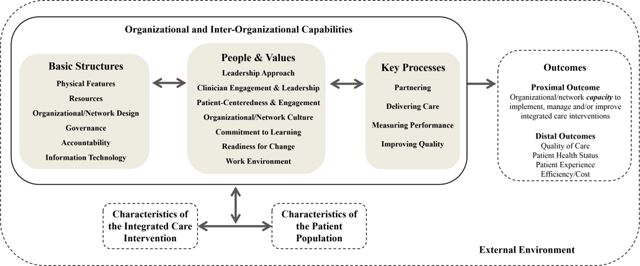
Figure 1
The Context and Capabilities for Integrating Care (CCIC) Framework [15].
Table 1
Context and Capabilities for Integrating Care (CCIC) Framework: Definitions and Examples [15].
| Concept | Definition | Examples |
|---|---|---|
| Basic Structures | ||
| Physical Features | Structural and geographic characteristics of the organization/practice and network | organization/practice size and age, urban or rural location, facilities, geographic proximity of network members |
| Resources | Availability of tangible and intangible assets for ongoing operations at the organization/practice and for network activities | staffing, funding, knowledge, time, project management support, administrative support, brand/reputation |
| Governance | How the board or steering committee is organized and its activities to direct, manage and monitor the affairs of the organization/practice and network | board/committee composition, types of sub-committees, frequency of meetings, types of decisions made (e.g., extent of centralized planning and standardization) |
| Accountability | The mechanisms in place to ensure that people and organizations meet formal expectations in the organization/practice and network | regulations enforced by an authority (e.g., government), formal agreements between organizations (e.g., data sharing), organizational mandates, professional scope of practice |
| Information Technology | The availability and ease of use of technology-based communication and information storage mechanisms in the organization/practice and across the network | shared electronic medical records, email communication, video conferencing, data access and mining, tele-healthcare |
| Organizational/Network Design | The arrangement of units and roles and how they interact to accomplish tasks in the organization/practice and network | organizational chart (hierarchy), types of departments/programs, job descriptions, communication and decision-making channels (e.g., are they centralized or decentralized? formal or informal?) |
| People and Values | ||
| Leadership Approach | The methods and behaviours used by formal leaders in the organization/practice or network (i.e., individual leaders, leadership teams, or lead organizations) | personal vision for the organization/practice or network, strategies used to empower staff, leadership style and competencies |
| Clinician Engagement & Leadership | The formal and informal roles held by clinicians in the organization/practice and network, particularly physicians, that enable them to buy-in to and steer change, and influence others | active involvement of clinicians in planning, leading or supporting new initiatives (e.g., clinical champions or directors, networks led by primary care practices) |
| Organizational/Network Culture* | Widely shared values and habits in the organization/practice or network | perceptions regarding what is important and what is appropriate behavior |
| Focus on Patient-Centeredness & Engagement | Commitment to placing patients at the center of clinical, organizational and network decision-making | collection and use of patient feedback, consideration for patient needs and preferences, patient input and representation on committees as a standard practice, patient involvement in co-designing services |
| Commitment to Learning | The existence of a set of values and practices that support ongoing development of new knowledge and insights within the organization/practice and network | experimentation encouraged and rewarded, forums for meeting with and learning from other organizations and external experts, time and resources to reflect on past performance |
| Work Environment | How employees perceive and experience their job and their workplace in the organization/practice and network | opportunity for input, job satisfaction, burnout |
| Readiness for Change | The extent to which organizations and individuals are willing and able to implement change in the organization/practice and network | attitudes toward change and toward new or innovative ideas, extent of fit between current vision/strategy and the change |
| Key Processes | ||
| Partnering | The development and management of formal and informal connections between different organizations/practices | sharing information, sharing staff, engaging in collaborative problem-solving, building a common understanding and vision, exchanging knowledge, implementing referral and discharge/transfer agreements |
| Delivering Care | The methods used by providers in caring for patients in the organization/practice and network | inter-professional teamwork and joint care planning, use of standardized decision support tools, medical model vs. holistic model of care, shared patient-provider decision-making |
| Measuring Performance | The systematic collection of data about how well the organization/practice and network is meeting its goals | shared performance measurement framework, regular measurement and reporting, data access and mining |
| Improving Quality | The use of practices and processes that continuously enhance patient care in the organization/practice and network | providing quality improvement (QI) training to staff, systematic use of QI methods (e.g., process mapping, control charts), application of best practices |
[i] *Capabilities such as Focus on Patient-Centeredness and Engagement, Commitment to Learning and Readiness for Change may manifest in the culture of the organization or network.
Table 2
Organizational Factors Measured by Selected Instruments/Items. ✓ denotes the main area covered by instrument, ⨯ denotes other areas directly covered by one or more items, ○ denotes areas indirectly addressed in the instrument.
| Selected Instruments | CCIC Factors (12/18) | Resources | Organizational/Network Design | Leadership Approach | Clinician Engagement & Leadership | Organizational/Network Culture | Commitment to Learning | Work Climate | Readiness for Change | Delivering Care (Teamwork) | Improving Quality | Partnering | Measuring Performance |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Team Climate Inventory [20] (14 items) | ⨯ | ⨯ | ⨯ | ✓ | |||||||||
| Organizational Culture Inventory [24] (12 items) | ○ | ○ | ✓ | ○ | ○ | ○ | ○ | ||||||
| Change Readiness Survey [21] – 3 scales only (15 items) | ✓ | ||||||||||||
| Survey of Organizational Attributes in Primary Care (SOAPC) [2223] – 3 scales only (14 items) | ⨯ | ⨯ | ○ | ✓ | ⨯ | ✓ | ⨯ | ||||||
| Measure of Network Integration [19] – 2 scales only (9 items) | ⨯ | ⨯ | ✓ | ⨯ | |||||||||
| Partnership Self-Assessment Tool (PSAT) [1826] – 6 scales only (38 items) | ⨯ | ⨯ | ○ | ○ | ✓ | ⨯ | |||||||
Table 3
An Example of the Use of Mixed Methods to Triangulate Data on Clinician Engagement and Leadership.
| Method | Content |
|---|---|
| Document and Website Review | 1. Clinician leadership of key committees and initiatives (particularly for quality and safety). |
| 2. Clinician involvement on the board. | |
| Possible sources of information include: organizational website, annual reports, strategic plans, policies and procedures, terms of reference, improvement plans, job descriptions, meeting minutes and evaluation reports. | |
| Survey Instrument | Participatory Decision-Making Scale of the Survey of Organizational Attributes for Primary Care (SOAPC) [2223] |
| 1. This is a very hierarchical organization: The decisions are made at the top, with little input from those doing the work. | |
| 2. This practice encourages staff input for making changes and improvements. | |
| 3. This practice encourages nursing and clinical staff input for making changes and improvements. | |
| Responses are measured on a 5-point Likert scale from “strongly disagree” to “strongly agree”. | |
| Interview Question Repository | How engaged and active are you and other clinical staff members in organizational issues? |
Prompts:
|
