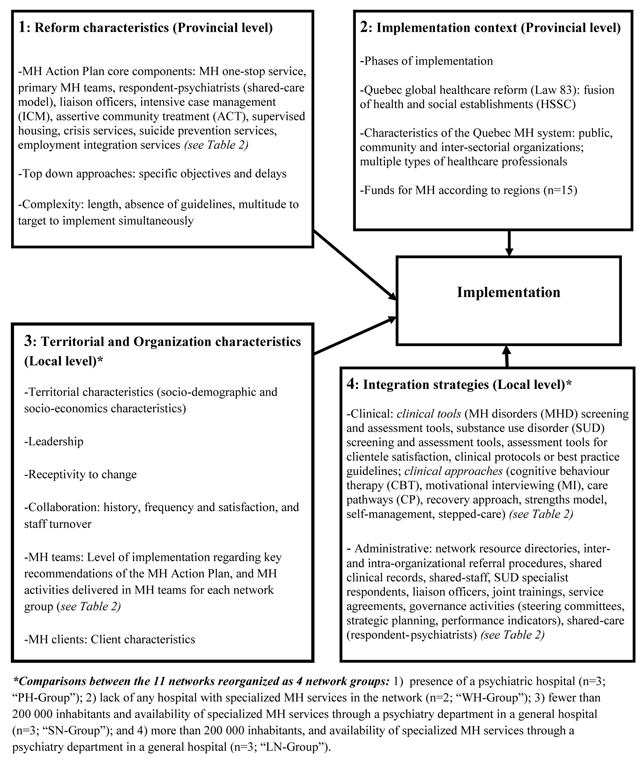
Figure 1
Conceptual framework.
Table 1
Socio-demographic Description of Professionals.
| Variables | Categories | Questionnaires completed by managers/Coordinators of MH* specialized services (N = 48) | Questionnaires completed by managers/Coordinators of MH primary care teams (N = 33) | Questionnaires completed by managers/Coordinators of HSSC (N = 9) | Questionnaires completed by Respondent- psychiatrists (N = 16) | Interviews (N = 102) | Total: 208 |
|---|---|---|---|---|---|---|---|
| Average age [Mean (SD)] | 45.7 | 42.2 | 48.6 | 49.1 | 50.7 | 47.26 | |
| Gender [n (%)] | Female | 30 | 25 | 5 | 6 | 69 | 135 |
| Male | 18 | 7 | 4 | 10 | 33 | 72 | |
| Current position [n (%)] | Psychiatrists | 0 | – | 0 | 16 | 7 | 23 |
| General practitioners (GPs) | 0 | – | 0 | – | 10 | 10 | |
| Psychosocial clinicians | 9 | 7 | 0 | – | 4 | 20 | |
| Regional managers | 0 | 0 | – | 4 | 4 | ||
| Directors | 0 | – | 3 | – | 35 | 38 | |
| Program administrators/Coordinators | 39 | 26 | 6 | – | 42 | 113 | |
| Years of experience [Mean (SD)] | In the current position | 7.4 | 5.6 | 5.9 | 2.9 | 7.9 | 5.9 |
| In psychiatry | – | – | – | 17.8 | – | 17.8 | |
| In health and social services | – | – | – | – | 23.1 | 23.1 | |
| In mental health (MH) | – | – | – | – | 19.4 | 19.4 | |
| With adult populations (MH) | – | – | – | – | 19.5 | 19.5 | |
| Organizations | Regional agencies | – | – | – | – | 10 | 10 |
| Psychiatric hospitals (PHs) | 23 | – | – | 4 | 14 | 41 | |
| General hospitals (GHs) | 25 | – | – | 3 | 9 | 37 | |
| Health and social service centres | 33 | 9 | 9 | 44 | 95 | ||
| Medical clinics | – | – | – | 7 | 7 | ||
| Community organizations | – | – | – | – | 18 | 18 | |
| Types of territories [n (%)] | With a PH | 23 | 15 | 3 | 4 | 37 | 82 |
| Without specialized MH services | – | 2 | 1 | 1 | 16 | 20 | |
| > 200 000 inhabitants, with a psychiatric department in a GH | 13 | 12 | 3 | 2 | 21 | 51 | |
| < 200 000 inhabitants, with a psychiatric department in a GH | 12 | 4 | 2 | 9 | 28 | 64 | |
[i] *MH: mental health.
Table 2
Synthesis of the Mental Health (MH) Reform – implementation targets.
| 1-Quebec MH Reform: Targets achieved | PH-Group (n = 3) | WH-Group (n = 2) | SN-Group (n = 3) | LN-Group (n = 3) | |
|---|---|---|---|---|---|
| MH one-stop service | |||||
| MH one-stop service in all networks with a population of 50,000 inhabitants or more | 3 (100%) | 1 (50%) | 1 (33%) | 3 (100%) | |
| Health and Social Service Centres (HSSC)-MH primary care teams (for adults) | |||||
| 20 multi-disciplinary MH clinicians/100,000 | 1 (33%) | 1 (50%) | 2 (67%) | 1 (33%) | |
| 2 general practitioners (GPs)/100,000 | 0 (0%) | 1 (50%) | 0 (0%) | 1 (33%) | |
| Access to evaluation: 7 days | 1 (33%) | 1 (50%) | 1 (33%) | 2 (67%) | |
| Access to treatment: 30 days | 0 (0%) | 1 (50%) | 0 (0%) | 2 (67%) | |
| Intensive case management (ICM) | |||||
| ICM in HSSC | 1 (33.3%) | 2 (100%) | 2 (67%) | 2 (67%) | |
| ICM offered by MH community organizations (but under the responsibility of the HSSC) | 3 (100%) | 0 (0%) | 0 (0%) | 3 (100%) | |
| Respondent-psychiatrists (shared-care model) | |||||
| 1 respondent-psychiatrist/50,000 (3 hours/service: to HSSC-MH Primary care teams and GPs) | 3 (100%) | 1 (50%) | 3 (100%) | 2 (67%) | |
| Specialized MH services | |||||
| Access to evaluation in specialized MH services: 14 days | 0 (0%) | N.A. | 0 (0%) | 2 (67%) | |
| Access to treatment in specialized MS services: 2 months | 0 (0%) | N.A | 0 (0%) | 2 (67%) | |
| Assertive community treatment programs (ACT) | 1 (33%) | N.A | 1 (33%) | 1 (33%) | |
| 2- Main strategies to consolidate primary care or network integration, based on the literature [58] | |||||
| 2.1 Clinical Strategies | |||||
| Evaluation/clinical tools: Establish clinical standardization and rationalization to promote best practices.[14] |
| Mainly implemented in the PH Group | |||
| Clinical Approaches (Best practices) | Cognitive behaviour therapy (CBT): Psychotherapy aiming to change thinking and behaviour. Effective for most MHDs, including SUDs [59]. | Mainly used in the WH-Group | |||
| Motivational interviewing (MI): Brief intervention aiming to engage motivation to change behaviour. Mainly effective for SUDs [60]. | Mainly used in the WH-Group | ||||
| Care pathways: Systematic interventions planned for integrating care between different organizational units, or between providers, for a well-defined group of clients and treatment periods. Originally established in physical health for acute care, for which it has been proven effective, this care process aims at enhancing continuity of care and system efficiency. It is applied currently in MH [61]. | Mainly used in the LN-Group | ||||
| Recovery approach: Personal journey that involves developing hope, a secure base and sense of self, supportive relationships, empowerment, social inclusion, coping skills, and meaning. In most longitudinal studies, recovery rates were 80% for bipolar disorders, 65% to 80% for major depression, 70% for SUDs and 60% for schizophrenia [6263]. | Mainly used in the SN-Group | ||||
| Strengths model: Intervention focusing on the strengths and interests of the user rather than pathology and oriented toward achieving goals set by the user him/herself. Mainly effective for severe MHD [64]. | Mainly used in the SN-Group | ||||
| Illness self-management: Systematic provision of education and supportive interventions in order to increase skills and confidence of the client in managing his/her health problems. Mainly effective for depression [65]. | Mainly used in the WH-Group | ||||
| Stepped-care: Care delivery model in which interventions are performed hierarchically based on the intensity of client problems. Mainly effective for depression [66]. | Little used, but more in the PH-Group | ||||
| 2.2- Administrative Strategies | |||||
Referral mechanisms:
| Mainly implemented in the PH- and WH-Groups | ||||
| Shared staff: Professionals offering services across more than one organization to insure coverage of the required range of services and to intensify inter-organizational collaboration [14]. | Little implemented, but more in the PH-Group | ||||
| SUD specialist respondents: Specialists in SUDs who hold case discussions with MH and other teams concerning SUDs, aiming to reinforce SUD expertise and interventions including SUDs and co-occurring MHD-SUDs. | Mainly implemented in the WH-LN-Groups | ||||
| Liaison officers: Professionals designated by an organization to relay information between departments of a single organization or between organizations serving the same clientele. [14]. | Mainly implemented in the PH- and SN-Groups | ||||
| Joint training: A strategy to enhance collaborative environments by simultaneously training clinicians with different areas of expertise and/or from different services or organizations in a network [53]. | Mainly implemented in the PH-Group | ||||
| Service agreements: Administrative strategy used for formalizing mechanisms to facilitate access and continuity of services between at least two organizations or programs in the same organization [14]. | Mainly implemented in the LN-Group | ||||
Table 3
Compositions and activities of mental health (MH) services.
| Variables | Categories | PH-Groupa | WH-Groupb | SN-Groupc | LN-Groupd | |||
|---|---|---|---|---|---|---|---|---|
| Primary care (n = 15) | Specialized care (n = 23) | Primary care (n = 2) | Primary care (n = 12) | Specialized care (n = 13) | Primary care (n = 4) | Specialized care (n = 12) | ||
| Mean % | Mean % | Mean % | Mean % | Mean % | Mean % | Mean % | ||
| Composition of professional teams [n(Mean)] | Psychologists | 3.4 | 0.9 | 10.8 | 0.9 | 0.7 | 6.8 | 1.0 |
| Social workers | 3.8 | 1.9 | 4.0 | 1.3 | 1.1 | 8.3 | 2.0 | |
| Psycho-educators | 3.2 | 2.0 | 10.0 | 0.9 | 1.8 | 7.0 | 0.9 | |
| Nurses | 2.4 | 3.9 | 7.3 | 1.2 | 5.8 | 3.0 | 9.6 | |
| Psychiatrists | 0.1 | 2.3 | 1.4 | 0.0 | 3.6 | 4.0 | 5.2 | |
| General practitioners (GPs) | 0.3 | 0.4 | 1.2 | 0.9 | 1.1 | 0.3 | 0.5 | |
| Professionals in substance use disorders (SUD) | 1.5 | 1.7 | 0.0 | 0.2 | 0.3 | 0.3 | 0.9 | |
| Time allocated by teams to [n (%)] | Treatment or intervention | 53.0 | 61.8 | 67.5 | 49.4 | 71.1 | 56.6 | 63.2 |
| Evaluation | 27.5 | 29.4 | 9.0 | 23.6 | 35.8 | 31.8 | 24.5 | |
| Coordination with other teams | 21.8 | 22.0 | 16.0 | 14.9 | 19.2 | 17.5 | 8.3 | |
| Clientele followed-up [n (%)] | Stabilized disorders | 58.3 | 22.5 | 41.6 | 52.5 | |||
| Common MH disorders (MHD) | 44.3 | 30.0 | 16.5 | 33.8 | ||||
| Severe MHD | 37.1 | 40.0 | 62.2 | 23.8 | ||||
| Personality disorders | 41.5 | 29.0 | 20.0 | 14.4 | 33.8 | 12.5 | 24.8 | |
| Chronic physical disorders | 32.3 | 17.5 | 21.8 | 8.3 | ||||
| Co-occurring MHD-SUDs | 37.5 | 47.1 | 50.0 | 31.2 | 50.1 | 32.3 | 33.3 | |
| Suicidal ideations | 27.8 | 33.2 | 45.0 | 14.8 | 33.8 | 28.8 | ||
| Co-occurring MHD and chronic physical disorders | 25.5 | 36.3 | 25.0 | 27.0 | 43.6 | 15.8 | 22.9 | |
| Problems with the law | 5.5 | 22.1 | 20.0 | 11.7 | 4.0 | 15.7 | ||
| High users | 21.1 | 34.6 | 22.5 | 14.1 | 4.5 | 11.2 | ||
| Psychotic disorders | 50.2 | 48.2 | 51.4 | |||||
| Mood disorders | 40.9 | 21.0 | 35.8 | |||||
| Anxiety disorders | 26.7 | 24.3 | 26.4 | |||||
| Bipolar disorders | 27.9 | 18.7 | 20.4 | |||||
| Frequency of visits [n (%)] | Once or more/month | 89.9 | 93.7 | 93.4 | 88.4 | 76.7 | 97.4 | 81.4 |
| Once/3 months | 6.8 | 4.8 | 5.0 | 0.7 | 12.5 | 1.7 | 9.3 | |
| Once/6 months | 1.9 | 1.2 | 1.7 | 2.8 | 6.3 | 0.9 | 4.6 | |
| Once/year | 1.4 | 0.3 | 0.0 | 8.1 | 4.5 | 0.0 | 4.8 | |
| Duration of client follow-up [n (%)] | >1 year (%) | 50 | 87.3 | 22.5 | 72.4 | 88.2 | 60.0 | 65.6 |
| < a year (%) | 20.9 | 11.8 | 35.0 | 13.8 | 10.6 | 26.7 | 8.5 | |
| < 6 months (%) | 12.7 | 14.5 | 27.5 | 12.1 | 18.9 | 18.3 | 0.7 | |
| < 3 months (%) | 31.9 | 77.9 | 17.5 | 23.3 | 47.1 | 45.0 | 69.5 | |
| Proportion of clientele referred to [n (%)] | MH Community organizations | 36.8 | 29.8 | 25.0 | 46.3 | 21.5 | 36.3 | 38.8 |
| Specialized MH services | 16.2 | 34.8 | 25.0 | 23.1 | 25.7 | 7.5 | 13.0 | |
| Intersectoral resources | 5.1 | 14.6 | 22.5 | 15.9 | 3.9 | 11.7 | 10.0 | |
| SUD rehabilitation centres | 10.9 | 12.8 | 7.5 | 10.2 | 11.6 | 11.7 | 23.4 | |
| Community organizations not in MH | 13.9 | 20.0 | 21.8 | 7.5 | ||||
| HSSCe-MH Primary care teams | 27.6 | 23.0 | 22.5 | |||||
[i] a: With a psychiatric hospital (PH); b: Without specialized MH services in the network; c: <200 000 inhabitants with psychiatric department in a general hospital (GH); d: >200 000 inhabitants with psychiatric department in a GH; e: Health and Social Services Centres (HSSC)-MH Primary care teams.
Table 4
Frequency of interactions with other services and organizations and satisfaction.
| Variables | Categories | PH-Groupa | WH-Groupb | SN-Groupc | LN-Groupd |
|---|---|---|---|---|---|
| Meand | Meand | Meand | Meand | ||
| Frequency of interactions from HSSCe-MHf primary care teams | General practitioners (GPs) in medical clinics | 3.4 | 3.5 | 2.7 | 3.5 |
| HSSC one-stop service | 2.9 | 4.5 | 3.6 | 3.3 | |
| HSSC general services | 2.5 | 3.0 | 3.7 | 3.5 | |
| Respondent-psychiatrists | 4.7 | 3.8 | 4.6 | 4.4 | |
| Emergency rooms | 3.1 | 2.5 | 4.3 | 3.3 | |
| Hospitalization units | 3.1 | 2.8 | 3.9 | 3.4 | |
| Day hospitals | 3.0 | 2.3 | 3.3 | 2.9 | |
| Community organizations | 2.6 | 3.0 | 2.8 | 2.5 | |
| Crisis centres | 3.1 | 4.0 | 2.9 | 4.8 | |
| SUDg rehabilitation centres | 3.5 | 4.0 | 2.8 | 3.3 | |
| Satisfaction of interactions from HSSC-MH primary care teams | GPs in medical clinics | 3.4 | 3.0 | 4.1 | 3.5 |
| HSSC one-stop service | 4.1 | 4.0 | 4.3 | 4.5 | |
| HSSC general services | 4.1 | 5.0 | 3.9 | 2.5 | |
| Respondent-psychiatrists | 4.6 | 3.5 | 4.4 | 5.0 | |
| Emergency rooms | 3.5 | 3.0 | 4.5 | 3.6 | |
| Hospitalization units | 3.9 | 2.7 | 4.2 | 3.5 | |
| Day hospitals | 4.4 | 3.5 | 4.8 | 4.8 | |
| Community organizations | 3.4 | 3.5 | 3.8 | 2.8 | |
| Crisis centres | 3.7 | 5.0 | 4.6 | 5.0 | |
| SUD rehabilitation centres | 4.9 | 4.0 | 4.3 | 4.0 |
[i] a: PH: with a psychiatric hospital; b: WH: without an hospital in the network; c: SN: small networks (<200 000 inhabitants with psychiatric department in a general hospital); d: LN = large networks (>200 000 inhabitants with psychiatric department in a general hospital); d: Mean from 0 to 5; 5 = better; e: HSSC: Health and Social Services Centres; f: Mental health; g: SUD: Substance use disorders.
Table 5
Integration strategies developed by HSSCa-MH primary care teams to consolidate care in their services or to integrated their services with specialized care.
| Variables | Categories | PH-Groupb | WH-Groupc | SN-Groupd | LN-Groupe |
|---|---|---|---|---|---|
| Clinical Strategies | Meanf | Meanf | Meanf | Meanf | |
| Evaluation/clinical tools | Screening tools for MHDsg | 3.6 | 1.5 | 2.3 | 1.7 |
| Screening tools for SUDh | 4.0 | 4.5 | 3.7 | 4.0 | |
| Assessment tools for MHDs | 3.6 | 2.0 | 2.7 | 2.7 | |
| Assessment tools for SUDs | 4.1 | 3.0 | 3.1 | 3.7 | |
| Assessment tools for client satisfaction | 2.5 | 2.0 | 1.9 | 2.7 | |
| Clinical protocols or best-practice guidelines | 2.9 | 5.0 | 3.1 | 3.7 | |
| Cognitive behaviour therapy (CBT) | 3.0 | 4.0 | 3.7 | 3.3 | |
| Clinical Approaches | Motivational interviewing (MI) | 3.1 | 4.0 | 3.3 | 3.0 |
| Care pathway | 3.0 | 3.0 | 2.3 | 3.7 | |
| Recovery approach | 2.7 | 2.5 | 3.4 | 2.7 | |
| Strengths model | 2.9 | 2.5 | 3.1 | 3.0 | |
| Illness self-management | 2.5 | 3.0 | 2.4 | 2.6 | |
| Stepped care | 2.5 | 1.0 | 1.4 | 2.3 | |
| Administrative Strategies | Meanf | Meanf | Meanf | Meanf | |
| Network resource directories | 4.9 | 4.0 | 4.0 | 4.0 | |
| Referral procedures within the organization | 4.4 | 5.0 | 4.3 | 3.7 | |
| Referral procedures between organizations | 4.3 | 5.0 | 3.9 | 4.0 | |
| Shared clinical records | 4.2 | 4.5 | 3.7 | 2.3 | |
| Shared staff | 2.3 | 2.0 | 2.1 | 1.3 | |
| Liaison officers | 3.2 | 2.0 | 3.0 | 2.3 | |
| Joint training | 3.4 | 2.0 | 2.7 | 2.7 | |
| Service agreements | 3.0 | 2.5 | 3.1 | 3.7 | |
| SUD specialist respondents | 2.2 | 3.0 | 2.4 | 3.0 | |
[i] a: HSSC: Health and Social Services Centres; b: PH: with a psychiatric hospital; c: WH: without an hospital in the network; d: SN: small networks (<200 000 inhabitants with psychiatric department in a general hospital); e: LN: large networks (>200 000 inhabitants with psychiatric department in a general hospital); f: Mean: from 0 to 5; 5 = greatest utilization; g: MHDs: Mental health disorders; h: SUDs: Substance use disorders.
