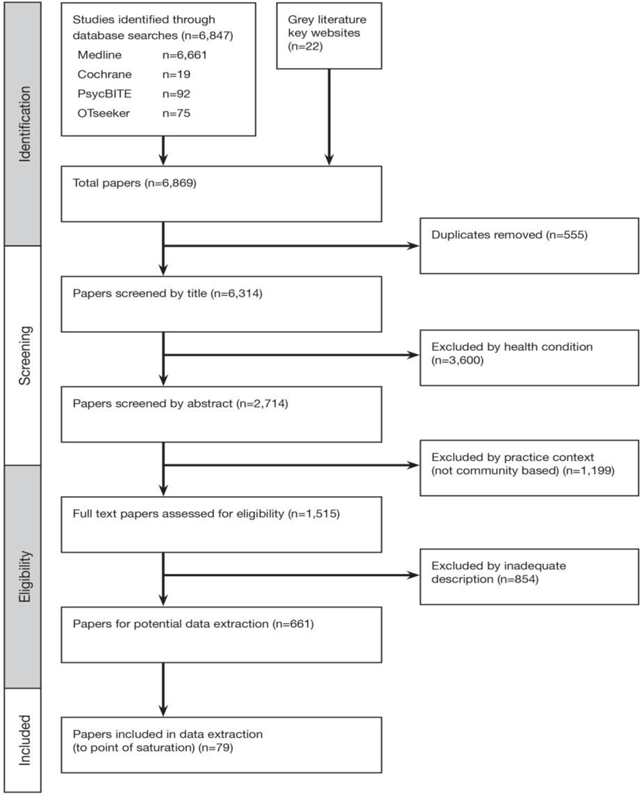
Figure 1
Flow of Study Selection.
Table 1
Description of the mapped papers.
| Published papers (n = 65) | Grey Literature (n = 14) | |
|---|---|---|
| Country of focus | ||
| Australia | 7 | 9 |
| Canada | 1 | 1 |
| Germany | 1 | 0 |
| Hong Kong | 1 | 0 |
| Japan | 1 | 0 |
| New Zealand | 0 | 1 |
| Spain | 1 | 0 |
| Sweden | 1 | 0 |
| United Kingdom | 5 | 1 |
| United States America | 33 | 2 |
| International | 14 | 0 |
| Health Condition | ||
| Mental Health | 26 | 0 |
| Diabetes/chronic or long term health condition | 8 | 0 |
| Brain injury | 8 | 4 |
| Spinal Cord Injury | 2 | 0 |
| Not specific | 21 | 10 |
| Type of paper/study | ||
| Systematic review | 1 | n/a |
| Qualitative study (includes literature review) | 40 | 2 |
| Intervention study (includes study protocols) | 7 | n/a |
| Theoretical paper | 11 | n/a |
| Editorial/perspective/expert opinion | 5 | 0 |
| Practice guidance/standards | 1 | 10 |
| Conference paper | 0 | 2 |
Table 2
Mapped models of case management, and related names, theoretical description and case management features.
| Model and mapped terms | Theoretical description | Case management features |
|---|---|---|
| 1. Broker – Service broker – Managed care – Medical case management – Generalist – Gatekeeper [92526272829]* | An impartial organizational or service focused approach to connect a patient to needed services and to coordinate between different service providers, with an emphasis on a network of providers thereby containing costs by preventing inappropriate access and use of services | Case managers attempt to assist clients to identify their needs and broker services and supports. Contact is limited. |
| 2. Clinical – Rehabilitation – Direct care [2830313233343536373839404142] | Involves clinical, collaborative, strategic and communication roles with patient and key stakeholders (e.g. providers, payers, employers): establishes comprehensive case management goals and objectives, interventions, and outcomes including specified timeframes; provides clinical interventions and brokers other clinical services; aims to assist, facilitate, monitor and resolve client issues using clinical skills, clinical services and community resources; may involve adjusting the therapeutic regimen or communicate the need for adjustment to other providers. The individual goals and needs of the client dictate the response and services. In the rehabilitation model this aim is to restore functional ability prior to the injury or illness; case management is extended to include identifying and assessing client skill deficits, barriers to achievement of personal goals, teach skills, provide support and responsibility for the continuity of care and coordinating services including in times of crisis. | Contact can be brief, or an episode of planned activity over 2–3 years. |
| 3. Chronic care – Long term – Integrated care – Standard [94344454647] | More system wide integrated care but tailored to the individual e.g. in primary practice working with a multi-disciplinary team and utilizing system supports. Provides proactive support by the team; and recognizes that quality care is predicated on productive interactions between clients, families and caregivers, providers ; case managers are providers with specific system supports (e.g., protocols), structured relationships with specialist expertise for consultation, support and integration; typically have strong links to the primary care provider to support ongoing coordinated and integrated care with follow-up; condition neutral and is applicable across conditions and risk factors | Longer term involvement with a focus on the integration of care and supports |
| 4. Strengths based [9272830383941484950515253] | Based on the premise of the client using their own strengths, resilience, interests, potentials, abilities and knowledge to lead to recovery rather than on their limits (deficits); adopts an ecological perspective that recognizes the importance of people’s environments (context), the individual’s resilience; emphasises the importance of the relationship with the case manager, to support and enable clients to develop skills | |
| 5. Assertive – Intensive case management – Recovery – Intensive comprehensive care [52953] | Assertive case management focuses on recovery rather than cure of the health condition (e.g., mental health). It involves; a team providing all necessary treatment and care (at home or work) in their natural environment rather than involving other services; aims to reduce hospitalizations: and purposively outreaches to clients to support their opportunities for choice and living a meaningful and satisfying life as a member of a community. Intensive case management addresses the social and health needs of people, is intensive and long term with an individual case manager. | Assertive: Clients are shared by a team to provide services including outreach, direct services such as counselling, skill development, family consultation and support, crisis intervention. Time of involvement is unlimited Intensive: small case load which are not shared across the team. Intensive comprehensive care: combination of assertive and intensive |
[i] *refer to Appendix 2 for details of the articles in scoping study.
Table 3
Examples of the terms in the literature mapped to component heading.
| Component Heading | Broad description | Mapped terms |
|---|---|---|
| 1. Case finding | To identify patients not in contact with services | – Assertive outreach – Detection of patients – Patient identification/outreach – Access – Outreach |
| 2. Establishing rapport | Focusing on the connection developed between the case manager and client Establishing alliance and collaboration with the patient | – Establish and provide a one-to-one relationship – Initial phase – Engagement – Building on the relationship (including with other providers) – Establishing accountability – Establish responsibilities – Negotiate responsibility – Establish therapeutic alliance – Establish long term collaborative and human relationship |
| 3. Assessment | Comprehensive understanding of the needs, capabilities and available resources and community services | – Need identification – Intake – Perform social diagnosis – Assess client and family – Interview – Assessment of needs (e.g. social support, levels of care, readiness and willingness for services, living situation, financial resources, access, barriers, home evaluation, need for referral – Community assessment – Gather information – Use comprehensive assessment instruments – Identify strengths and obstacles to attainment of goals – Cognitive and behavioural assessment – Identify present achievements, interests, resources, interests and aspirations – Document and communicate needs – Document aims and objectives – Estimate level of case management support required – Screening for co-morbid conditions – Determine decision making capacity |
| 4. Planning | Development of plan with client input including setting goals, actions steps towards achievement of goals and selection of resources | – Gatekeeper of funds – Discharge planning – Decision making – Resource identification – Setting goals with client – Goal setting – Design and implementation of care packages – “Moving forward” – Design of an individualized care plan – Determine comparative costs of alternate plan options – Review relapse prevention options – Plan for disengagement of case management |
| 5. Navigation | Facilitate safe and effective connections to services across settings | – Anticipate, identify barriers – Help remove barriers to holistic care |
| 6. Provision of care | Supply care directly or be delegation (relevant to qualifications and experience of case manager) | – Crisis intervention – Patient interventions – Supportive and formal therapeutic interventions – Therapy – Skills training – Patient interventions – Group work – Medication management – Symptom monitoring |
| 7. Implementation | Broker and implement the best package and arrange or purchase services on behalf of the client | – Care arranging – Service implementation – Clinical management – Communication – Arrange and activate services – Develop social networks – Locating and coordinating services – Perform a cost-benefit analysis – Identify formal and informal community resources and support programs – Collect and analyse data – Plan for clients transition along the continuum of care |
| 8. Coordination | Navigating the system of providers and resources needed, referral, facilitate multi-disciplinary collaboration, to ensure and advocate with other agencies for the appropriate use of resources and supports to client, including their purchase of the services themselves. | – Continuity – Linking – Linking to needed services – agency liaison – Environmental interventions – Resource management – Liaison – Facilitation – Interagency coordination – Resource acquisition – Facilitate transitions – Educate and facilitate – Referral – Negotiate – Facilitate patient access – Advocate with providers – Consultation with stakeholders |
| 9. Monitoring | – Proactive support – Monitoring service delivery – Monitor outcomes – Follow-up – Tracking clients – Maintain communication with stakeholders – Monitoring evaluation or reassessment – Maintenance/follow up – “Pushing/pulling and letting go” – Manage | |
| 10. Evaluation | Determine the clients progress toward established goals and outcomes and the effectiveness of care | Monitor outcomes and quality of care – Reassessment – Evaluate effectiveness including timeliness – Document client response – Evaluate availability of services needed – Determine. Prepare and communicate when case management services no longer required – Collect and analyse outcome data |
| 11. Feedback | General – Case consultation – Reports to treating providers – Maintain privacy and confidentiality – Regular meetings with treatment team to review goals and progress – Listen to stakeholders, collect information objectively | |
| 12. Education/information | Information and assistance to (e.g. client, family other service providers, workplace etc) to assist understanding of e.g. Health condition, Support services | – Providing information – Educate about early signs and symptoms – Assistance with applications, appropriate documents, |
| 13. Advocacy | Advocate for the client, best practice and the payer in line with client’s best interests | – Advocacy for social service programs, during hospitalisation etc – Advocate for more community-based services – Community advocacy – Obtaining financial assistance for the client – Intermittent function, affirmative, assertive approach to assisting client in receiving amenities or services that are being withheld unfairly. – Aiming to have gap/need filled – Assist clients to become autonomous and informed decision-makers |
| 14. Supportive counselling | Provide practical and emotional support, encouragement to facilitate knowledge, coping, adjustment and functioning | – Encouragement/support – Provision of problem solving support – Confrontation – Counselling – Individual, family or social support – Provision of emotional support – Conflict resolution – Provide practical and emotional support |
| 15. Administration | Complete administrative tasks | – Agency and other meetings – Complete paperwork – Treatment planning – Recording, report writing – Audits – Gathering statistics |
| 16. Discharge/Disengagement | Determining and planning for the appropriate time to discontinue case management including facilitating client independence and knowledge to self-manage condition and care needs | – Planning case closure – Case closure |
| 17. Community service development | Support local community to take collective action to develop new, adapt or grow services or generate solutions to common local problems | – Identify gaps – Use of statistics – Prepare funding submission – Create options with generic services – Identify and act on service gaps and overlaps at the client, community and population levels. |
