Table 1
Organizational Contextual Factors and Capabilities That Most Influence the Implementation and Delivery of Integrated Care: Results of Key Informant Interviews (n = 29).
| Semi-Structured Discussion (frequency) | Graphic Elicitation Ranking (frequency) |
|---|---|
| Partnering (116) | Clinician Engagement & Leadership (16) |
| Resources (103) | Patient-Centeredness & Engagement (12) |
| Readiness for Change (78) | Leadership Approach (11) |
| Clinician Engagement & Leadership (70) | Readiness for Change (9) |
| Delivering Care (56) | Information Technology (9) |
| Leadership Approach (51) | Organizational/Network Culture (9) |
| Patient-Centeredness & Engagement (31) | Resources (8) |
| Commitment to Learning (30) | Delivering Care (8) |
| Information Technology (29) | Governance (7) |
| Measuring Performance (27) | Partnering (4) |
| Governance (26) | Improving Quality (9) |
| Physical Features (19) | Measuring Performance (27) |
| Accountability (18) | Commitment to Learning (2) |
| Organizational/Network Design (16) | Accountability (2) |
| Organizational/Network Culture (15) | Physical Features (1) |
| Improving Quality (9) | Organizational/Network Design (0) |
| Work Environment (6) | Work Environment (0) |
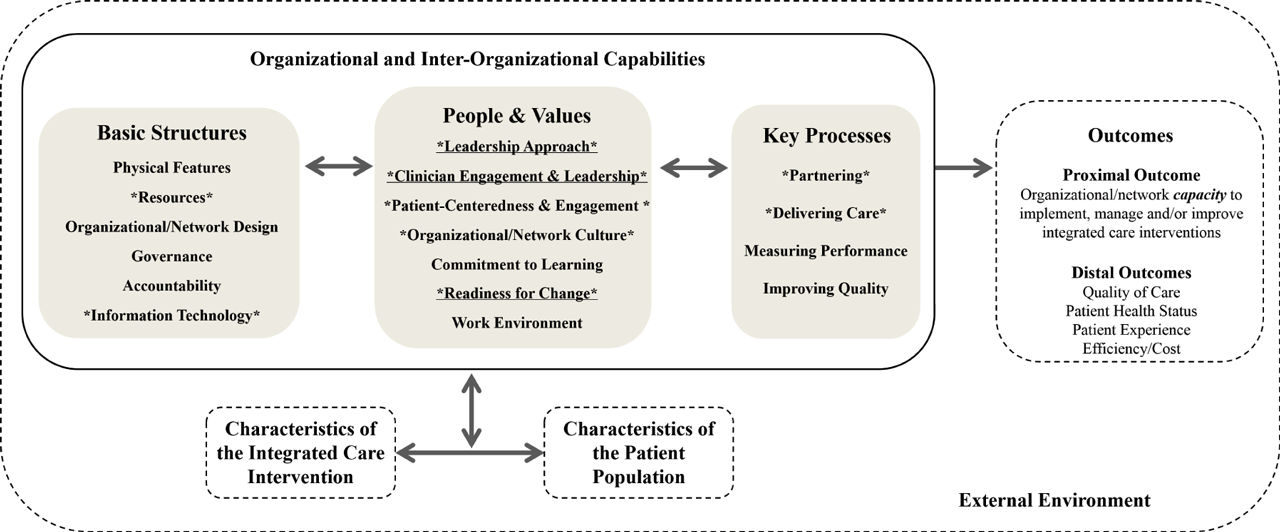
Figure 1
The Context and Capabilities for Integrating Care (CCIC) Framework. The CCIC Framework shows how organizational context and capabilities influence the implementation and outcomes of integrated care interventions. Contextual factors and organizational capabilities are organized into three categories: basic structures, people and values, and key processes. These contextual factors and organizational capabilities can be examined within organizations and across partnering organizations in a network. The nine contextual factors and organizational capabilities with the highest frequencies and highest rankings, based on key informant interviews, are depicted using an asterisk (*). The three most important organizational capabilities are underlined and asterisked; these are capabilities which ranked in the top six in both the quantitative content analysis of the semi-structured discussion and in the graphic elicitation. Boxes with dashed lines are outside of the scope of this study.
Table 2
Context and Capabilities for Integrating Care (CCIC) Framework: Definitions and Examples.
| Concept | Definition | Examples |
|---|---|---|
| Basic Structures | ||
| Physical Features | Structural and geographic characteristics of the organization/practice and network | organization/practice size and age, urban or rural location, facilities, geographic proximity of network members |
| Resources | Availability of tangible and intangible assets for ongoing operations at the organization/practice and for network activities | staffing, funding, knowledge, time, project management support, administrative support, brand/reputation |
| Governance | How the board or steering committee is organized and its activities to direct, manage and monitor the affairs of the organization/practice and network | board/committee composition, types of sub-committees, frequency of meetings, types of decisions made (e.g., extent of centralized planning and standardization) |
| Accountability | The mechanisms in place to ensure that people and organizations meet formal expectations in the organization/practice and network | regulations enforced by an authority (e.g., government), formal agreements between organizations (e.g., data sharing), organizational mandates, professional scope of practice |
| Information Technology | The availability and ease of use of technology-based communication and information storage mechanisms in the organization/practice and across the network | shared electronic medical records, email communication, video conferencing, data access and mining, tele-healthcare |
| Organizational / Network Design | The arrangement of units and roles and how they interact to accomplish tasks in the organization/practice and network | organizational chart (hierarchy), types of departments/programs, job descriptions, communication and decision-making channels (e.g., extent of centralization and formalization) |
| People and Values | ||
| Leadership Approach | The methods and behaviours used by formal leaders in the organization/practice or network (i.e., individual leaders, leadership teams, or lead organizations) | Personal vision for the organization/practice or network, strategies used to empower staff, leadership style and competencies |
| Clinician Engagement & Leadership | The formal and informal roles held by clinicians in the organization/practice and network, particularly physicians, that enable them to buy-in to and steer change, and influence others | active involvement of clinicians in planning, leading or supporting new initiatives (e.g., clinical champions or directors, networks led by primary care practices) |
| Organizational / Network Culture* | Widely shared values and habits in the organization/practice or network | perceptions regarding what is important and what is appropriate behavior |
| Focus on Patient-Centeredness & Engagement | Commitment to placing patients at the center of clinical, organizational and network decision-making | collection and use of patient feedback, consideration for patient needs and preferences, patient input and representation on committees as a standard practice, patient involvement in co-designing services |
| Commitment to Learning | The existence of a set of values and practices that support ongoing development of new knowledge and insights within the organization/practice and network | experimentation encouraged and rewarded, forums for meeting with and learning from other organizations and external experts, time and resources to reflect on past performance |
| Work Environment | How employees perceive and experience their job and their workplace in the organization/practice and network | opportunity for input, job satisfaction, burnout |
| Readiness for Change | The extent to which organizations and individuals are willing and able to implement change in the organization/practice and network | attitudes toward change and toward new or innovative ideas, extent of fit between current vision/strategy and the change |
| Key Processes | ||
| Partnering | The development and management of formal and informal connections between different organizations/practices | sharing information, sharing staff, engaging in collaborative problem-solving, building a common understanding and vision, exchanging knowledge, implementing referral and discharge/transfer agreements |
| Delivering Care | The methods used by providers in caring for patients in the organization/practice and network | inter-professional teamwork and joint care planning, use of standardized decision support tools, medical model vs. holistic model of care, shared patient-provider decision-making |
| Measuring Performance | The systematic collection of data about how well the organization/practice and network is meeting its goals | shared performance measurement framework, regular measurement and reporting, data access and mining |
| Improving Quality | The use of practices and processes that continuously enhance patient care in the organization/practice and network | providing quality improvement (QI) training to staff, systematic use of QI methods (e.g., process mapping, control charts), application of best practices |
[i] *Capabilities such as Focus on Patient-Centeredness and Engagement, Commitment to Learning and Readiness for Change may manifest in the culture of the organization or network.
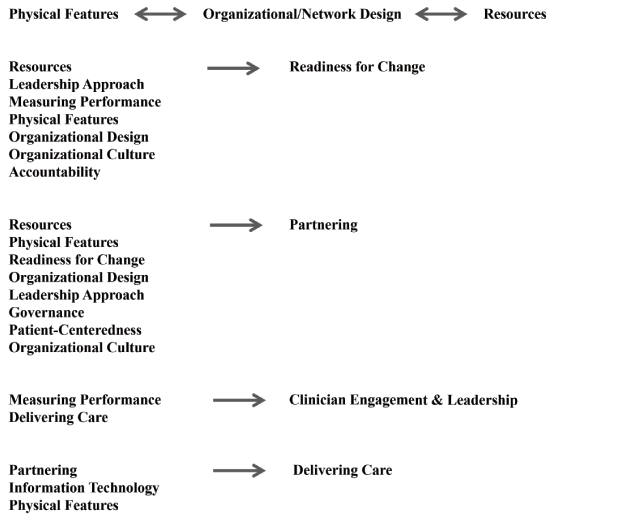
Figure 2
Most Important Hypothesized Relationships among Organizational Contextual Factors and Capabilities Based on Key Informant Interviews. The direction of the proposed relationships vary. Some of the relationships are positive, others negative, and some have the potential to be positive or negative, depending on the context and circumstances. Please refer to Supplemental File 1 for details on the proposed relationships.
