Table 1
List of Keywords/Mesh Terms.
| Key Terms: Role/Process | Medline Via Pubmed Mesh Term | Cinahl Plus – Cinahl Headings | Proquest Psycinfo – Thesaurus |
|---|---|---|---|
| Case manager / managers / management | Case management | Case Managers | n/a |
| Case worker / workers / working | Social Work | n/a | n/a |
| Key worker / workers / working | n/a | n/a | n/a |
| Care coordinator / coordinators / care coordination | n/a | nursing care coordination | n/a |
| Nursing care coordinator / nursing care coordinators / nursing care coordination | n/a | nursing care coordination | n/a |
| Service Manager / managers / management | n/a | n/a | n/a |
| multi-agency working / multidisciplinary team | n/a | multidisciplinary care team | |
| Key Terms: Patient Group | |||
| Children | Child, disabled children, hospitalized child | Child medically fragile, child disabled | n/a |
| Child | Child, hospitalized child, | Child disabled, child medically fragile | n/a |
| Paediatric / pediatric / paediatrics / paediatrics | Pediatrics | Pediatric care | Pediatrics |
| Young adult / young adults | Young Adult | Young adult | n/a |
| Youth / youths | Adolescent | Adolescence | n/a |
| Adolescent / adolescents | Adolescent, adolescent health services, hospitalized adolescent | Adolescent hospitalised / adolescent hospitalized | n/a |
| Young people | n/a | young adult | n/a |
| Young person / young persons | n/a | young adult | n/a |
| Key Terms: Context | |||
| Complex care | Tertiary Healthcare | Tertiary health care, multidisciplinary team | n/a |
| Disability | Disability evaluation, Disabled children, health services for persons with disabilities, chronic disease | Disability | n/a |
| Intellectual Disability / intellectual disabilities | Intellectual Disability | ||
| Disabled | Disabled children, health services for persons with disabilities, child health services, adolescent health services, health services needs and demands | Disabled | n/a |
| Chronic care | Long-term care | Multidisciplinary care team | n/a |
| Home telehealth | n/a | home health aides, home rehabilitation, home health care | n/a |
| Special health care needs | n/a | health services needs and demand, needs assessment | n/a |
| Medical complexity | n/a | n/a | n/a |
| Palliative care | Palliative care, hospice and palliative care nursing | Palliative care, hospice and palliative nursing, multidisciplinary care team, health services needs and demand | Palliative care |
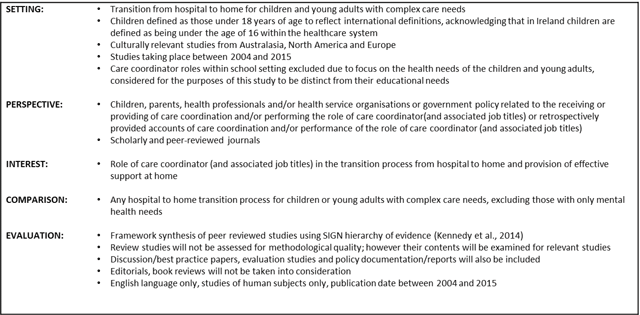
Figure 1
SPICE Framework and inclusion criteria.
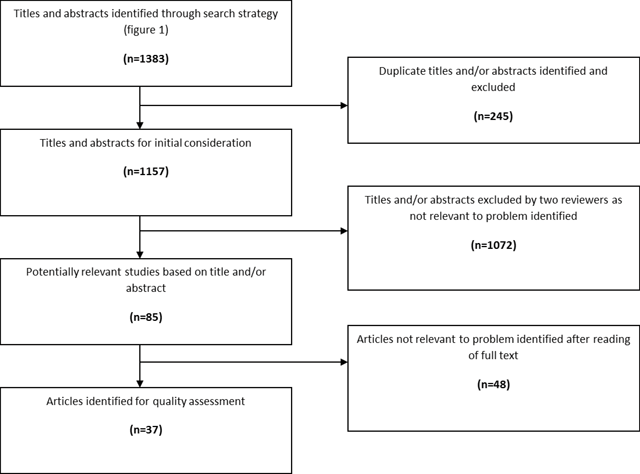
Figure 2
Search Result.
Table 2
Summary of articles reviewed.
| Author | Title | Approach | Sample Size | Empirical Research Perspective | Key Focus | Origin | Conclusions |
|---|---|---|---|---|---|---|---|
| Albanesi et al. (2009) | Role of disability-case manager for chronic diseases: Using the ICF as a practical background | Case Study | Single Case | Staff | Identifies how case managers contribute to care of children with disabilities | Italy | The case manager’s role is fundamental to support patients and their families; and one of its key interventions is the creation of a network around a person with complex care needs where this network does not exist. |
| Howitt (2011) | The family care coordinator: Paving the way to seamless care | Case study | Single case | Staff | Illustrate the concept of family care coordination through case study | Canada | Key components of the role are ongoing assessment, education, partnerships, communication, support and advocacy. Essential resources and pathways are required to implement the role and optimise outcomes. Challenges are identified to include time constraints, maintenance of boundaries and emotional burnout. |
| Care Coordination Network UK (2009) | Care Coordination Network UK: Key Worker Standards | Guidelines | Sets out guidelines for key worker standards | UK | |||
| Mengoni et al., (2014) | Developing Key Working | Guidelines | Offering guidelines to those developing key working services | UK | |||
| Department of Health (2009) | Integrated Care Pathway for Children and Young People with Complex Physical Healthcare Needs | Integrated Care Guidelines | Guide for community services in meeting the needs of families, children and young people, aged up to 18 years, who have complex physical healthcare needs | UK | |||
| Fraser et al. (2009) | Factors that influence case managers’ resource allocation decisions in pediatric homecare: An ethnographic study | Qualitative - Interviews, card sorts, participant observation over a 5 month period | 11 case managers | Staff | Factors that influence decision making by nurse case managers | Canada | The study provides new insights into resource allocation decision-making, offering a taxonomy to identify and classify influencing factors. |
| Ehrlich et al. (2009) | Coordinated care: what does that really mean? | Literature review | Identifies and examines the core attributes of care coordination within the primary care context | Australia | Offers a framework of coordinated care within the primary care setting that takes into consideration the key attributes of coordinated care that were identified during the review, with the aim of guiding future work around implementation and evaluation. | ||
| King and Meyer (2006) | Service integration and co-ordination: a framework of approaches for the delivery of co-ordinated care to children with disabilities and their families | Literature review | Aims to provide clarity and direction to provision of coordinated care | Canada | Offers a framework that can be used to support policy- and decision-making in the context of co-ordinated care provision. | ||
| McSpadden et al, (2012) | Care coordination for children with special health care needs and roles for physical therapists | Literature review | Summarise benefits of care coordination and explore potential roles for physical therapists | USA | Therapists need to be aware of and adapt to change in care models in order to be the provider of choice. | ||
| Robinson (2010) | Care coordination: a priority for health reform | Literature review | Outlines policy recommendations needed to enhance care coordination | USA | Recommendations include the need to facilitate better information transfer with wider use of information technology, include nurse practitioners as equal practitioners in reimbursement, create incentives to improve care coordination, reward the use of evidence based practice and advocate for better care coordination models | ||
| Greco et al. (2005) | An Exploration of Different Models of Multi-Agency Partnerships in Key Worker Services for Disabled Children: Effectiveness and Costs | Mixed methods | 225 Children with Disabilities Teams, 70% response rate, 87 interviews with key workers, questionnaires by 205 parents and 30 children | Multiple | Compare models of key working, identify areas for best practice, investigate sources of funding | UK | Key workers provide a valuable service that has a positive impact on many families’ lives and their collaborative approach facilitated access to appropriate support. However, outcomes vary across different areas, dependent on service management, understanding of the role and provision of training and supervision |
| Rahi et al. (2004) | Meeting the needs of parents around the time of diagnosis of disability among their children: evaluation of a novel program for information, support, and liaison by key workers | Mixed methods | 79 families from pre-group and 68 from post (68% and 65% response) | Family | Care coordination needs at time of diagnosis | UK | The greatest needs during the critical period around diagnosis are for information as well as emotional support from professionals, informal & formal networks and support groups. |
| Rodriguez and King (2014) | Sharing the care: the key-working experiences of professionals and the parents of life-limited children | Mixed methods | 35 at focus group, 25 interview | Multiple | Exploring the lived experience of caring and care planning for children with life limiting conditions | UK | The findings are limited by sample characteristics however they provide insight for current policy & practice initiatives. Key works need to be mindful of historic care arrangements and be prepared to step into the ‘family team’ arrangements. |
| Taylor (2012) | Implementing a care coordination program for children with special healthcare needs: partnering with families and providers | Mixed methods | 91 patients under care of care coordination counsellor, 439 patients provided with care binder | Multiple | Service evaluation, evaluating impact of care coordination counsellor service | USA | Patients supported by the counsellor service reported greater agreement when accessing resources and identifying a key point person for coordination. |
| Wood et al. (2009) | A multi-method assessment of satisfaction with services in the Medical Home by parents of children and youth with special health care needs (CYSHCN) | Mixed Methods | 6 practices, 262 (75% response) families completed questionnaire, 28 families in focus groups | Family | Assess satisfaction of parents with treatment by office staff, communication with the paediatricians, involvement in decision making and coordination of services outside the practice | USA | Paediatricians must become better equipped to identify and communicate more proactively with parents of children with CYSHCN who are under significant stress; and they and their staff must also improve their knowledge of community resources. |
| Webb et al. (2008) | Key workers and schools: meeting the needs of children and young people with disabilities | Mixed methods – interviews 7 service managers, 32 steering group members and 50 key workers, questionnaires completed by 189 parents and subset of 68 parents for interview | 7 case study areas | Multiple | Relationship between key worker services to promote inter agency care coordination and schools | UK | Key workers can improve home-school relationships, facilitate the contribution of teachers in inter-agency working, enable mainstream schools to better meet the needs of pupils with disabilities and improve their inclusive practice. |
| Beecham et al. (2007) | The costs of key worker support for disabled children and their families | Mixed methods – interviews and questionnaire | 7 service sites | Multiple | Identifies costs associated with providing care coordination services | UK | The low response rate and absence of data on some elements impacts generalisation of findings. Their findings highlight that contact costs varied depending on level of disability and number of role aspects performed by the key worker. |
| Cady et al. (2014) | Attributes of Advanced Practice Registered Nurse Care Coordination for Children With Medical Complexity | Mixed methods – interviews, documentary analysis, survey | 2628 care coordination episodes conducted by telehealth over consecutive 3 year time period for 27 children | Multiple | Investigates attributes of relationship-based advanced practice registered nurse care coordination | USA | The advanced practice registered nurse care coordination model has potential for changing the health management processes for children with medical complexity. |
| Purves et al. (2008) | The development of care coordination services in Scotland: A report to Care Co-ordination Network UK | Mixed methods, questionnaire to all 32 Scottish local authorities, telephone interviews | 22 questionnaires returned (69% response) | Staff | Demonstrates extent to which progress has been made in Scotland since 2004 and highlights where further work is needed | UK | There are number of challenges facing care coordination services including: funding issues, ongoing challenges of interagency working, qualification criteria, proliferation of coordinated planning mechanisms, providing family & child-centred services, understanding of the key worker’s role, the training and the development of key workers |
| Fitzgibbons et al. (2009) | Care management for children with special needs: Part II: the role of primary care | Documentary analysis | 2 Primary care practices in 5 counties in Washington state | Patients (children 17) with or at risk of a chronic condition as per Clinical Risk Groups Software. 189 initially selected (final sample 161) | Documents care management services | USA | Paediatric clinical care management activities directly relate to patient care and are complementary to, not duplicative of, case management provided by health plan managers. |
| Carter et al. (2007) | An exploration of best practice in multi-agency working and the experiences of families of children with complex health needs. What works well and what needs to be done to improve practice for the future? | Qualitative – appreciative interviews, nominal group workshops and consensus workshops | 20 mothers, 7 fathers, 1 child, 41 working with children | Multiple | Discusses what works well, why it has worked well and what best practice in the future could be | UK | The results suggest that parents need the opportunity to share and receive support from other parents who understand the reality of caring for a child with complex needs. Collaborative working needs to underpin the appointment of the most appropriate person to act as long-term coordinator where required by families. |
| Golden and Nageswaran (2012) | Caregiver voices: coordinating care for children with complex chronic conditions | Qualitative – focus group | 14 care givers | Family | Explores care givers’ perspective | USA | More information sharing and quality communication is needed among those providing care, caregivers need help in navigating the system of care, and caregivers develop strategies to cope with care coordination demands. The burden of coordinating care can be alleviated in part through improved communication and collaboration. |
| Ehrlich et al. (2013) | How does care coordination provided by registered nurses “fit” within the organisational processes and professional relationships in the general practice context? | Qualitative – interpretative, using focus groups | 9 registered nurses from 5 general practices | Staff | How nurse provided care coordination can fit into organisational processes | Australia | Registered nurse-provided care coordination could ‘fit’ within the context of general practice if it was adequately resourced. Successful development of the role requires attention to educational preparation, support of the individual nurse and attention to organisational structures. |
| Law et al. (2011) | Managing change in the care of children with complex needs: healthcare providers’ perspectives | Qualitative, semi structured interviews, focus groups, telephone interviews | 3 nursing and four allied health managers telephone interviewed, focus groups with 15 nursing and 11 AHP, and 3 nurses and 1 speech therapist interviewed by phone | Staff | Description of the role and activities of nursing and AHP caring for children with complex needs in a community setting | UK | Findings support the adoption of integrated partnership working, going beyond the identification of key professionals, to developing a set of criteria against which future service provisions could be judged. |
| Kingsnorth et al. (2015) | Inter-organizational partnership for children with medical complexity: The integrated complex care model | Qualitative, semi-structured interviews, focus groups, document review and audit of administrative databases | 12 families, 10 committee members, 7 key workers, 4 healthcare professionals - 21 in total for focus groups | Multiple | Identification of areas where care coordination can be improved at a systems level | Canada | At a systems level the integrated model fostered collaboration between partner organisations. At family level, development of inter-organisational management structures and communication platforms, provision of adequate resourcing, and increased engagement of primary care may enable high level organisational integration aimed at improved care coordination. |
| Brustrom et al. (2012) | Care Coordination in the Spina Bifida Clinic Setting: Current Practice and Future Directions | Semi structured interviews with clinic staff, focus groups with care givers | 43 staff, 38 caregivers through focus groups | Multiple | Examines elements of care coordination in spina bifida clinic setting | USA | Study findings suggest ways that care might be coordinated optimally in spina bifida clinics. A synthesis of these findings for clinics interested in implementing care coordination or improving the care coordination services they currently offer is provided. |
| Sloper et al. (2006) | Key worker services for disabled children: What characteristics of services lead to better outcomes for children and families? | Quantitative | 189 parents across 7 key worker schemes | Family | Examines which aspects of key worker schemes are related to better outcomes for families | UK | There is a need for regular training, supervision and peer support for key workers and negotiated time and resources for them to carry out the role. These influence the extent to which key workers can carry out aspects of the role and their amount of contact with families, which in turn impacts outcomes. |
| Palfrey et al. (2004) | The pediatric alliance for coordinated care: evaluation of a medical home model | Quantitative - completion of survey at baseline and follow up at 2 years. | 150 children with complex needs from 6 practices | Family | Determine satisfaction with care coordination intervention | USA | The PACC medical home intervention increases parent satisfaction with pediatric primary care. Those whose needs are most severe seem to benefit most from the intervention. There are some indications of improved health as well as decreased burden of disease with the intervention in place. |
| Antonelli et al. (2008) | Care coordination for children and youth with special health care needs: a descriptive, multisite study of activities, personnel costs, and outcomes | Quantitative – document analysis. Adaptation of the University of Massachusetts Medical School Care Coordination Measurement Tool | 6 general paediatric practices | Documentary analysis | Examines activities carried out by care coordinators and costs associated with role of care coordinator | USA | The presence of acute, family-based social stressors was a significant driver of need for care coordination activities. A high proportion of dependence on care coordination performed by physicians led to increase costs. Office-based nurses providing care coordination were responsible for a significant number of episodes of avoidance of higher cost use outcomes. |
| Greco and Sloper (2004) | Care co-ordination and key worker schemes for disabled children: Results of a UK-wide survey | Quantitative, postal survey | 225 Children with Disabilities Teams, 70% response rate | Staff | Explore the nature and variation of care coordination services | UK | The proportion of areas having care coordination or key worker services is consistent with findings on research with parents of disabled children. The extent of multiagency involvement in planning and overseeing the operation of the service was positive but joint funding was more problematic. There was considerable variation in service models. |
| Park et al. (2009) | The Evidence Base for Case Management Practice | Quantitative, secondary analysis | 4,419 case managers responding to online survey conducted by Commission for Case Manager Certification | Activity analysis | Compare case management activities and knowledge elements by profession and work setting | USA | There is evidence for how to develop case management programs consistent with both organisational characteristics and strengths of the nursing profession. |
| Petitgout et al. (2013) | Development of a hospital-based care coordination program for children with special health care needs | Service Evaluation | Describes the development of a hospital based inter-professional care coordination program for children with complex care needs | USA | Pediatric nurse practitioners play an important role in the medical home, collaborating with primary care providers, hospital-based specialists, community services, and social workers to provide services to children with special health care needs. |
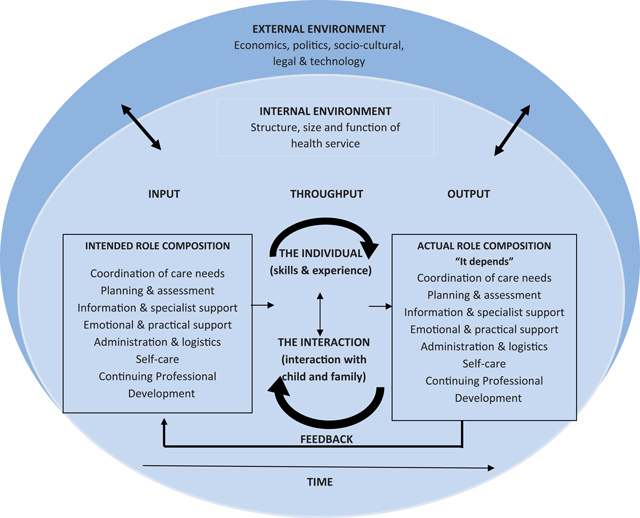
Figure 3
Conceptual map of findings.
