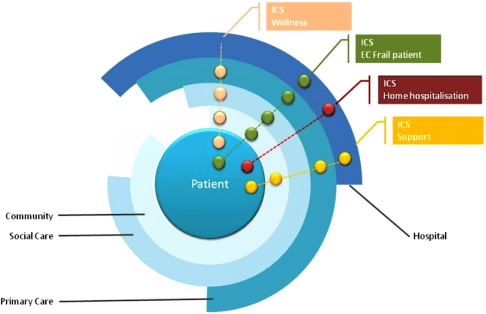
Figure 1.
Service model. The family of four Integrated Care Services deployed in NEXES with support of Information and Communication Technologies exemplifies the health paradigm based on longitudinal patient-centred care structured to achieve well-defined objectives with a continuum across the different layers indicated in the figure. Implicit in the model there are shared agreements among actors involving: informal (community) and formal care (primary care and hospital), as well as social support services. Enhanced accessibility of active patients/caregivers and collaborative work among professionals are basic characteristics of the model (see text for further details on the different Integrated Care Services supported by Information and Communication Technologies).
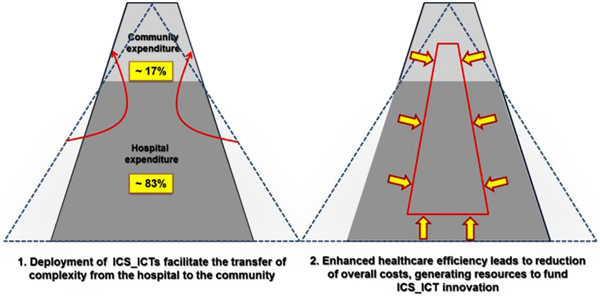
Figure 2.
Expected initial effects of the introduction of Bundled Systems with shared risks. The top portion of the left triangle (discontinuous line) indicates the per cent of hospital expenditure (–17%) that can be transferred to the community as Integrated Care Services. Those services are less intensive and less expensive. It will likely enlarge the top portion of the left figure (>17%) narrowing its base (<83%) in order to achieve aggregate cost savings and better margins (for a given reimbursement rate). The right figure displays the expected changes at provider's level after reorganization through Integrated Care Services supported by Information and Communication Technologies. The provider would have broader incentives to achieve savings over time (arrows), so that margins stay larger or increase.
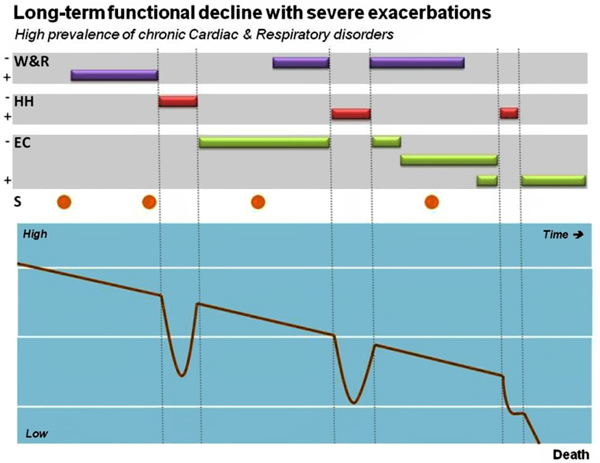
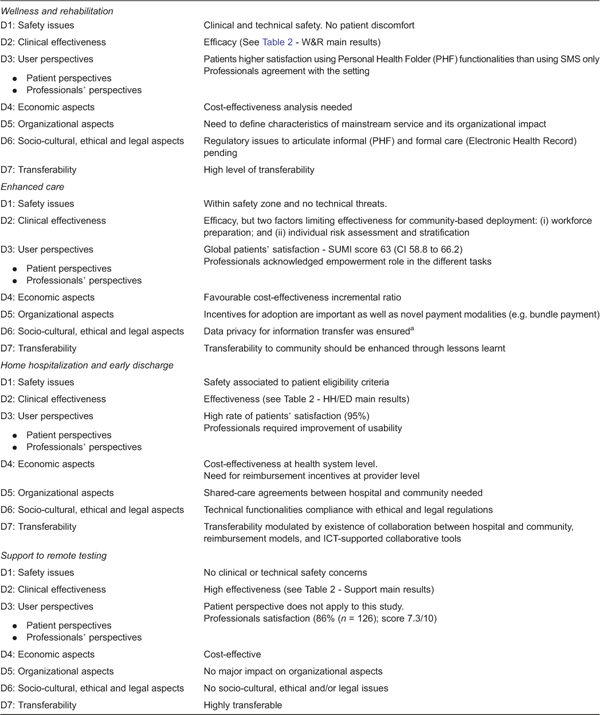
Figure 3.
Positioning Integrated Care Services supported by Information and Communication Technologies in chronic patients across time. The four Services were conceived as articulated services covering most of the complexities of chronic patients during the lifetime period. Functional decline overtime and occurrence of exacerbations are common features in chronic patients, acknowledging that both rate of progress and frequency/severity of acute episodes may show large variations among individuals and the characteristics of the predominant disease(s). The different Services can be administered alone or in combination, with different intensities/duration and also different purposes, as displayed. For example, the support to remote diagnosis (S) can be used either for initial diagnosis or for monitoring during the follow-up period.

Figure 1S.
30-day readmissions
Comparison of 30-d readmission rates for patients with Chronic Obstructive Pulmonary Disease, expressed as percentages, between the Catalan region, the Hospital Clinic and the Integrated Care Unit at Hospital Clinic (see text for details).
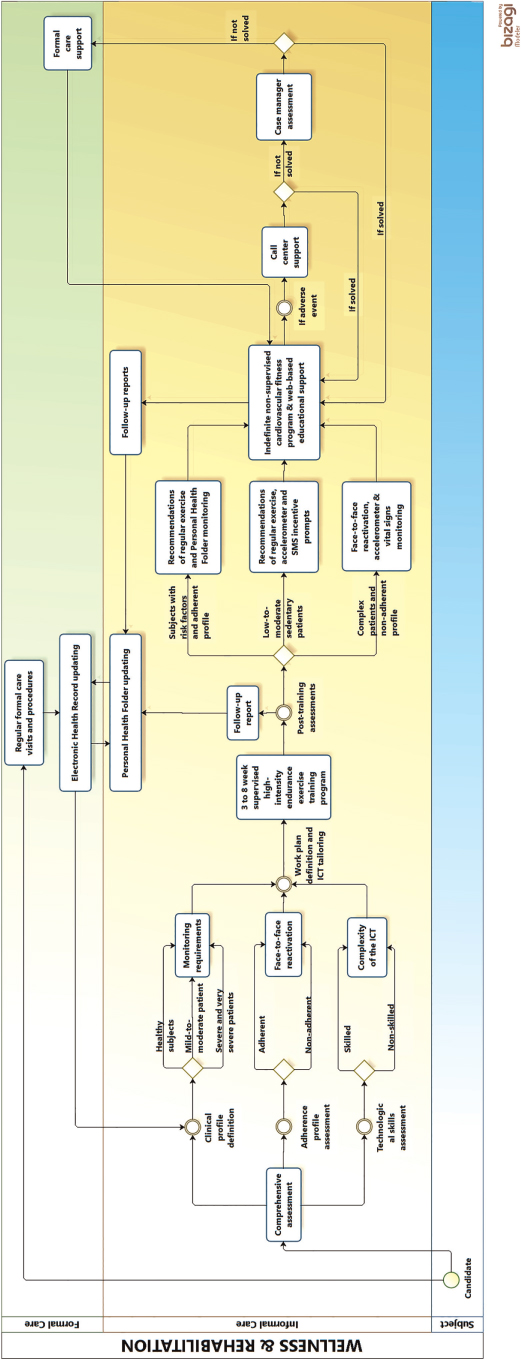
Figure 2S.
Wellness and Rehabilitation
Clinically stable chronic patients (cardiac, respiratory and/or type II diabetes mellitus), at different disease stages, that are eligible for an endurance training program are included into Wellness & Rehabilitation through formal (primary care or specialized care) or informal care (health center, pharmacy offices) providers. Basic assessments at entry into the service are conducted in order to define the work plan based on clinical characteristics, baseline aerobic capacity and adherence profile. Skills and acceptability of supporting technology for the non-supervised period of the program are also evaluated. The patient is then included into a supervised training program (3 to 8 weeks of duration). At the end of the supervised training period, he/she is included into the Integrated Care Service for community-based remotely assisted wellness program managed using his/her personal health folder. Additional supporting technology can be added depending upon requirements and patient's skills. During this non-supervised period, the patient has access to health professionals through the personal health folder and the call center (see text and reference [5] for further details).
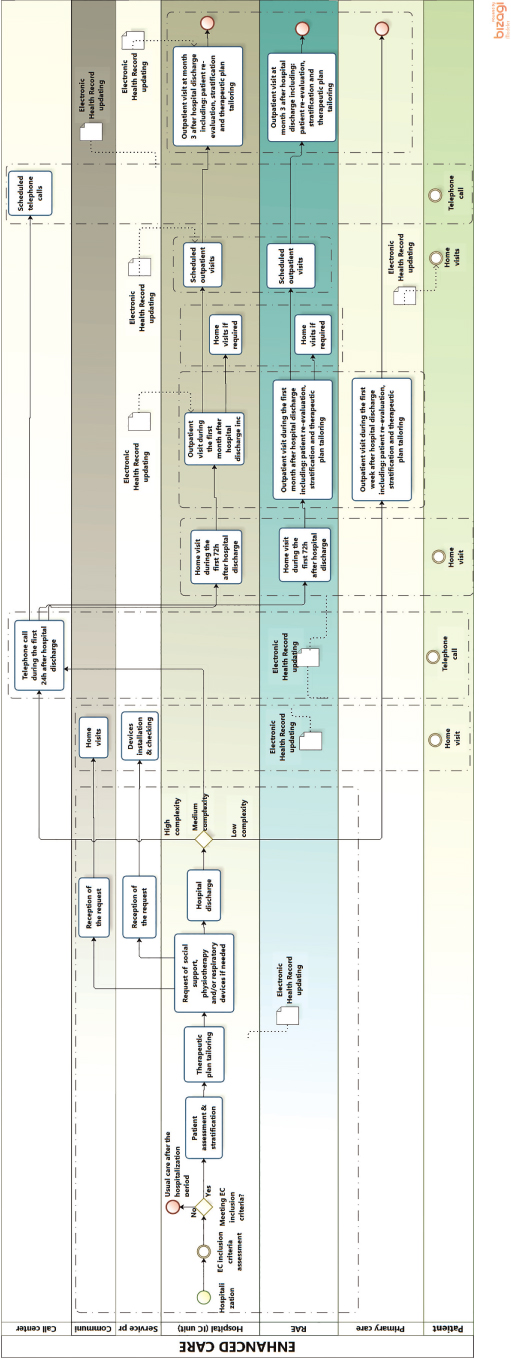
Figure 3S.
Prevention of admissions in frail chronic patients with previous history of repeated hospitalizations (EC)
Patients eligible for the service are frail with previous history of repeated hospitalizations. They can be admitted to the program either from the community or at discharge from an acute event (hospitalization ward, Home Hospitalization/Early Discharge, Day Hospital), as displayed in the figure. The Integrated Care team performs a comprehensive assessment of the eligible patients. During the evaluation process the patient receives a portfolio with: i) accessibility to the call center; ii) therapeutic plan including pharmacological and non-pharmacological aspects; and, iii) provision of supporting technology according to patient's needs established by the therapeutic plan, but also taking into account acceptability and technological skills. During the stud there has been a clear tend to adapt self-monitoring to the real needs of the clinical process as well as to explore tools management tools as the personal health folder.
A first visit at home together with primary care professionals was done within 72 hours of admission to the program. No subsequent visits were planned, but the patient had accessibility to program. The latter was customized depending upon the stratification level displayed in the figure.
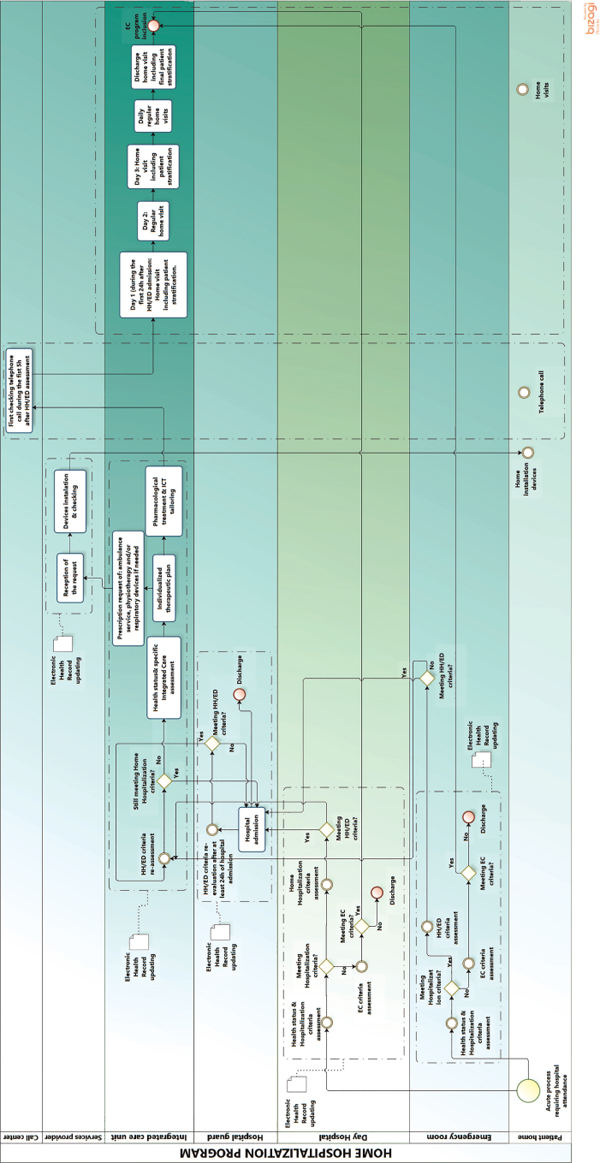
Figure 4S.
Home Hospitalization and Early Discharge (HH/ED)
Patients eligible for the Home Hospitalization/Early Discharge present criteria for hospitalization. The entry into in this service can be through different areas: Emergency room, Day Hospital or general hospitalization ward. The flow of the program is as follows: i) the staff of the corresponding department identify eligible patients for Home Hospitalization/Early Discharge and they are offered to be attended at home. If the Home Hospitalization /Early Discharge option is accepted by the patient, the Home Hospitalization/Early Discharge team proceeds to assess and confirm the criteria for admission into the program; ii) the patients signs the informed consent; iii) the Home Hospitalization/Early Discharge team does a comprehensive evaluation and establish the initial working plan to be developed at home; iv) before the transfer at home the patient receives a portfolio including: accessibility to the Call Center; pharmacological treatment that was prepared by the hospital pharmacy; description of the therapeutic plan including a basic educational program; and; logistics for delivery of complementary equipment (sensors, nebulizer, oxygen therapy, ….) depending on treatment plan previously defined; v) an ambulance transfers the patient at home; and, at the end of the process, vi) the patient receive a phone call from the Home Hospitalization/Early Discharge within a period of 5 hours to assess the status of the patient at home and to ensure that the logistics is fully operational.
The first home visit by a specialized nurse of the Home Hospitalization/Early Discharge team is carried out within 24 hours followed by a regime of daily visits. The program facilitates respiratory physiotherapy as needed. If the evolution of the patient is not positive, the Home Hospitalization/Early Discharge can program visits to a Day Hospital for assessment or plan a hospital admission. At discharge from Home Hospitalization /Early Discharge, the patients are allocated to the appropriate health care level or included into another Integrated Care Service according to his/her needs and established working plan. A discharge report was prepared by the Home Hospitalization/Early Discharge team. The discharge visit is performed by one Home Hospitalization/Early Discharge team member at patient's home.
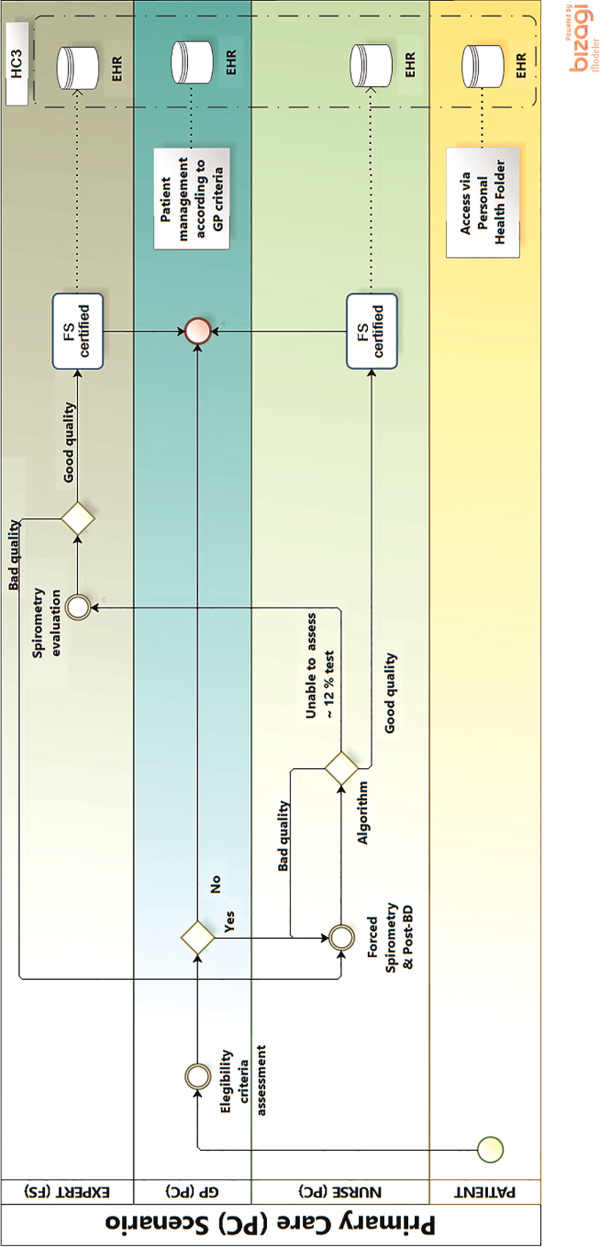
Figure 5S.
Support to remote diagnosis in Primary Care (Support_1)
Forced Spirometry transfer to Primary Care. The figure depicts the clinical process of a patient with respiratory symptoms attending a primary care visit. The flow is as follows: the general practitioner decides that the patient is a candidate for Forced Spirometry testing and both baseline and post-bronchodilator studies will be done by a non-specialized nurse. At the end of the testing, the results will be automatically assessed using the algorithm that will generate Forced Spirometry certification for quality. The three possible outcomes are: i) the Forced Spirometry testing qualify as high quality. It will be used by the General practitioner for his/her decision-making process and the certified Forced Spirometry will be sent to the patient's Electronic Health Records and to the regional repository (shared Electronic Health Records or “Catalan Electronic Health Records” (Historia Clinica Compartida de Catalunya)); ii) the Forced Spirometry testing does not fulfill quality criteria. Then automatic feedback with specific information on the problem is forwarded to the nurse while the patient is still on site. Consequently, the nurse will have the opportunity to solve the problem and generate a high-quality Forced Spirometry test; and, iii) approximately 12% of the Forced Spirometry testing will be classified as undefined by the automatic algorithm and forwarded to the specialist for advice. The specialist will provide remote off-line recommendations directly to both the General Practitioner/nurse and the patient will be attended by the General Practitioner who will take the final decision on how to proceed. In two of these scenarios, the first and the third, the certified Forced Spirometry will be forwarded to the regional Electronic Health Records or “Catalan Electronic Health Records” (Historia Clinica Compartida de Catalunya).
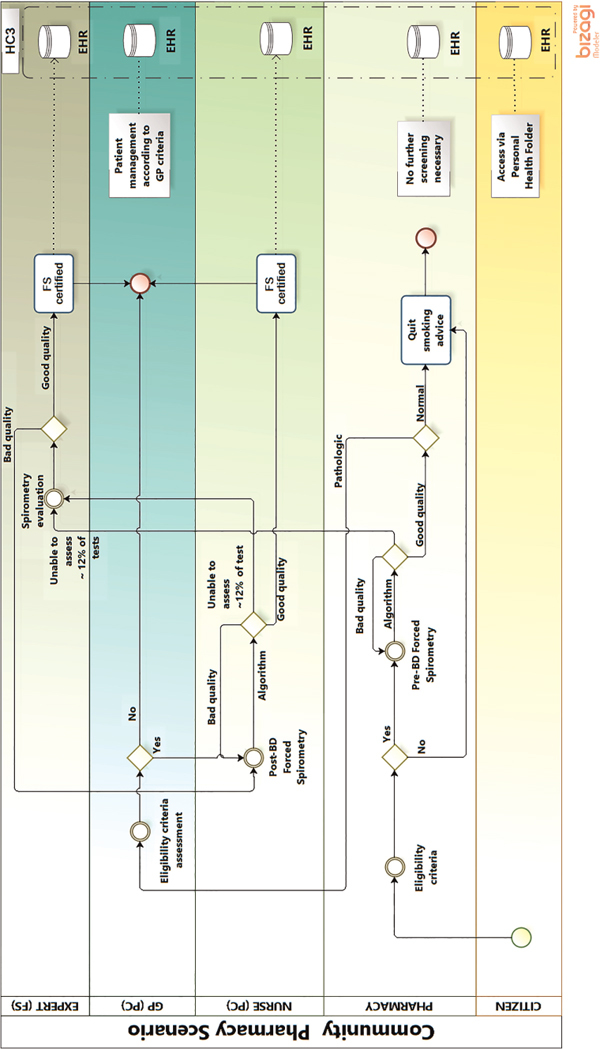
Figure 6S.
Support to remote diagnosis in Primary Care (Support_2)
Role of Pharmacy Offices (Community Pharmacy) in a Chronic Obstructive Pulmonary Disease case finding program. The figure depicts the process of a citizen/customer attending a Community Pharmacy where he/she sees a banner inviting participation in a respiratory health status assessment program. If the citizen decides to apply, then the Community Pharmacy officer will administer the Chronic Obstructive Pulmonary Disease questionnaire to assess health status. If risk factors are identified, the citizen will be invited to perform a pre-bronchodilator Forced Spirometry testing carried out by the Community Pharmacy officer. Regarding the quality of the testing, there are three possible outcomes: i) the Forced Spirometry testing is qualified as high quality and it will be certified as such by the automatic algorithm and forwarded to the regionally shared Electronic Health Records (or “Catalan Electronic Health Records” (Historia Clinica Compartida de Catalunya); ii) the Forced Spirometry testing does not fulfil quality criteria. Then, automatic feedback with specific info on the problem is forwarded to the Community Pharmacy officer while the patient is still on site. Consequently, the Community Pharmacy officer will have the opportunity to solve the problem and generate a high-quality Forced Spirometry test; and, iii) approximately 12% of the Forced Spirometry testing will be classified as undefined by the automatic algorithm and forwarded to the specialist for advice. The specialist will provide remote off-line recommendations directly to the Community Pharmacy officer and the certified Forced Spirometry testing will be forwarded simultaneously to the regionally shared Electronic Health Records The citizen's flow in the case of high-quality Forced Spirometry testing can be as follows: i) Normal Forced Spirometry testing: the Community Pharmacy officer will generate a report on paper giving tests results and advice about stopping smoking; ii) Abnormal Forced Spirometry results: the Community Pharmacy officer will generate a report on paper advising the subject to contact his/her general practitioner, who will have access to the certified Forced Spirometry testing through the “Catalan Electronic Health Records” (Historia Clinica Compartida de Catalunya); and iii) Undefined results (12% of the testing): the subject will be informed of the specialist's advice by the Community Pharmacy officer.
Table 1.
Main characteristics of the sites

M, man; W, women; GDP, gross domestic product; Suppl., supplemental; RCTS, randomized controlled trials; ICT, information and communications technology; HI, health information.
Table 2.
Summary of the field studies assessing the four integrated care services
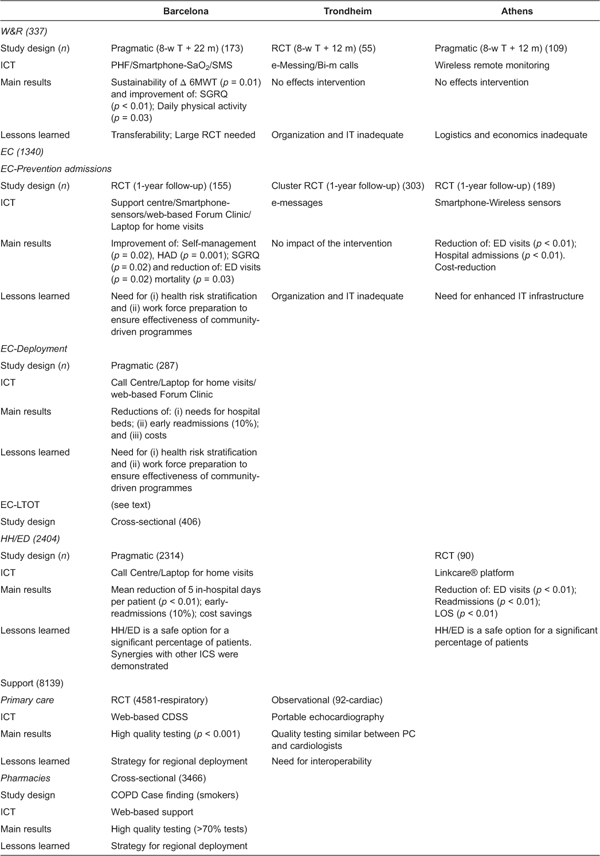
Number of patients within parenthesis.
COPD, chronic patients with obstructive pulmonary disease; W&R, Wellness and Rehabilitation; EC, Enhanced Care; EC-Prevention Admissions, Prevention of Admissions; EC-LTOT, Long-term Oxygen Therapy; HH/ED, Home hospitalization and Early Discharge; Support, Remote support for diagnosis; 8-w T + Xm, 8-week Training programme and follow-up after training; PHF, Personal Health Folder; ICT, Information and Communication Technology; RCT, Randomized Controlled Trials; SaO2, oxygen saturation pulse oximetry; SMS, Short Message Service; e-Messing and Bi-m calls, messaging services using ELIN platform; IT, Information Technology; HAD, Anxiety & Depression; SGRQ, Saint George Respiratory Questionnaire; ED, Emergency Department; web-based Forum Clinic, web-based patient education; CDSS, Clinical Decision Support System.