Table 1
Results Quality Appraisal.
| RCT’s Author (y) | Questions (Dutch Cochrane for RCT’s instrument) | TOTAL/9 | Quality appraisal: Medium/High | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| Bellantonio, 2008 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | medium |
| Berggren, 2008 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | high |
| Berglund, 2013 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | medium |
| Boult, 2008 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | medium |
| Boyd, 2009 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | high |
| Bryant, 2011 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 | medium |
| Chapman, 2007 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 4 | medium |
| Counsel!, 2007 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | high |
| Counsell, 2009 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | high |
| Denneboom, 2007 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 | medium |
| Hogg, 2009 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | high |
| Markle-Reid, 2010 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | high |
| Mudge, 2012 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5 | medium |
| Phelan, 2007 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 | medium |
| Respect team, 2010 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | high |
| Ryvicker, 2011 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 | medium |
| Stenvall, 2007a | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | medium |
| Stenvall, 2007b | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | high |
| Unutzer, 2008 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | medium |
| Van Leeuwen, 2009 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | high |
| Wu, 2010 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 | medium |
| Young, 2007 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 | medium |
| For all questions 1 = yes 0 = no or? Questions: 1. Randomization? 2. Allocation concealment? 3. Patient blinding? 4. Blinding of administrator of treatment? 5. Blinding outcome assessment? 6. Similarity of groups at the start of the study? 7. Descriptions of losses to follow-up/withdrawals? 8. Intention-to-treat analysis? 9.Groups equally provided of care? Note: Publications with a score < 4 were excluded. | |||||||||||
| SR Author (y) | Questions (Dutch Cochrane for SR instrument) | TOTAL/ 8 | Medium/High | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
| Gates, 2008 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | high |
| Handoll, 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | high |
| Nazir, 2013 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | high |
| Stroke Unit Trialists’, 2007 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | high |
| Cameron, 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | high |
| For all questions 1 = yes 0 = no or? Questions: 1. Question adequately formulated? 2. Quality of search? 3. Selection procedure? 4. Quality appraisal? 5. Description of data extraction? 6. Description of study baseline characteristics? 7. Clinical and statistical heterogeneity? 8. Statistical pooling? Note: Publications with a score < 4 were excluded. | ||||||||||
| Cross sectional study’s Author (y) | Questions (Dutch Cochrane for cohort research) | TOTAL/8 | Medium/High | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
| Dedhia P, 2009 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 5 | medium |
| For all questions l = yes à = no or? Questions: 1. Comparable groups defined? 2. Can selection bias be excluded? 3. Is the exposure defined and is the method judging exposured? 4. Is the outcome well defined and is the method judging outcome adequate? 5. Is the outcome blind for exposure defined? 6. Is the follow-up period long enough? 7. Can selective loss-to-follow-up be excluded? 8. Are the important confounders of prognostic factors identified and is this being adapted in the design of the research or the analyses? Note: Publications with a score < 4 were excluded. | ||||||||||
| Qualitative research Author (y) | Questions (Dutch Cochrane for qualitative research) | TOTAL/ 7 | Medium/High | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| Rantz, 2013 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 4 | medium |
| For all questions 1 = yes 0 = no Questions: 1. Relevant research question? 2. Adequate method of data collection? 3. Adequate sampling ? 4. Research is controllable? 5. Concrete description of methods used for analysis? 6. Researcher perspective is described? 7. Conclusion fits qualitative research criteria? Note: Publications with a score < 4 were excluded. | |||||||||
[i] RCT’s= Randomized controlled trials, SR= Systematic review. A score < 4 is low, between 4 and 6 = medium, > 7 = high
Table 2
Overview data-extraction included studies.
| Reference | Study design | Population | Aim | Intervention and control | Outcome |
|---|---|---|---|---|---|
| Chapman, 2007 | RCT | 118 residing in nursing homes (Aged ≥75) | This study evaluated the effectiveness of advanced illness care teams (AlCTs) for nursing home residents with advanced | AICT advanced illness care teams versus usual care | Descriptive characteristics of the participants (age education, income, MMSE, Global deterioration scale, ADL-Scale, gender, marital status, race or ethnicity) * pain * depression * agitation With: * Cohen-Mansjield Agitation Inventory (CMAI) to measure agitated behaviors in elderly people * Faces Legs Activity Cry Consolability (FLACC) Behavioral Pain Scale. * Cornell Scale for Depression in Dementia (CSDD). * Pain in Advanced Dementia (PAINAD). |
| Counsell, 2007 | RCT | 951 adults 65 years or older | To test the effectiveness of a geriatric care management model on improving the quality of care for low-income seniors in primary care. | Geriatric resources for assessment and care of elders (grace) versus usual care | Main outcome measures: * medical outcomes: 36-item short-form (SF-36) scales and summary measures (PCS, physical component summary and MCS, mental component summary) * instrumental and basic activities od daily living (AHEAD-survey), also days in bed due to illness or injury * patients’ overall satisfaction * emergency department visits not resulting in hospitalization and hospitalizations. Also: Depression severity with Patient Health Questionnaire Quality of medical care with ACOVE (Assessing Care Of vulnerable Elders) |
| Denneboom, 2007 | RCT | 738 Older people (≥ 75 years) on polypharmacy (> five medicines) | To determine which procedure for treatment reviews (case conferences versus written feedback) results in more medication changes, measured at different moments in time. To determine the costs and savings related to such an intervention. | Pharmacists and GPs performed case conferences on prescription-related problems vs pharmacists provided resuits of a treatment review in GPs as written feedback. | * number of medication changes (following recommendations with clinical relevance) * costs and savings associated with the intervention at various times were calculated. |
| Phelan, 2007 | RCT | 874 patients aged 75 and older | To assess the effect or a team of geriatrics specialists on the practice style of primary care providers (PCPs) and the functioning of their patients aged 75 and older. | An interdisciplinary team of geriatrics specialists worked with patients and providers to enhance the geriatric focus of care vs usual care | * Practice level outcomes: - careful prescribing, operationalized as avoidance of prescribing high-risk medications (defined for purposes of this study as psychoactive medications); and proactive screening for selected geriatric syndromes (depression, cognitive impairment, falls). - satisfaction with the Senior Resource Team (SRT) * patient level outcomes - functional status: Arthritis Impact Measurement Scale 2F ShortForm (AIMS2-SF) - new disability in any basic ADLs (bathing, using the toilet, feeding oneself, and walking inside the home), self-rated health, psychological, well-being (assessed using the Mental Health Index-5), and hospitalizations. * death ascertainment (24-months follow-up) |
| Stenvall, 2007a | RCT | 199 patients with femoral neck fractures aged 70 years or older | To investigate the short- and long-term effects of a multidisciplinary postoperative rehabilitation programme in patients with femoral neck fracture. | Special Intervention program in geriatric ward versus conventional care in orthopedic ward | Short- and long-term effects of intervention on: * activities of daily living * mobility after hip fracture (walking ability) * consumption inpatient days after discharge * mortality |
| Stenvall, 2007b | RCT | 199 patients with with femoral neck fracture aged ≥ 70 years | This study evaluates whether a postoperative multidisciplinary, intervention program, including systematic assessment and treatment of fall risk factors, active prevention, detection, and treatment of postoperative complications, could reduce inpatient falls and fall-related injuries after a femoral neck fracture. | Special intervention program in geriatric ward vs conventional care in orthopedic ward | * postoperative fall incidence rate * postoperative complications * postoperative in-hospital stay |
| Stroke unit, 2007 | SR | Involving 6936 patients of which one subgroup age: greater than 75 years and have had a stroke | To assess the effect of stroke unit care compared with alternative forms of care for patients following a stroke. | Organized inpatient (stroke unit) care | * primaryanalysis examined: death, dependency and type requirement for institutional care * secondary outcome measures included: quality of life, patient and care satisfaction, duration of stay in hospital or institution or both |
| Young, 2007 | RCT | 490 older patients (81–90) | To compare the effect of community hospital care on Independence for older people needing rehabilitation with that of general hospital care. | community hospital rehabilitation versus usual care | * primary outcome: independence with Nottingham extended activities of daily living scale (NEADL) * secondary outcome: independence with Barthel index; for emotional, social and physical health problems the Nottingham health profile, hospital anxiety and depression scale; mortality; discharge destination; 6-months residence status and satisfaction with services. |
| Bellantanio, 2008 | RCT | 100 persons with dementia moving into two dementia-specific assisted living facilities > 70Y. | To determine whether a multidisciplinary team intervention minimizes unanticipated transitions from assisted living for persons with dementia. | Four systematic multidisciplinary assessments conducted by a special geriatric team versus usual clinical care consisted of a medical evaluation conducted by the resident’s primary care physician | Permanent relocation from assisted living to a nursing facility, emergency department (ED) visits, hospitalization, and death. * socio demographic and medical information age, sex, comorbidities, weight * Cognitive Status 30-item Folstein MMSE * Functional Status KATZ-ADL index * Behavioral Symptoms BehaveAD Rating scale |
| Bergrenn, 2008 | RCT | 199 patients with femoral neck fracture aged ≥ 70 years | This study evaluates whether a postoperative multidisciplinary, multifactorial fall-prevention program performed by a geriatric team that reduced inpatient falls and injuries had any continuing effect after discharge. The intervention consisted of staff education, systematic assessment and treatment of fall risk factors and vitamin D and calcium supplementation. | Special intervention program in geriatric ward versus conventional care in orthopedic ward | Comparing falls and new fractures between intervention and control. * basic characteristics during hospitalization, at 4 months and 12 months. * medical data * social data * including morbidity and mortality, the occurrence of falls.* occurrence of falls were registered from the records (obliged to document) |
| Boult, 2008 | (cluster) RCT | 904 multimorbid older patients (66-106y) | To assess whether GC can improve the quality of health care for this population, “Guided Care" (GC) was designed to enhance quality care by integrating a registered nurse, intensively trained in chronic care, into primary care practices to work with physicians in providing comprehensive chronic care to 50–60 multimorbid older patients. | Guided Care versus usual care | * Patients ‘heaith and functional status, quality of health care, and satisfaction with health care. * Patient Assessment of Chronic Illness Care (PACIC) * Satisfaction with 11 aspects of care. * The amounts of time spent on five tasks necessary for managing chronically ill patients. * Whether the physician knows six elements of information. * Whether four care coordination processes occur. * Elements of information and care coordination were derived from the Primary Care Assessment Tool (PCAT). |
| Gates, 2008 | SR | Involving 5874 elderly | To evaluate the effectiveness of multifactorial assessment and intervention programmes to prevent falls and injuries among older adults recruited to trials in primary care, community, or emergency care settings. | Fall prevention interventions versus standard care, no fall prevention intervention | * no of fallers * fall related injuries * recurrent falls * admission to hospital attendance at emergency departments * attendance at doctor’s surgery * death * move to institutional care |
| Unutzer, 2008 | RCT | 551, 60 years or older patients with major depression, dysthymia or both | To determine the long-term effects on total healthcare costs of the Improving Mood: Promoting Access to Collaborative Treatment (IMPACT) program for late-life depression compared with usual care. | Collaborative care intervention (IMPACT) vs usual care | cost outcome data |
| Counsell, 2009 | RCT | 951, low lncome seniors aged 65 or older | To provide, from the healthcare delivery system perspective, a cost analysis of the Geriatric Re-sources for Assessment and Care of Elders (GRACE) intervention, which is effective in improving quality of care and outcomes. | Home-based care management for 2 years versus usual care. | * chronicen preventive care costs * acute care costs * total costs in the full sample (* predefined high-risk and low risk groups) |
| Dedhia, 2009 | pre-post design ‘cohort’ | 422 patients 65y> admitted to the hospitalist services | To study the feasibility and effectiveness of a discharge planning intervention | Intervention period: October-April 2007 1. admission form with geriatric cues 2. facsimile to the primary care 3. inteicisciplinary worksheet to identify barriers to discharge 4. pharmacist-physician collaborative medication reconciliation 5. predischarge planning appointments vs control period January–May2006 | Thirty-day readmission and return to emergency department rates and patient satisfaction with discharge. * Katz * self-perceived health status * ED visits * need for hospital read mission * patient satisfaction with Coleman’s Care Transition Measures (discharge planning intervention: * follow-up within 1 week of discharge * follow-up at 30 days after discharge Effect of the intervention across the three hospital sites) |
| Handoll, 2009 | SR | Involving 2498 elderly | To examine the effects of multidisciplinary rehabilitaion, in either inpatient or ambulatory care settings, for older patients with hip fracture. | Interventions with treatments in a multidisciplinary rehabilitation program (supervised by geriatrician or rehabilitation physician/clinician) versus usual care | Primary outcome: * ‘poor outcome’ defined as death or deterioration of functional status leading to increased dependency in the community or admission to institutional care. Secondary outcomes: * Morbidity * Length of stay in hospital ano hospital readmission * Carer burden * Costs |
| Hogg, 2009 | RCT | 241 adults 50 and older and considered to be at risk of experiencing adverse health outcomes | To examine whether quality of care (QQC) improves when nurse practitioners and pharmacists work with family physicians in community practice and focus their work on patients who are 50 years of age and older and considered to be at risk of experiencing adverse health outcomes. | Anticipatory and Preventive team care (APT care) from a collaborative multidisciplinary team versus usual care from family physicians | Main outcome measure: * chronic disease management score secondary outcomes: * Intermediate clinical outcomes (mean hemoglobine A1c blood pressure). * Quality of preventive care * QOL with the SF-36 |
| Van Leeuwen, 2009 | Multisite RCT | 906 Young-old (60-74y) and old-old patients (≥ 75y) | To compare the clinical outcome of young-old patients and old-old patients who received collaborative care management for depression. | Patient have access for 12 months to a depression clinical specialist who coordinated depression care with their primary care physician. | Comparison between groups on ‘process of care’ type of treatment and level of care received. Clinical outcomes compared between groups: Symptom checklist (SCL)-20 depression score, treatment response (≥ 50% decrease SCL-20 score). |
| Boyd, 2009 | Cluster RCT | 904 of 65 and older and ‘highrisk patients’ | To evaluate the effects of “GuidedCare” on patient-reported quality of chronic illness care. | ‘Guided care’ integrate a nurse trained in chronic care into a primary care practice to work with 2-5 physicians in providing comprehensive chronic care to 50-60 multi-morbid older patients. | Patient Assessment of Chronic Illiness Care (PACIC)survey by telephone: (Experience of chroniccare) * goal setting, coordinated care, decision support, problem solving, patient activation, aggregate quality |
| Wu, 2010 | RCT | 74 long-term care facility resident (aged >70y) | To evaluate the clinical effectiveness of integrated interdisciplinary team care for severely disabled LTCF residents in Taiwan, so to promote better quality of care in this setting. | Integrated care model versus traditional model of care | Physical function, nutritional status, several quality indicators (Quality indicators included unplanned feed tube replacement, unplanned urinary catheter replacement, emergency department visit, hospitalizations, and incidence of urinary infections, pneumonia, and pressure sore.) |
| Cameron, 2010 | SR | Involving 25422 elderly | To present the best evidence for effectiveness of programs designed to reduce the incidence of falls in older people in nursing facilities and hospitals. | Any intervention to reduce falls vs usual care or placebo | Primaryoutcome: * number of falls * number of people who fall Secondary outcome: * severity of falls * fractures and deaths |
| Markle-Reid, 2010 | RCT | 109 elderly 75y and older | This study determined the effects and costs of a multifactorial, interdisciplinary team approach to falls prevention. | Multifactorial, interdisciplinary team approach compared with usual home care services | * number of falls * fall risk factors (number of slips and trips, functional health status and related quality of lite, nutritional status, gait and balance, depressive symptoms, cognitive function, and confidence in performing ADLS) * the six-month costs of use health services with a multifactorial, interdisciplinary team approach |
| Respect team, 2010 | Multiple interrupted time-series | 551 Aged ≥ 75 | To estimate the effectiveness of pharmaceutical care for older people, shared between GPs and community pharmacists in the UK, relative to usual care. | Pharmaceutical care, shared between GPs and community pharmacists in the UK relative to usual care (acted as own control) | Primary outcome: UK Mecication Appropriateness Index (UK-MAI) Secondary outcomes: * quality of life (SF-36) * health utility measured by the EQ-5D * costs of pharmaceutical care * associated health care to the NHS were also collected |
| Bryant, 2011 | RCT | 269 65 years and older on five or more prescribed medicines. | The objective was to determine whether involvement of community pharma-cists undertaking clinical medication reviews, working with general practitioners, improved medicine-related therapeutic outcomes for patients. | Community pharmacists undertook a clinical medication review (Comprehensive Pharmaceutical Care)and met with the patient’s general practitioner to discuss recommendations about possible medicine changes versus usual care. | * Ouality of Life (SF-36) * Mecication Appropriateness Index. |
| Ryvicker, 2011 | RCT | 3290 older chronically ill patients served by a large homecare organization | To describe (1) the impact of a guality improvement initiative (QI) on functional outcomes of older, chronically ill patients served by a large homecare organization; and (2) key implementation challenges affecting intervention outcomes. | A quality improvement initiative on functional outcomes of older, chronically ill patients served by a large homecare organization vs usual care. | Primary outcomes: changes in ADL on patient level (Notes from observations and from semi-structured interviews about how the intervention was implemented during phase 1 and phase 2) |
| Mudge, 2012 | Pre-planned subgroup analysis of controlled trial | 1004 aged over 65 and admitted from residential aged care | To identify the impact of an interdisciplinary care model on medical inpatients admitted from residential aged care (RAC). | Interdisciplinary care model on medical inpatients admitted form residential aged care (RAC) | In-hospital mortality for patient from RAC and 6-month mortality compared to patients from the community. |
| Berglund, 2013 | RCT | 161 age 80 and older or 65–79 with minimum 1 chronic illness and a need for assistance in ADL | To analyse frail older people’s views of quality of care when receiving a comprehensive continuum of care intervention, compared with those of people receiving the usual care (control group). | Data-collection period: January 2009-October 2011. A comprehensive continuum of care intervention versus usual care. (The intervention included early geriatric assessment case management, interprofessional collaboration, support for relatives and organising of care-planning meetings in older people’s own homes.) | Poeple’s views on quality of care with questionnaire. Scales and items contained: functionl ability, illness, life satisfaction, health, medication and quality of care. |
| Nazir, 2013 | SR | Involving > 33015 elderly | To study the impact of interdisciplinary interventions on health outcomes of NH residents and to document features of successful interventions including those that used formal teams. | RCT’s, NH setting or residential care facilities, team-based interventions and outcomes that were facility or resident based. | (impact on) Resident outcomes as reported in the included studies. |
| Rantz, 2013 | Qualitative research (during randomized two group repeated-measures design) | Nursing homes (72 professionals) | The purpose of this article is to discuss a qualitative analysis of field notes of observational data of the nursing homes that participated in a two-year intervention to improve quality of care, resident outcomes, and organizational working conditions (Rantz et al., 2012). The focus of this analysis was on the use of team and group processes by the nursing home staff in quality improvement efforts. | Facilities in resident outcome “need of improvement” received multilevel intervention designed to help them (quality improvement methods and team and group process for direct-care decision-making…) | The focus of this analysis was on the use of team and group processes by the nursing home staff in quality improvement efforts. Description of behavior of staff in intervention facilities during a RCT for improving quality of care and subsequently improving resident outcomes in nursing homes. |
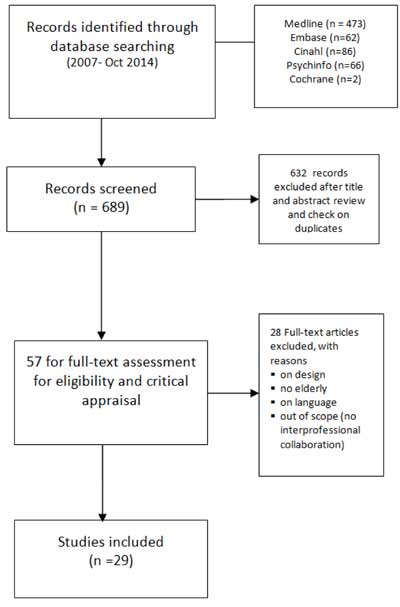
Figure 1
Flowchart results literature search.
Table 3
Overview of the outcome indicators on interprofessional collaboration.
| Reference | Collaboration | Patient level outcomes | Costs | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| KE | ID | spr | Spa | QOHC | P | Fl | QOL | 1 | D | B | T | LOSH | M | PR | ||
| Chapman 2007 | NS | S | NS | NS | S | |||||||||||
| Counsell 2007 | S | S | NS | S | ||||||||||||
| Denneboom 2007 | S | |||||||||||||||
| Stenvall 2007a | S | NS | ||||||||||||||
| Stenvall 2007b | S | |||||||||||||||
| Phelan 2007 | NS | NS | NS | NS | ||||||||||||
| Young 2007 | S | S | ||||||||||||||
| Bellantonio 2008 | NS | |||||||||||||||
| Bergrenn 2008 | NS | |||||||||||||||
| Bonit 2008 | S | S | S | |||||||||||||
| Gates 2008 | NS | |||||||||||||||
| Unützer 2008 | NS | |||||||||||||||
| Boyd 2009 | S | S | S | |||||||||||||
| Counsell 2009 | S | |||||||||||||||
| Dedhia2009 | NS | |||||||||||||||
| Handoll 2009 | S | NS | NS | NS | NS | NS | ||||||||||
| Hogg 2009 | S | S | ||||||||||||||
| Stroke Unit 2009 | NS | S | S | S | ||||||||||||
| Van Leeuwen 2009 | S | |||||||||||||||
| Cameron 2010 | NS | |||||||||||||||
| Markle-Reid2010 | S | NS | ||||||||||||||
| Respect team 2010 | NS | NS | ||||||||||||||
| Wu 2010 | NS | |||||||||||||||
| Bryant 2011 | S | S | ||||||||||||||
| Ryvicker2011 | NS | S | ||||||||||||||
| Mudge 2012 | S | S | ||||||||||||||
| Berglund 2013 | S | |||||||||||||||
| Nazir 2013 | S | S | ||||||||||||||
| Rantz 2013 | NS | |||||||||||||||
[i] KE = Key elements
ID = Involved disciplines
SPr = Satisfaction professionals
Spa = Satisfaction patients
QOHC = Quality of Health Care
P = Pain
FI = Fall incidence
QOL = Quality of Life
D = Depression
I = Independence
B = Behaviour
T = Transtions
LOSH = Length of Stay in Hospital
M = Mortality
PR = Period of Rehabilitation
NS = not significant
