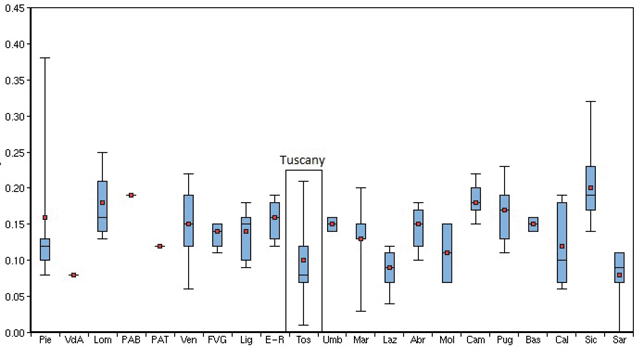
Figure 1
Age- and gender-adjusted hospitalization rates for diabetes-related lower limb amputations (major and minor) per 100,000 residents in the Italian Regions and Provinces – 2012. Source: National Outcome Evaluation Program – National Agency for Regional Health Services.
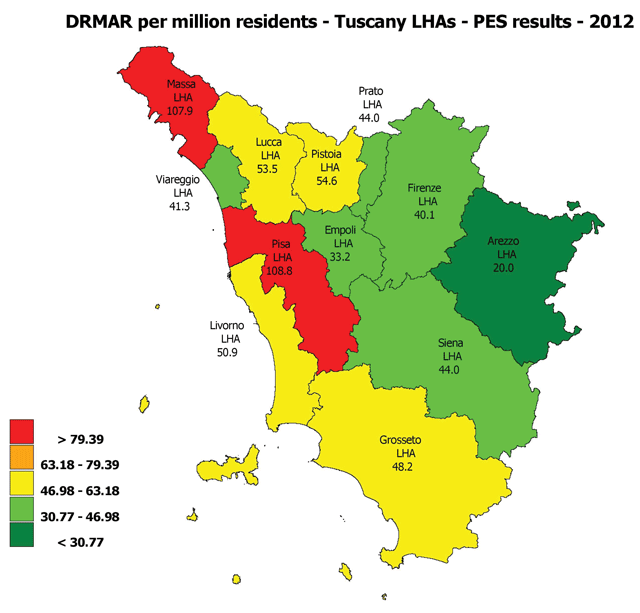
Figure 2
Diabetes-related lower limb major amputation rate per million residents – MeS-Lab Tuscany PES results – 2012. Source: MeS-Lab.
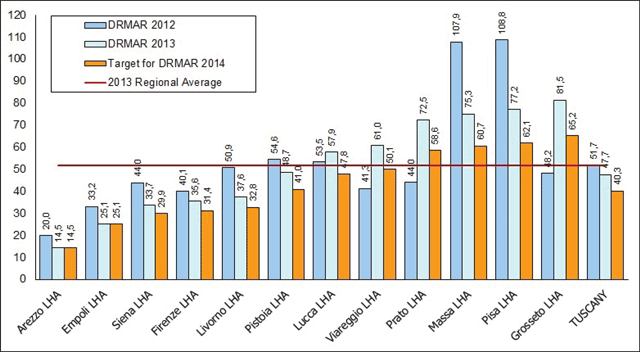
Figure 3
LHA DRMAR targets in Tuscany for 2014. Source: MeS-Lab.
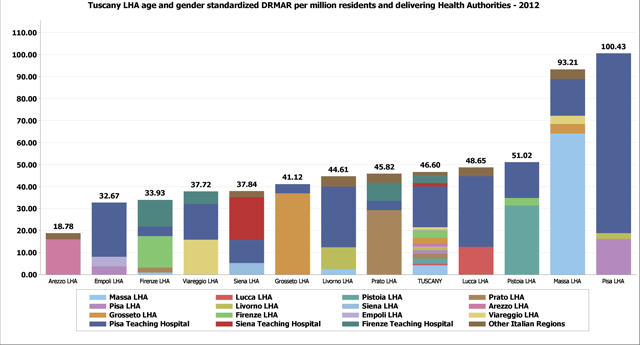
Figure 4
Age and gender standardized diabetes-related lower limb major amputation rate per million residents in Tuscany, 2012. Details for the delivering Health Authority. Source MeS-Lab.
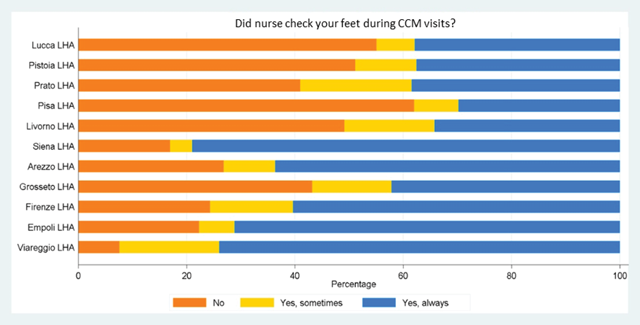
Figure 5
Diabetic patient experience regarding foot check-ups in Tuscan LHAs – Survey 2012. Source: MeS-Lab.
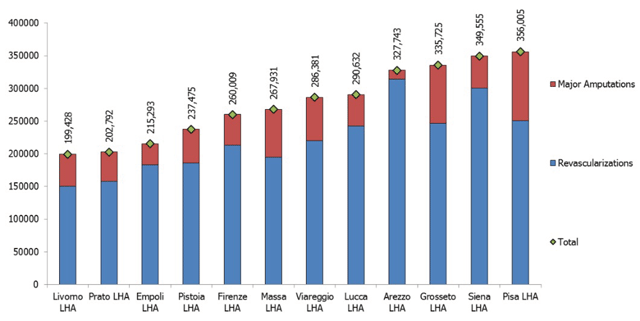
Figure 6
Estimated LHA expenditure (DRG) of hospitalizations for diabetes-related revascularizations and lower limb major amputations per 100.000 residents – Average of the four-year period between 2009 and 2012. Source: MeS-Lab.
Table 1
Summary of the organizational mapping.
| Area | Mapping results |
|---|---|
| Screening, admissions and visits | Professionals pointed out coordination problems with Primary Care (PC) regarding the prompt identification and management of ulcers/complications, leading to late diagnoses. Patients were therefore often admitted to the outpatients clinics with severe conditions and without previous DF assesment by their GPs. This was confirmed by the survey presented in Figure N.5.: foot check-ups by PC professionals were not a comman practice. Outpatient clinics also differed in the scheduling procedures for visits and diagnostics exams. Moreover, some HAs did not schedule dedicated slots in their radiology departments in agreement with the diabetology departments. |
| Revascularization procedures | The organization of this phase greatly differed between HAs. Some LHAs did not have catherization labs to perform lower-limb revascularization procedures so they had to refer their patients to other HAs. This implied a greater need for coordination among these providers. Other HAs provided some schedule hours during the week for the revascularization of lower limbs. In some HAs, revascularizations were usually performed without involving the diabetologists. |
| Surgery | In some HAs, interventions and follow-up treatments were often planned without involving the diabetologists. Lack of coordination occured both before and after surgery. Only in some HAs, diabetologists directly performed basic and minor surgical procedures. |
| Urgent path | Some professionals identified barriers to flexible and “fast track”, access, exams, revascularization procedures and interventions for patients with urgent needs because of a lack of coordination with other professionals. |
| Follw-up and continuity of care | Communication with PC professionals was also considered a critical aspect after discharges with regards to the management of lesions, wounds, ulcers and specific medications. |
| Education for patients and caregivers | Only in some organizations, educations for the prevention and treament of ulcers and lesions was provided for both individuals and groups of patients and caregivers. PC professionals were often not well-trained in preverting and recognizing DF problems and providing appropriate education for patients and caregivers. |
| Training professionals | Perodic educational meeting on prevention, treatment and team building, especially between diabetologists and PC professionals, were not held in every organization. These meetings should be held more in large hospitals (such as THs) and in those areas where the care path is fragmented among LHAs and THs. |
| Information Systems | The development and implementation of information systems are very different in each organization. Only some HAs quickly collected comprehensive information about their patients over time and easily shared them with other departments. |
Table 2
| Categories of variation in medical care | Actions | |
| Effective Care of an individual service or procedure (e.g. minimal volumes for specific surgical precedures to ensure patients’ safety and better outcomes) | Refers to services of proven values and without significant tradeoffs: the benefits of these services outweigh the risks | Reduction |
| Effective care of an Integrated Care pathway | Refers to services whose variation is due to a lack of integration throught the entire care pathway | Reduction |
| Supply-sensitive care | Represents service for which human and the availability of technical resources (e.g. physicians, hospital beds) strongly influence the amount of care delivered | Reduction |
| Preference-sensitive care | Comprises care for conditions that have more than one treatment option, each with its own benefits and tradeoffs | Follow patient preferences |
