Table 1
Baseline characteristics of patients with and without SMuRFs – univariable analysis.
| VARIABLE | TOTAL (n = 2379) | NO SMURF (n = 605) | ≥1 SMURF (n = 1774) | P VALUE |
|---|---|---|---|---|
| Age | ||||
| (Mean age ± SD) | 56.13 ± 12.37 | 57.44 ± 13.95 | 55.68 ± 11.74 | <0.001 |
| <60 years | 1392 (58.5%) | 323 (53.4%) | 1069 (60.3%) | 0.003 |
| ≥60 years | 987 (41.5%) | 282 (46.6%) | 705 (39.7%) | |
| Sex | ||||
| Male | 1823 (76.6%) | 441 (72.9%) | 1382 (77.9%) | 0.012 |
| Female | 556 (23.4%) | 164 (27.1%) | 392 (22.1%) | |
| Risk Factors | ||||
| Hypertension | 810 | 0 | 810 | |
| Diabetes | 933 | 0 | 933 | |
| Dyslipidemia | 34 | 0 | 34 | |
| Current tobacco user | 834 | 0 | 834 | |
| Former tobacco user | 152 (6.4%) | 63 (10.4%) | 89 (5.0%) | <0.001 |
| Alcohol | 838 (35.2%) | 113 (18.7%) | 725 (40.9%) | <0.001 |
| F/h/o CAD | 45 | 15 (2.5%) | 30 (1.7%) | 0.219 |
| Sleep duration per day | ||||
| Duration (mean ± SD) | 7.65 ± 0.89 | 7.67 ± 0.86 | 7.64 ± 0.90 | 0.439 |
| ≤ 6 hours | 300 (12.6%) | 72 (11.9%) | 228 (12.9%) | 0.810 |
| >6 to ≤ 7 hours | 364 (15.3%) | 88 (14.5%) | 276 (15.6%) | |
| >7 to ≤ 8 hours | 1570 (66%) | 411 (67.9%) | 1159 (65.3%) | |
| >8 to ≤ 9 hours | 127 (5.3%) | 29 (4.8%) | 98 (5.5%) | |
| >9 hours | 18 (0.8%) | 5 (0.8%) | 13 (0.7%) | |
| CKD | 26 (1.1%) | 5 (0.8%) | 21 (1.2%) | 0.465 |
| CVA | 42 (1.8%) | 4 (0.7%) | 38 (2.1%) | 0.017 |
| COPD | 21 (0.9%) | 6 (1%) | 15 (0.8%) | 0.740 |
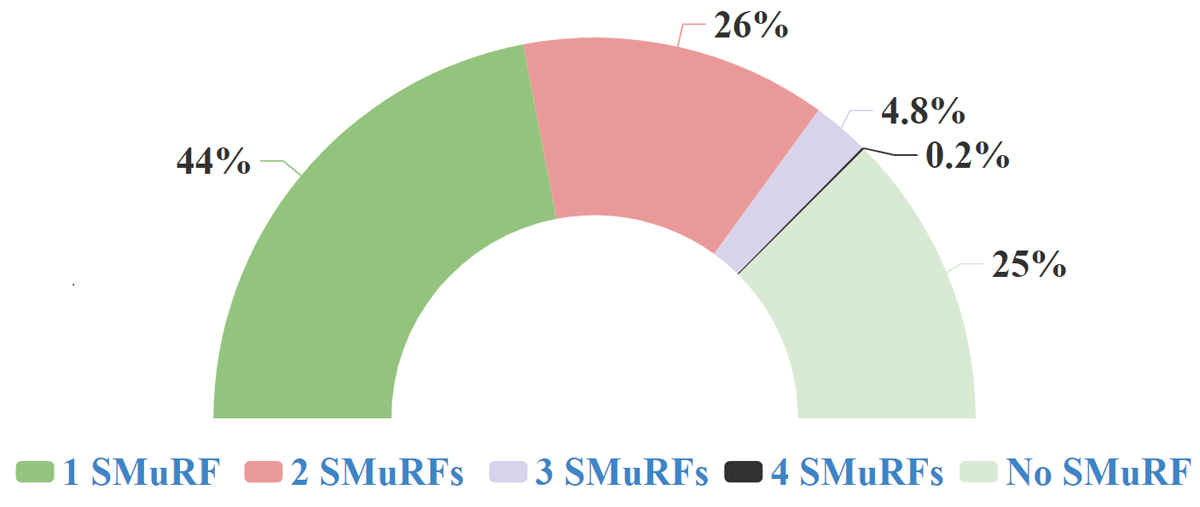
Figure 1
Number of SMuRFS identified in the enrolled patients.
Note: SMuRF: Standard modifiable cardiovascular risk factor.
Table 2
Clinical presentation and reperfusion strategies.
| PARAMETER ANALYZED | TOTAL (n = 2379) | NO SMURF (n = 605) | ≥1 SMURF (n = 1774) | P VALUE |
|---|---|---|---|---|
| Time Window (symptom onset to presentation at hospital) | ||||
| Time window (hours) | 13.23 ± 17.47 | 13.08 ± 17.25 | 13.28 ± 17.25 | 0.809 |
| <6 hours | 1234 (51.9%) | 313 (51.7%) | 921 (74.6%) | 0.794 |
| 6–12 hours | 534 (22.4%) | 143 (23.6%) | 391 (22%) | |
| 12–24 hours | 315 (13.2%) | 79 (13.1%) | 236 (13.3%) | |
| >24 hours | 296 (12.4%) | 70 (11.6%) | 226 (12.7%) | |
| Location of infarction | ||||
| Anterior | 1374 (57.8%) | 379 (62.6%) | 995 (56.1%) | 0.005 |
| Non anterior | 1005 (42.2%) | 226 (37.4%) | 779 (43.9%) | |
| Killip Class | ||||
| Class I | 1773 (74.5%) | 466 (77.0%) | 1307 (73.6%) | 0.105 |
| Class II, III & IV | 606 (25.5%) | 139 (23.0%) | 467 (23.6%) | |
| Left ventricular ejection fraction | ||||
| Mean EFa ± SDb | 46.1 ± 8.78 | 46.13 ± 8.9 | 46.10 ± 8.45 | 0.938 |
| ≤ 40% | 676 (28.4%) | 163 (26.9%) | 513 (28.9%) | 0.643 |
| 41–54% | 1260 (53.0%) | 326 (53.9%) | 934 (52.6%) | |
| >54% | 443 (18.6%) | 116 (19.2%) | 327 (18.4%) | |
| Right ventricular function | ||||
| TAPSEc mean ± SD | 17.81 ± 2.46 | 18.05 ± 2.3 | 17.74 ± 2.51 | 0.03 |
| TAPSE < 17 | 297 (12.5%) | 57 (9.4%) | 240 (13.5%) | 0.008 |
| Primary reperfusion strategyg | ||||
| Fibrinolysis | 1242 (52.2%) | 320 (52.9%) | 922 (52%) | 0.852 |
| SKd | 1097 (46.1%) | 278 (46%) | 819 (46.2%) | |
| TNKe | 121 (5.1%) | 35 (5.8%) | 86 (4.8%) | |
| Reteplasef | 24 (1.0%) | 7 (1.2%) | 17 (1.0%) | |
| Primary PCI | 238 (10%) | 63 (10.4%) | 175 (9.9%) | |
| Neither | 899 (37.8%) | 222 (36.7%) | 677 (38.2%) | |
| Overall Reperfusion Strategyh | ||||
| Primary/PI PCI | 354 (14.9%) | 90 (14.9%) | 264 (14.9%) | 0.961 |
| Fibrinolysis only (no PCI) | 1035 (43.5%) | 266 (44.0%) | 769 (43.3%) | |
| Neither | 990 (41.6%) | 249 (41.2%) | 741 (41.8%) | |
[i] aEF – Ejection fraction; bSD: Standard deviation; cTAPSE – Tricuspid annular plane systolic excursion; dSK- Streptokinase; eTNK tPA -Tenecteplase; fPCI-Percutaneous coronary intervention; gPrimary reperfusion strategy- The type of reperfusion therapy offered at admission to the hospital; hOverall reperfusion strategy: The reperfusion therapy offered during the entire hospital stay.
Table 3
Angiographic analysis. Analysis of angiographic findings of the 1089 patients who underwent coronary angiogram.
| PARAMETER | TOTAL (n = 1089) | NO SMURF (n = 270) | ≥1 SMURF (n = 819) | P VALUE |
|---|---|---|---|---|
| Culprit Lesions | ||||
| LMCA | 3 (0.2%) | 1 (0.4%) | 2 (0.2%) | 0.605 |
| LAD | 554 (50.9%) | 145 (53.7%) | 409 (49.9%) | |
| LCX | 51 (4.7%) | 8 (3.0%) | 43 (5.3%) | |
| RCA | 218 (20.0%) | 55 (20.4%) | 163 (19.9%) | |
| Unspecified | 263 (24.2%) | 61 (22.6%) | 202 (24.7%) | |
| Single Vessel Disease | 508 (46.6%) | 127 (47%) | 381 (46.5%) | 0.883 |
| Multivessel Disease | 581 (53.4%) | 143 (53%) | 438 (53.5%) | |
[i] LMCA-Left main coronary artery; LAD- Left anterior descending artery; LCX- Left circumflex coronary artery; RCA-Right coronary artery.
Table 4
In-hospital and 12 months Outcome – univariable analysis. [Univariate analysis of the difference in the outcome parameters between the SMuRFless and the SMuRF group, expressed as proportions, P value and odds ratio].
| PARAMETERS | TOTAL (n = 2379) | NO SMURF (n = 605) | ≥1 SMURF (n = 1774) | P VALUE | UNADJUSTED ODDS RATIO (95% CI) |
|---|---|---|---|---|---|
| In-Hospital Outcome | |||||
| In hospital Mortality | 265 (11.1%) | 65 (10.7%) | 200 (11.3%) | 0.720 | 0.96 (0.77–1.20) |
| Any complications | 739 (31.1%) | 176 (29.1%) | 563 (31.7%) | 0.225 | 0.91 (0.78–1.06) |
| Arrhythmic complications | 589 (24.8%) | 132 (21.8%) | 457 (25.8%) | 0.052 | 0.85 (0.72–1.0) |
| Tachyarrhythmia | 387 (17.1%) | 84 (13.9%) | 303 (17.1%) | 0.066 | 0.83 (0.68–1.02) |
| Bradyarrhythmia | 207 (8.7%) | 49 (8.1%) | 158 (8.9%) | 0.543 | 0.923 (0.72–1.12) |
| Mechanical Complications | 45 (1.9%) | 15 (2.5%) | 30 (1.7%) | 0.219 | 1.32 (0.87–2.0) |
| Ventricular septal rupture | 37 (1.6%) | 13 (2.1%) | 24 (1.4%) | 0.17 | 1.39 (0.89–2.12) |
| Cardiogenic Shock | 229 (9.6%) | 55 (9.1%) | 174 (9.8%) | 0.605 | 0.94 (0.74–1.12) |
| Right ventricular dysfunction | 297 (12.5%) | 57 (9.4%) | 240 (13.5%) | 0.008 | (0.73 (0.57–0.93) |
| Follow up Outcome | |||||
| Discharged alive | 2114 (88.9%) | 540 (89.3%) | 1574 (88.7%) | 0.720 | 0.96 (0.77–1.20) |
| Lost to follow up | 344 (16.3%) | 84 (15.6%) | 260 (16.5%) | 0.601 | 0.93 (0.71–1.22) |
| Post discharge mortality (n = 2035) | 194 (9.5%) | 51 (9.8%) | 143 (9.4%) | 0.818 | 1.03 (0.80–1.32) |
| One -year mortality (n = 2035) | 459 (22.6%) | 116 (22.3%) | 343 (22.7%) | 0.854 | 0.98 (0.82–1.12) |
Table 5
Sub group analysis of In Hospital Mortality and SMuRF less ness. [Role of the baseline features in modulating the influence of SMuRFless-ness on in-hospital mortality].
| OVERALL | ≥ 1 SMURF | NO- SMURF | OR | 95% CI | P-VALUE FORINTERACTION | |||
|---|---|---|---|---|---|---|---|---|
| ALIVE N (%) | DEATH N (%) | ALIVE N (%) | DEATH N (%) | |||||
| Whole group | 1574 (88.7) | 200 (11.3) | 540 (89.3) | 65 (10.7) | 0.947 | 0.704–1.274 | 0.720* | |
| Age | <60 | 996 (93.2) | 73 (6.8) | 308 (95.4) | 15 (4.6) | 0.690 | 0.341–1.399 | 0.304 |
| >60 | 578 (82.0) | 127 (18.0) | 232 (82.3) | 50 (17.7) | ||||
| Sex | Male | 1248 (90.3) | 134 (9.7) | 405 (91.8) | 36 (8.2) | 0.788 | 0.403–1.542 | 0.487 |
| Female | 326 (83.2) | 66 (16.8) | 135 (82.3) | 29 (17.7) | ||||
| Ex Smoking | Yes | 79 (88.8) | 10 (11.2) | 60 (95.2) | 3 (4.8) | 2.466 | 0.583–10.441 | 0.220 |
| No | 1495 (88.7) | 190 (11.3) | 480 (88.6) | 62 (11.4) | ||||
| AWMI | Yes | 873 (87.7) | 122 (12.3) | 337 (88.9) | 42 (11.1) | 1.185 | 0.576–2.438 | 0.645 |
| No | 701 (90.1) | 78 (10.0) | 203 (89.8) | 23 (10.2) | ||||
| RVD | Yes | 188 (78.3) | 52 (21.7) | 45 (78.9) | 12 (21.1) | 1.079 | 0.425–2.742 | 0.873 |
| No | 1386 (90.4) | 148 (9.6) | 495 (90.3) | 53 (9.7) | ||||
| CAR | Yes | 355 (77.7) | 102 (22.3) | 104 (78.8) | 28 (21.2) | 1.129 | 0.584–2.184 | 0.718 |
| No | 1219 (92.6) | 98 (7.4) | 436 (92.2) | 37 (7.8) | ||||
[i] * This is not a p value of interaction. This is the P value of differences between ≥ 1 SMuRF group and SMuRF less group in the entire study cohort. AWMI Anterior wall Myocardial infarction; RVD Right Ventricular dysfunction; CAR Cardiac arrhythmias.
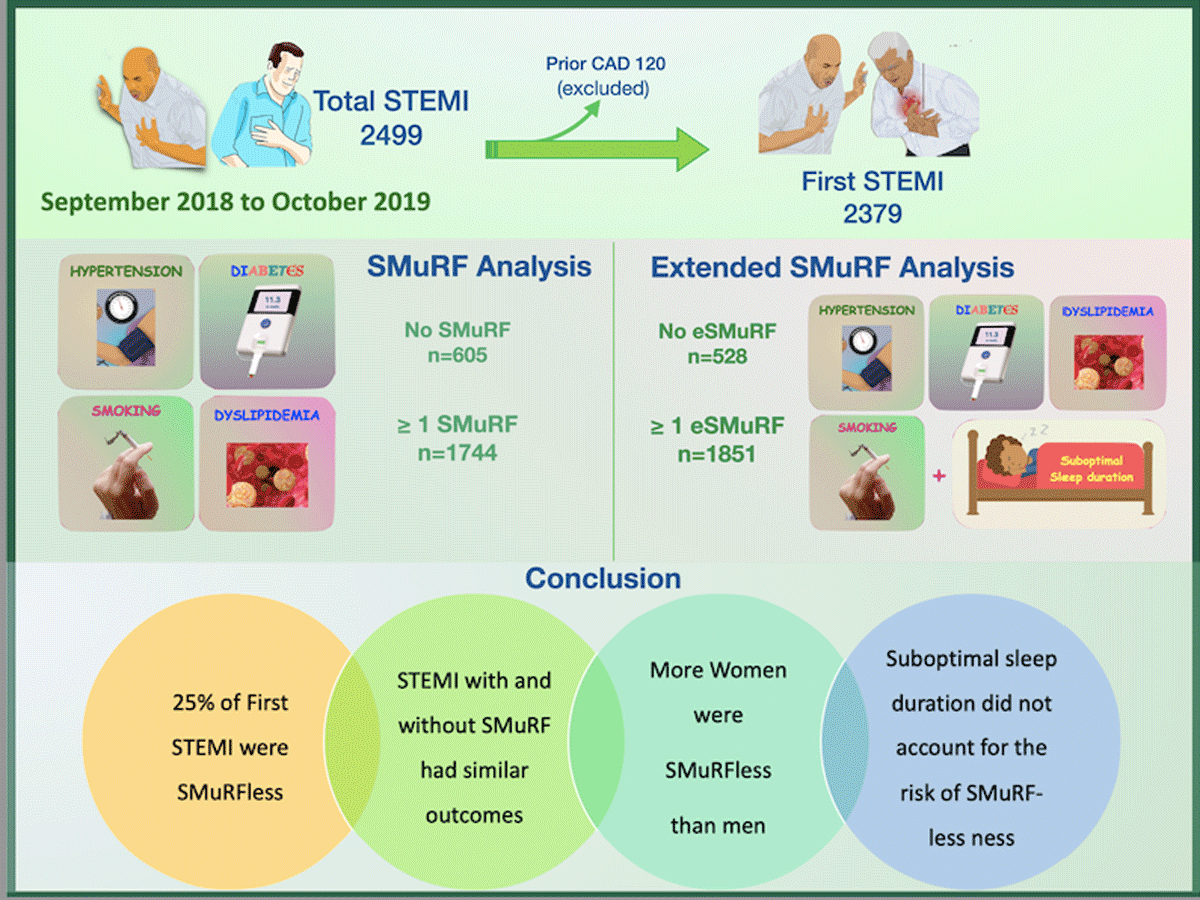
Figure 2
Central illustration-methods and outcome of the study.
Note: SMuRF—Standard modifiable cardiovascular risk factor; eSMURF—extended standard modifiable cardiovascular risk factor; STEMI—ST segment elevation myocardial infarction.
| 1 | STEMI | : | ST segment Elevation Myocardial Infarction |
| 2 | SMuRF | : | Standard Modifiable Cardiovascular Risk Factors |
| 3 | eSMuRF | : | Extended Standard Modifiable Cardiovascular Risk Factors |
| 4 | CAD | : | Coronary Artery Disease |
| 5 | PCI | : | Percutaneous Coronary Intervention |
| 6 | COPD | : | Chronic obstructive pulmonary disease |
| 7 | CVA | : | Cerebro vascular accident |
| 8 | CKD | : | Chronic Kidney Disease |
| 9 | LAD | : | Left Anterior Descending Artery |
| 10 | LMIC | : | Low-and middle-income countries |
