Introduction
Citizen science has great potential to contribute to society and to innovative research. It has come to be understood as an approach that involves citizens in knowledge production, valuing their multiple capacities to document, reflect on, and act on pressing societal issues, and generates outcomes and impacts that are better suited to specific local conditions. Numerous authors have defined and identified the range of approaches that may be labelled as citizen science (Haklay et al. 2021a; Haklay et al. 2021b; Eitzel et al. 2017; Auerbach et al. 2019; Haklay 2013; Shirk et al. 2012; Bonney et al. 2009). Similarly, citizen science has been used in a wide range of academic disciplines, a growth in part facilitated by the internet and the advancement of digital tools (Vohland et al. 2021). Contemporary debates in the field of citizen science are careful to resist a narrow definition because any exclusionary approach will necessarily fail to address the challenge of accommodating considerable heterogeneity within the field (Auerbach et al. 2019). In this way, terminology in citizen science is important (Eitzel et al. 2017), especially considering the increasingly international, multicultural, multi-disciplinary, and multi-lingual interest in citizen science (Vohland et al. 2021).
Even though citizen and patient engagement in health research has a long tradition, citizen science is a relatively underdeveloped branch in the health domain (Rowbotham et al. 2019; Wiggins and Wilbanks 2019; King et al. 2019; Borda et al. 2019; ICPHR 2013; Den Broeder 2017; Den Broeder 2018; English 2018; Bonhoure et al. 2023, Cigarini et al. 2018). Participation in the health domain has long focussed on including patients in agenda-setting for research (Abma and Broerse 2010), or in shared decision-making in the process of health care (Elwyn et al. 2012). A number of approaches have emerged over the years to include patients in various forms of health research, such as participatory health research (PHR; Wright and Kongats 2018), patient and public involvement and engagement (PPI or PPIE; Baines and Regan de Bere 2018; NIHR 2021; Carlton et al. 2022), patient and public patient-oriented research (POR; Rouleau et al. 2018), community-based participatory research (CBPR; Wallerstein et al. 2018), patient engagement (PCORI 2018), and patient innovation (Patient Innovation 2021). The domains in health in which citizen science may play out are again very diverse, including public health (Den Broeder 2018), environmental health (Perelló et al. 2021), biomedical health (Guerrini et al. 2022), and health equity (Rosas et al. 2022), and spanning applied research (Lewis and Leibrand 2016) to fundamental research (Koepnick et al. 2019). The level of involvement that citizens and patients may have in health research may vary across any participation scale adopted (Arnstein 1969; Shirk et al. 2012).
Yet, in recent years, a new generation of citizen and patient involvement in health research is growing (Turbe et al. 2021; Hammel et al. 2021), and new labels are emerging, such as participant-led research (Vayena et al. 2016), patient science (Heyen et al. 2022), do-it-yourself medicine (Wexler 2022), and personal science (Wolf and De Groot 2020). This new generation aims for a more substantial, if not decisive role of citizens in the process of biomedical research. Again, roles can be very different: from contributors of data in crowdsourced modes of citizen science (Swan 2012; Canas et al. 2021) to principal investigators (Lewis and Leibrand 2016). At the same time, a substantial amount of citizen engagement with health research occurs off the beaten institutional track (Wiggins and Wilbanks 2019). Some of it emerges in the shape of “experiential knowledge,” acquired in the process of dealing with a disease or the healthcare sector in general, and narrated in self-published documents (Frank 2013; Van de Bovenkamp et al. 2020).
In whatever form patient and citizen participation in the health research domain presents itself, and in the light of the growing availability of digital solutions that enable real-time and home-based data collection, citizen involvement is expected to revolutionise the way innovation takes place in the health care ecosystem (Ciasullo et al. 2022). An example of innovative applications of citizen science in health can be seen with initiatives that sprang up to tackle the COVID-19 pandemic, such as seven projects indexed in the SciStarter platform. Furthermore, patients and citizens claim and explore more demanding roles and capacities (Wexler 2022), and challenge current health research (Remmers et al. 2023). Beyond handbooks of PPIE in more conventional health research (NIHR 2021; INVOLVE 2017), at present, there is no clear overview of the main challenges that citizen science initiatives in the health domain are facing, nor of what particularities distinguish health-related citizen science from citizen science in other domains.
In this paper, we describe the attempt of the European Citizen Science Association (ECSA) Working Group (WG) “Citizen Science for Health” (CS4H) to start filling this knowledge gap. ECSA is a membership organisation set up in 2014 to increase the democratisation of science, encourage the growth of citizen science in Europe, and support the participation of the general public in research processes. The goals of the CS4H WG are specifically to increase the social and scientific impact of citizen science for health, by creating a community of stakeholders dedicated to promoting and developing citizen science for health; developing and disseminating tools, methods, ethical frameworks and training materials for CS4H; and enhancing the visibility and potential of citizen science projects in the health domain.
The CS4H working group developed a survey, with the specific aim of getting a better view on different citizen science stakeholders’ perspectives on:
What sets CS4H projects apart from non-health-related citizen science.
Which conditions would need further development to support the growth of CS4H as a practice.
Through this survey, we aimed to better understand the characteristics and enabling factors of citizen science in the health domain and identify which of these aspects need future work.
Methods
A pilot survey was conducted at a workshop on “Enhancing Health through Citizen Science” during the ECSA conference in September 2020, initiated by authors GR, SW, LdB, and MdG. The 36 workshop participants were mainly professional researchers active in some form of citizen science in the health domain. The survey yielded a broad overview of the needs of the community working in the field of citizen science and health, and a strong interest in further collaboration. The results were documented in an informal workshop report (Remmers et al. 2020). This led to the establishment of the international ECSA working group CS4H in December 2020. This working group decided to pursue the pilot survey and to conduct it across a diverse range of countries and stakeholders, to further the reach of the survey, especially among patients and citizens, and to engage a wider range of responses.
Procedure and data collection
To carry out this work, a subgroup of the ECSA WG on CS4H was formed, made up of the first four authors of this paper. This task force met regularly online throughout 2021 and 2022 to design, pilot, and disseminate the survey, before closing it and overseeing the analysis of the results.
The survey was collaboratively re-designed by the members of the task force, consisting of both formal scientists and citizen scientists (see author contributions for details), and open for input by the wider ECSA WG CS4H. This resulted in a 34-item, online survey containing closed-ended questions applying both nominal and ordinal scales, plus some open-ended questions (see Supplemental File 1: Survey Citizen Science for Health). The survey was originally designed in English and was subsequently translated by WG members into German, French, Spanish, Portuguese, and Dutch. The survey received ethical approval from the University of Twente (no. 210928) and was technically hosted by the Citizen Science platform Scivil in Belgium, and designed and administered in Microsoft Forms. The survey was open between 1 January and 31 August 2022.
The survey was disseminated by members of the CS4H WG, using social media (LinkedIn, Facebook) and newsletters from their organisations. News items about the survey were placed in ECSA’s channels, and targeted emails were written to networks known to the members of the WG. A total of 254 responses were obtained. The raw data was processed and made suitable for analysis by DreamTeam-students of DesignLab, University of Twente. The preliminary survey results were presented at the Citizen Science conference in Aarhus, April 2022, in a workshop; at a poster session at the ECSA citizen science conference in October 2022; and discussed with the wider CS4H WG. The preliminary results as well as the feedback obtained, were then reviewed and discussed in the sub-group and incorporated into this paper.
Statistical data analysis and visualisation
The survey data was exported as an XLSX spreadsheet from Microsoft Forms and loaded into the statistical analysis software R, where it was visualised and analysed. The full code is online alongside the data (see data availability statement). For the quantitative analysis, we limited the data to the response options provided, removing individual responses that are provided as free-text responses (e.g., for self-identification). For the comparisons in perceived importance amongst a) those who self-identify as researchers compared with respondents identifying as persons with a health condition and b) those who are primarily familiar with researcher-driven citizen science and those more familiar with citizen-driven citizen science, we performed two-tailed Mann-Whitney U tests for each of the 13 different conditions and then corrected for multiple testing using False Discovery Rate.
Results
Demographics
Between January 1st and August 31 2022, a total of 254 individuals participated in the survey. The ages of respondents ranges from 18 to 76 or older, with most respondents being between 26 and 55 (Figure 1a). About two-thirds of all respondents were female (Figure 1b), and 95% of respondents have some form of a higher education degree (Figure 1c).
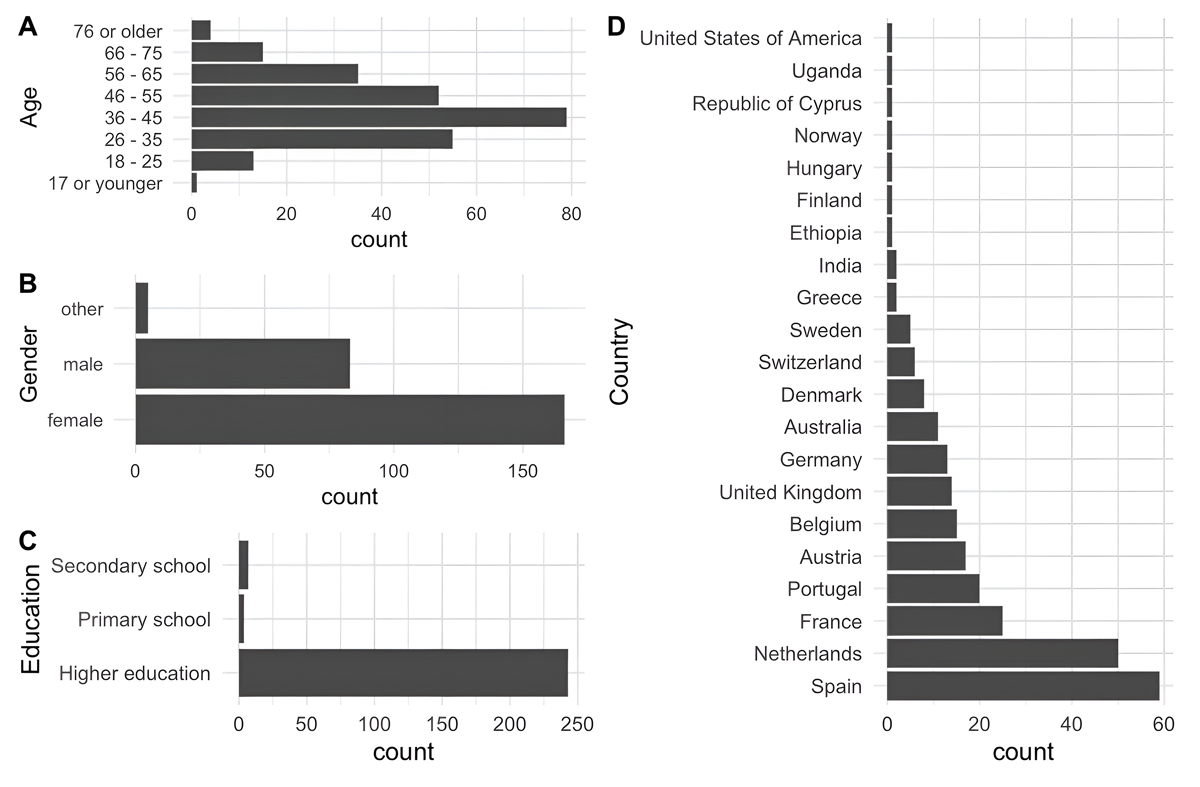
Figure 1
The demographic profile of respondents to the survey: (a) age distribution, (b) gender distribution, (c) education distribution, and (d) geographic profile.
In terms of geographic distribution, most of the respondents are living and working in Western Europe, with respondents from Spain and the Netherlands making up 43% of respondents (Figure 1d). Outside of Europe, a smaller number of respondents participated from Australia, India, Ethiopia, Uganda, and the United States.
To better understand the profile and background of respondents, we also asked respondents to optionally self-identify using a number of predefined categories such as researcher, person with/without a health condition, citizen science project manager, carer for someone with a health-condition, or health professional, but they could also write in their own identifications and select as many identifications as they wanted. All but one respondent answered this question.
The majority of respondents (54%) identified themselves as researchers, followed by “person without a health condition” (33%). As respondents could select multiple self-identifications, we also looked at which combinations frequently occurred, finding that most respondents only selected a single label (Figure 2a), with only the combination of “researcher” and “person without a health condition” having any significant overlap (8.6% of respondents). We furthermore also asked respondents to specify if they had any involvement in citizen science in general and/or in specific health-related citizen science before taking the survey. Overall, we found that 70.1% of respondents were involved in any form of citizen science, regardless of academic field, prior to taking our survey. Furthermore, 51.6% of all respondents answered that they had involvement in health-related citizen science before the survey. With few exceptions, such as respondents who identified as citizen science project managers or health professionals, these numbers remain quite stable across the respondent groups (see Figure 2b, c).
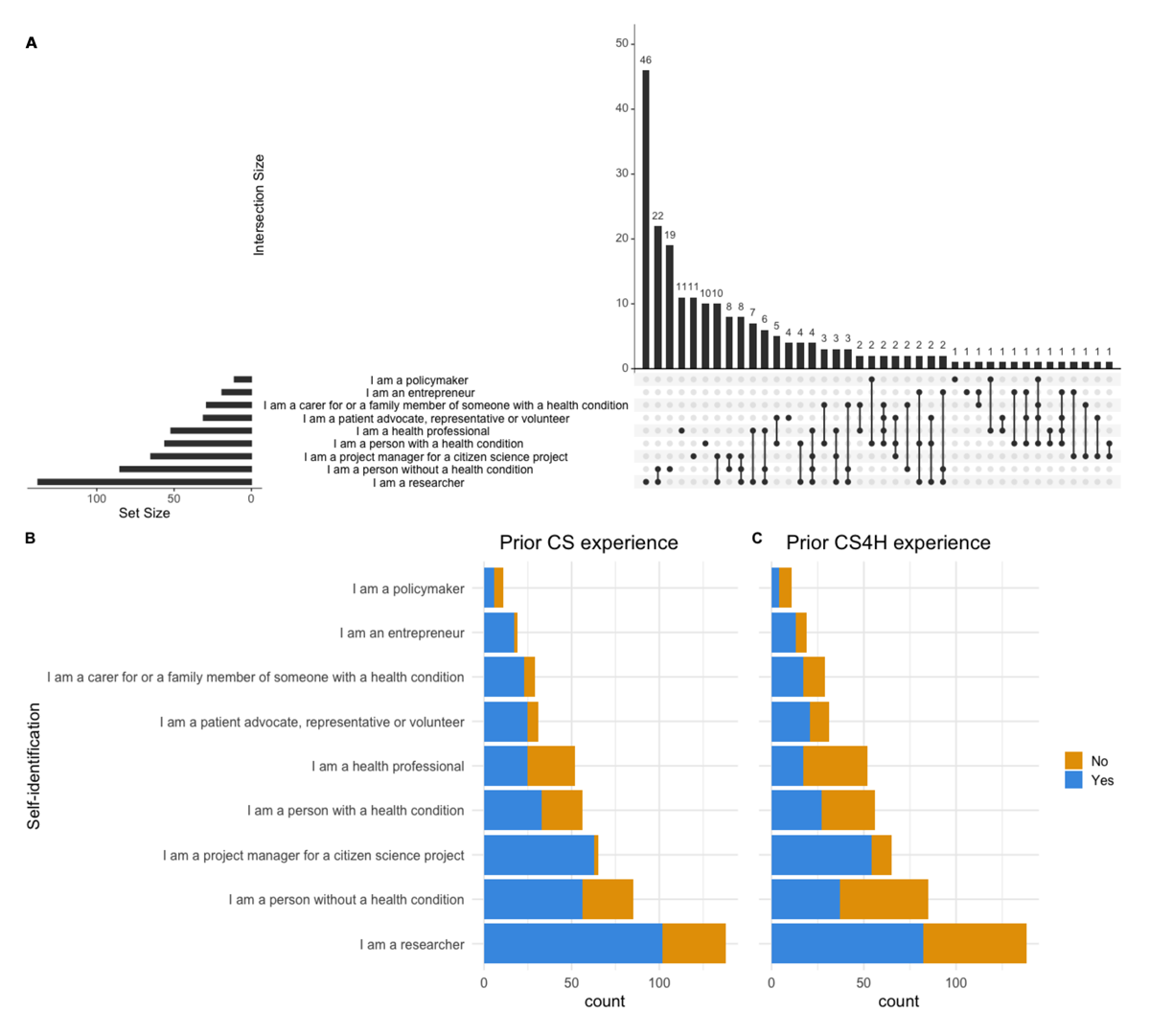
Figure 2
(a) Self-identifications chosen by respondents. The left-hand bars show the total number of responses per category, the right-hand bars show overlapping responses and frequency as respondents could select multiple categories. (b,c) The breakdown of respondents by self-identification and whether they had prior experience with citizen science generally (b), and health-related citizen science specifically (c). CS4H: Citizen Science for Health.
The 131 respondents that had prior experience in citizen science for health (51.6 %) were also asked to classify the project that they are or had been most involved in across two axes (see Figure 3). Of these, 121 respondents classified their projects. The vertical axis shows the purpose of the project (whether it aims for generic/public goals, or an individual goal, such as a patient exploring personal health questions). The horizontal axis shows whether a project is driven by academic researchers or by citizens/patients (Figure 3).
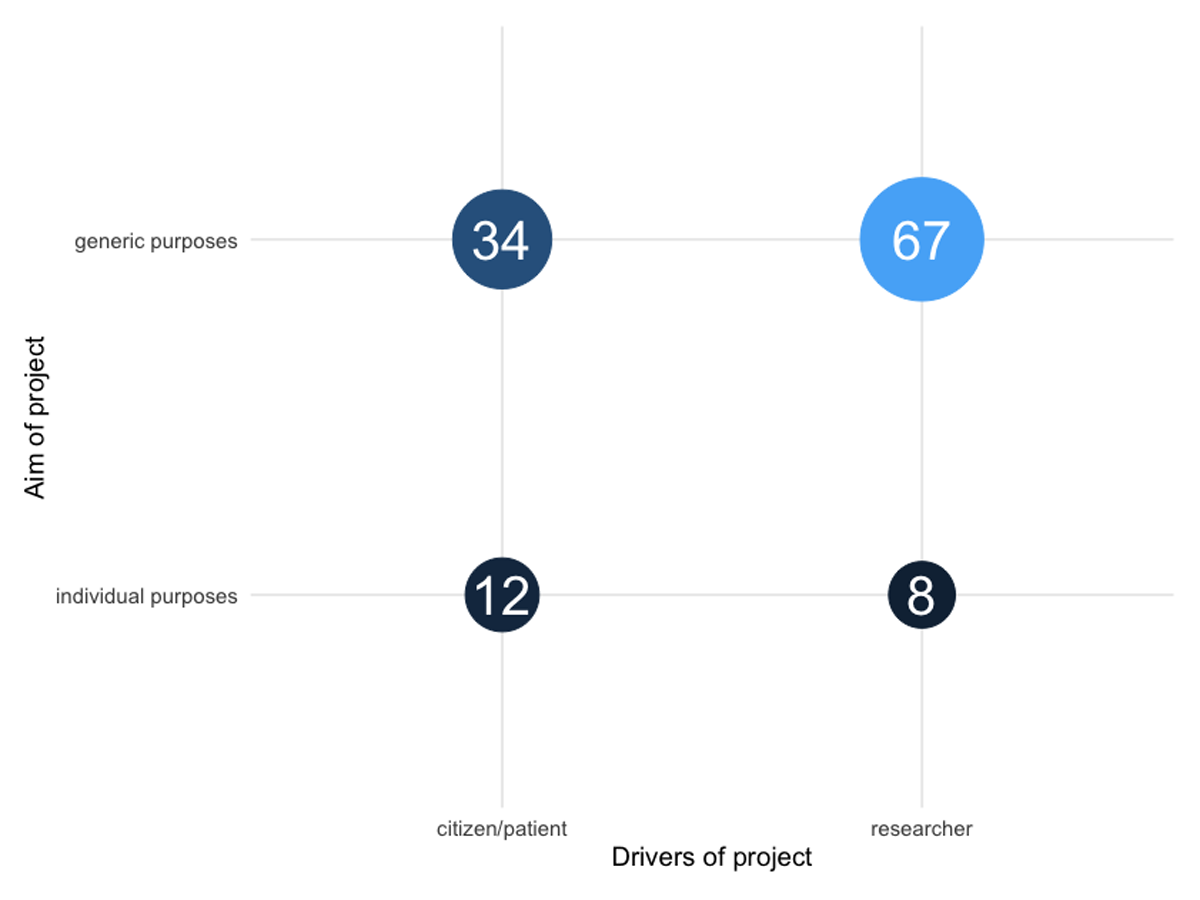
Figure 3
Classification of the CS4H projects that survey respondents are or have been involved in. CS4H: Citizen Science for Health.
Most of the respondents’ CS4H projects are driven by researchers (>60%), and most of the CS4H projects strive for generic goals (>80%). In contrast, CS4H projects that mainly explore individual health questions are less represented. This breakdown differs between who the main project drivers are: 25% of projects driven by citizens or patients explore individual purposes, whereas only 10% of researcher-driven projects do so.
What makes health-related citizen science different?
One of the goals of our survey was to understand which factors (if any) make health-related citizen science different from citizen science more generally. It is important to note that our focus was on the perception of CS4H practitioners of the differences between citizen science in health and citizen science in other domains. Based on our previous pilot study at the 2020 ECSA conference, we suggested a number of options from which respondents could select multiple answers, while also giving them the opportunity to suggest their own differences. Panels b and c in Figure 2 provide insight into whether respondents have experience with citizen science in health and/or in other domains. A vast majority of respondents see at least a few differences between health-related citizen science and citizen science more broadly, with only 6.7% of respondents reporting that they do not see any marked differences.
Three main differences emerge that are perceived by the majority of all respondents:
The ethical requirements and consent mechanisms are of a different nature (66.9% of respondents);
In health, citizens are more likely to be the subject of research than in other areas of citizen science (57.9%); and
The dynamics between stakeholders (e.g., patients, doctors, researchers) are more complex (57.5%).
Afterwards, we also investigated if respondents differed in their perception of potential differences according to their prior experience with (health-related) citizen science. (Figure 4). The results are sorted out in four groups (A to D). The respondents within group A (n = 76) indicated that they had not been involved in any form of citizen science prior to completing the survey, whereas the ones in group B (n = 178) answered that they had. Group B is then split into two subgroups (C and D). Group C consists of 47 respondents with experience in citizen science, but not specifically in the health domain; whereas the 131 respondents in group D did have that specific experience. The data do not permit to further split group D into those with having “only” or “also” experience in health-related citizen science.
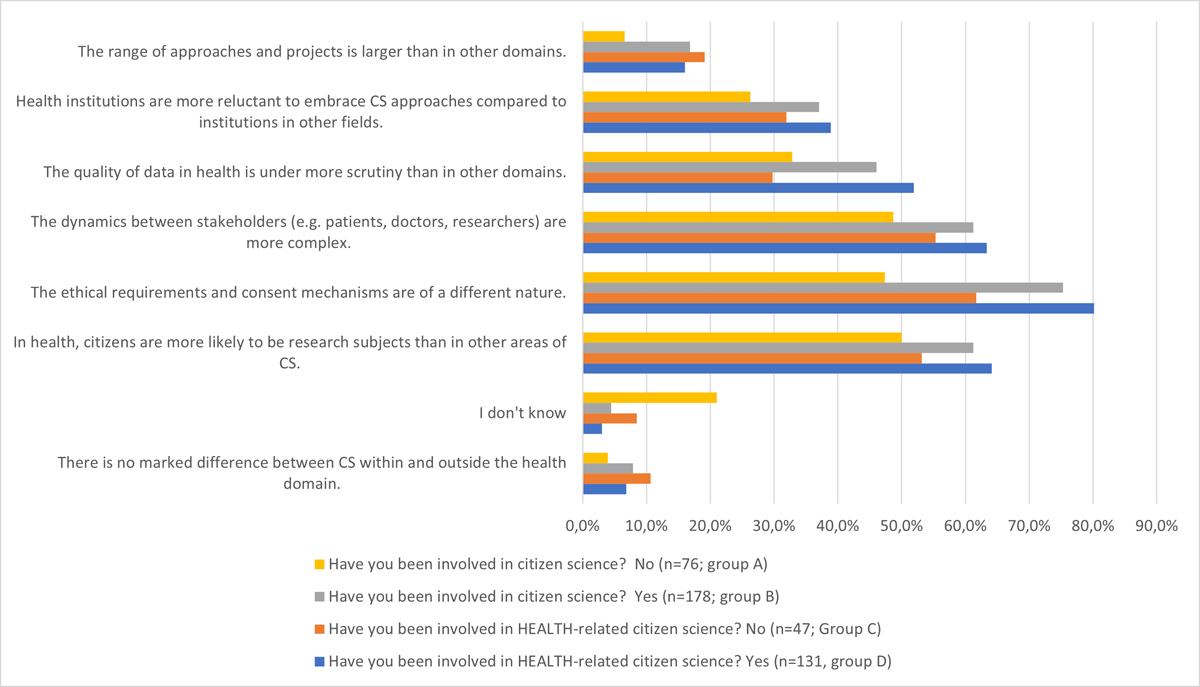
Figure 4
Perceived differences between health-related citizen science and other forms of citizen science. Results are grouped by whether respondents had prior involvement with (health-related) citizen science or not (groups C and D are subsets of group B).
What stands out most from the differentiation in Figure 4 is that the ranking of the perceived differences remains practically unchanged across all groups. Even those that had no prior experience with citizen science (group A), and hence had to base their observations on their general idea or intuition of what citizen science and citizen science in the health domain entails, came to a similar top-3 prioritization of the differences as those with prior experience, albeit with less pronounced differences among the issues. We have no explanation for this phenomenon, other than that their generic engagement with science and health may have provided them with a hint of what is happening within the domain of citizen science for health. The relatively high score for group A on “I don’t know” (21.1 %) suggests, however, less confidence in selecting options. Also, those with experience in citizen science, but not in the health domain (group C), tended to select “I don’t know” more often than those with experience in health (8.5 % versus 3.1 %). A slightly larger portion of group C as compared with group D (10.6% versus 6.9%) considered that there are no marked differences between citizen science within and outside the health domain. Put differently, those with experience with citizen science in the health domain (group D) tend to have a more outspoken perception of the differences. This is shown, for example, very clearly on the issue of “ethical requirements and consent mechanisms,” which is considered an important difference by 80.2 % of this group, versus 61.7% of those lacking such specific experience, and 47.4% of those without any experience with citizen science at all.
Necessary conditions to grow health-related citizen science
We also investigated which conditions would need to be enhanced or strengthened for health-related citizen science to grow as a practice. To that end, we asked the 131 respondents that had prior experience through health-related citizen science projects to score 13 conditions (see Table 1) that were identified during the 2020 ECSA conference, and at a later stage refined by the survey-subgroup, on a 5-point scale from not important at all to very important.
Table 1
An overview of 13 conditions for the growth of health-related citizen science that respondents were asked about. Survey participants responded to the conditions exactly as worded in this table. The “short title” is introduced in this paper for convenience.
| SHORT TITLE | CONDITION |
|---|---|
| ROI | Balanced “return on investment” – both researcher and citizen/patient must be satisfied with participating in the project |
| Ethics | Adequate ethical frameworks and review procedures |
| Data Infrastructure | Data infrastructure to appropriately connect data of different sources (e.g., Real World Data, clinical data, etc.), including issues such as data quality, ownership, security, interoperability |
| Dissemination | Publication and dissemination of research and results |
| Tooling | Provision and development of tools for citizens to conduct research (apps, ehealth devices, adequate research procedures, etc.) |
| Citizen Visibility | Make the existing diversity of citizen science practices visible (unlocking the potential of citizens) |
| Lobby | Communication and lobby channels vis-a-vis policy makers |
| Learning Infrastructure | Development of a multi-stakeholder co-creative learning infrastructure |
| Education | Familiarity with or understanding of (medical) professionals about citizen science |
| Health Records | Access of citizens to their health records |
| Legal Frameworks | Legislative frameworks (e.g,. regarding eHealth tools, involvement of industry) |
| Literature | Access to health literature for citizens |
| Labs | Access to lab facilities for citizen/patients |
We converted the scoring into a numerical scale from -2 (not important at all) to +2 (very important) and calculated the mean across all 131 respondents, to rank the different conditions by their perceived importance (Figure 5). No condition reached an average score below zero, indicating that none of them were seen as unimportant by a majority of our respondents and only access to lab facilities for citizens/patients, which scored close to zero (0.14), was seen as mostly neutral. On the upper end of the scale, the highest scoring conditions were balanced return on investment (1.47) and adequate ethical frameworks (1.41).
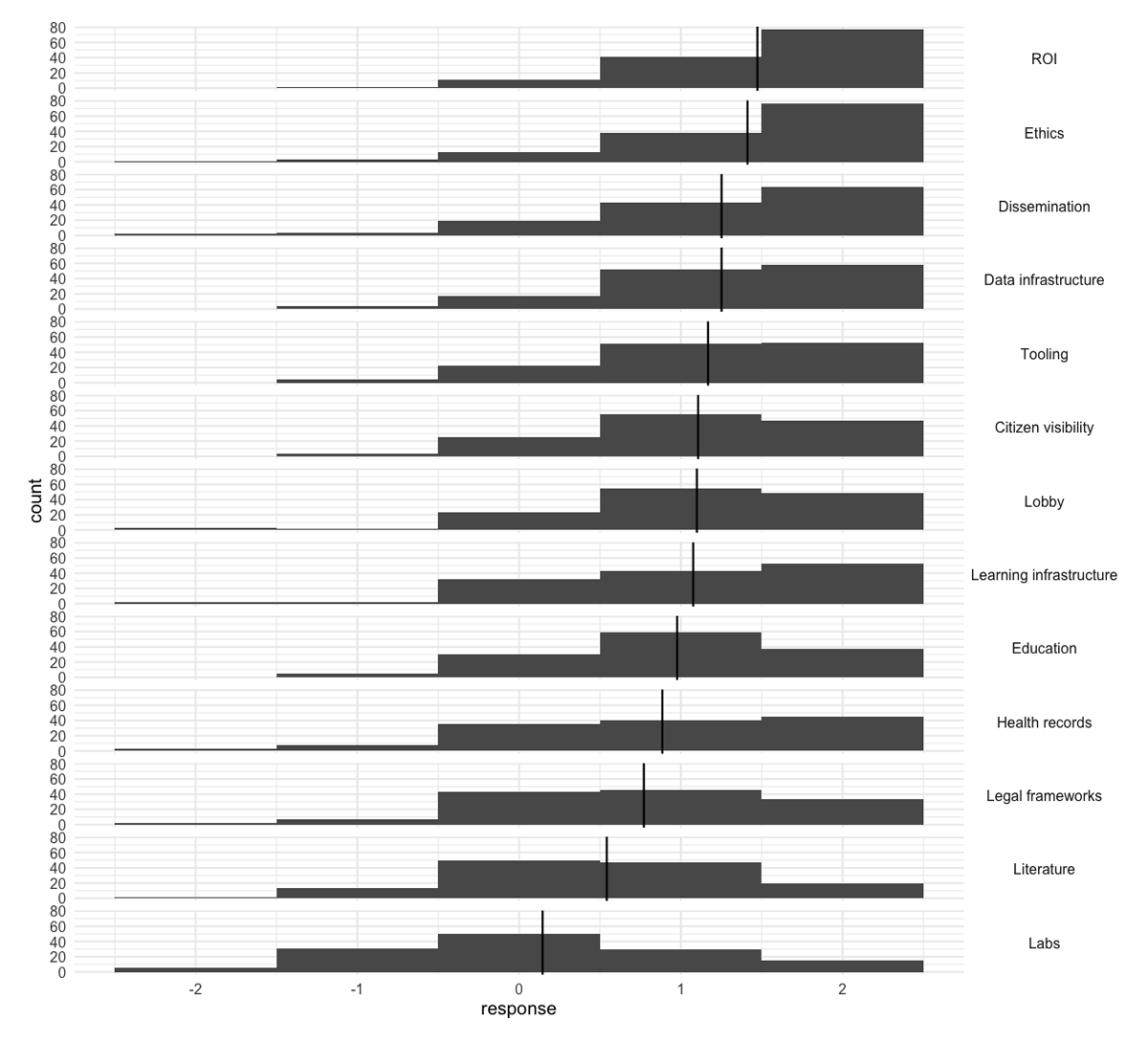
Figure 5
Respondents’ views on the importance of 13 conditions to further grow health-related citizen science, from -2 (not important at all) to +2 (very important). Bars give the absolute number of responses, and vertical lines give average scores.
Given the diversity amongst participant backgrounds, we aimed to investigate whether the perceived importance of these conditions differed based on self-identification. As our sample of respondents was heavily skewed towards respondents that are researchers, we could not perform an exhaustive group-by-group comparison. Instead, we focused on the comparison between “researchers” and “people with a health-condition” because these two groups represent two of the main stakeholders in health-related citizen science projects, and also because there was comparatively little overlap between the two groups while retaining enough respondents to make a comparison (see Figure 2).
Looking at the two groups side-by-side we observe that there are very few differences between them (Figure S1, in Supplemental File 2: Supplemental Figures, Tables, and Text), with most of the conditions being scored similarly between researchers and peope with health-conditions. In some cases (like dissemination or ethics) researchers score the condition slightly higher than patients, while in other cases—such as access to citizen visibility or access to literature—the picture is reversed. The latter condition is one of the few in which the median scoring of researchers is neutral. However, people with a health condition score this condition as important. Regardless of these smaller differences, none of those differences are significantly different when performing a Mann–Whitney U test and correcting for multiple testing using False Discovery Rate.
We then similarly compared the respondents’ perceived importance rankings based on whether they are mostly familiar with CS4H projects that are driven by professional researchers or citizens/patients (see Figure S2 in Supplemental File 2: Supplemental Figures, Tables, and Text). Here, we also do not observe marked differences between both groups, with the biggest differences being respondents who are more familiar with researcher-driven CS4H efforts ranking the perceived importance of a balanced ROI lower than those who come from a citizen-driven CS4H background. In contrast, we observe the opposite effect with respect to the importance of accessing the academic literature. As for the personal self- identification, differences are small and not statistically significant.
Discussion
In this section, we put forward the limitations of our approach, as well as discuss our results.
Limitations
As an interdisciplinary and broad approach, citizen science has many forms (Haklay et al. 2021a). We discuss the perceived particularities that, according to the survey respondents, are unique to the domain of health, as well as the conditions that are in need of further development to enable growth of citizen science for health as a practice. Given this breadth and diversity of health-related citizen science, we claim no representativeness for health-related citizen science in general, instead the results need to be seen in the context of the survey’s design. In this sense, our survey asked respondents only about their perspectives on citizen science in health, and this is not an extensive comparison with other citizen science domains, implying we have no information about the exact respondents’ experience in those other citizen science domains.
The survey presented in this paper was created by the CS4H WG of ECSA, and was disseminated through the networks of its members. Because of this, a large number of respondents are engaged in citizen science as it is developing in Europe. Additionally, this creation and dissemination process may have contributed to an overrepresentation of researchers’ perspectives despite best efforts to overcome this. Consequently, our survey may have missed out different perspectives, both in terms of regions and stakeholders. Furthermore, respondents engaged in CS4H projects that primarily explore individual health questions are less represented in this survey. This implies a limitation of our research, and our findings might need to be adjusted for future research involving a larger number of respondents engaged in this kind of CS4H project. Despite this, our results can shed light on some important aspects of CS4H, and we call for further research to complement knowledge of perspectives from less-covered regions, stakeholders, and CS4H projects.
The particularities of citizen science in health
Despite these limitations, some consistent views on the characteristics that set health-related citizen science apart from other citizen science projects can be observed. Three main particularities for citizen science for health emerged, as they were mentioned by over 50% of the respondents, across all backgrounds, and regardless of experience with health-related citizen science, and even regardless of whether they had experience with citizen science at all: (1) the ethical requirements and consent mechanisms are of a different nature, (2) citizens and patients are more likely to be the subject of research than in other types of citizen science, and (3) the dynamics between stakeholders are more complex.
These points seem to be, by their nature, highly interlinked: If citizen scientists are more likely to (additionally) participate as subjects in the research, then ethical requirements are likely to differ from other research approaches that do not involve participants as human subjects, as described below. Similarly, this additional role that participants can play in health-related citizen science means that the interactions and dynamics between stakeholders become more complex.
While the ethical conduct of researchers is important in other disciplines as well (Iaccarino 2001; Reijers et al. 2018), few other research domains deal so intimately with the personal sphere as health research. Ever since the World Medical Association’s Helsinki Declaration on research with human subjects (WMA 1964), research and biomedical ethics are a key part of medicine and health research, with the expressed goal of minimising individual harm and maximising public value (Beauchamp and Childress 2001; Rice 2008; McNair 2022). In public health research—where communities and groups instead of individuals are at the core—additional ethical frameworks with a focus on societal justice are necessary (Ballantyne 2019). Overseeing these ethical frameworks to protect research subjects typically falls to Research Ethics Committees. Jacobs and Tinnerholm Ljungberg (2021) assert that these committees have become “gatekeepers of science” to their central role, and have the power to give legitimacy to certain ways of probing into the world and not others. In the same vein, Stark (2012, p. 229) claims that research ethics committees “in so doing, …change what is knowable.”
Conflicts can emerge at the interface of these ethical frameworks and citizen science, as the latter deliberately expands the roles of citizens from mere followers to active leaders (Senabre Hidalgo et al. 2021; Eitzel et al. 2017). When people with health conditions engage in self-experiments—as we all do in our ordinary lives by adapting our lifestyles—long-standing ethical policies in health research struggle to adapt to such different modes of research: Citizens tend to introduce what can be labelled as “practice-based evidence pathways” as opposed to the “evidence-based practice pathway” which is dominant in health research (Ogilvie et al. 2020; Greenhalgh 2020).
Given the central role of “evidence” in healthcare—e.g., in defining treatment protocols, reimbursement schemes, policy development, etc.—the processes of data collection (Resnik 2019) and evidence construction are highly scrutinised. In line with this, in our survey we find that the research practices that generate evidence and the ethical requirements to govern these processes are viewed as important particularities of citizen science in health when compared with other domains of science. For this reason, research methodology, ethics, and their interrelationship merit further study.
A joint dialogue is necessary to overcome those barriers, but as health research professionals are embedded within the status quo, having such a dialogue on equal footing is not an easy task: Green and Johns (2019) argue that citizens in the role of patients need to be empowered to deal with such power relations in order to provide their knowledge, data, and experience. In turn, health researchers need to listen and open up to citizens’ demands and become more democratic, transparent, and aligned with society demands.
Factors for growing citizen science in the health domain
We also aimed to get a better understanding of which factors would need improvement to support, nurture, and grow this practice. Out of the 13 conditions we asked about, two stand out as particularly important to the respondents: (1) a balanced return on investment (ROI) for both researchers and participants (patients or citizens), and (2) adequate ethical frameworks.
Both formal and informal researchers need to derive value from their engagement in citizen science. The balanced ROI is different for researchers and patients or citizens. For researchers, trustworthy data and the possibility to publish or patent/licence are important outcomes for their career recognition and assessment; whereas for patients or citizens, other values, such as helping to solve medical problems, the joy of participating in science, or recognition as a contributor to research may be more relevant (Senabre et al. 2022; Haeusermann 2017). In the health domain, which typically views participants or patients as “research subjects” who need to be protected, the ROI for patients is often limited to compensation for travel costs and more abstract future benefits for society, such as better health care. In citizen science, patients claim benefits that are more immediate, and that reflect their role in the research, such as more clarity on what helps them or what does not (Richards et al. 2018).
In particular, this deeper involvement and the changed role of participants is linked to the second important condition, that of adequate ethical frameworks. These have been an active topic of discussion and research in the field of health-related citizen science. Wiggins and Wilbanks (2019) highlight how traditional health and biomedical research is governed by a variety of regulatory and legal frameworks that are aimed at protecting research participants from misdemeanours by scientists and institutions. These existing frameworks rely on research being situated and led by institutions, which can be problematic. Depending on the nature of a given health-related citizen science project, these relationships with institutions can be wholly or partially absent, or researchers and participants can face each other in more collegial relationships. Lewis (2022) and Fiske et al. (2019) also identify similar challenges around ethical review procedures not being adapted to citizen science and patient-led research. As such, the question of how to design and implement ethical oversight methodologies that can help facilitate health-related citizen science—while serving and protecting non-institutional participants—remains an open and urgent question that should be given attention to help grow health-related citizen science. In fact, citizen science projects that operate or emerge outside academic and/or institutionalised bodies lack expertise in their core teams on ethical committees’ submission processes or even have problems identifying the regulating body to address. At the same time, ethical committees are still not familiarised with citizen science practices and thus can hamper grassroots, bottom-up, health-related citizen science projects (Magalhães et al. 2023; Remmers et al. 2023).
The concept of “adequate ethical frameworks” also highlights an interesting discrepancy in the ranking of importance between factors: While ethical frameworks come out on the top, the highly related issue of “legal frameworks” appears only towards the bottom of the list. Partially, this might be due to the survey sample, which is skewed towards researchers, who most often encounter regulatory frameworks through the lens of ethical oversight and engage a lot less frequently with the legal frameworks behind them. As already seen above, the ethical concerns surrounding citizen science broadly (Rasmussen 2019; Resnik 2015; Resnik 2019) and for citizen science in the health domain in particular (Wiggins and Wilbanks 2019; Fiske 2019; Groot 2022) remain frequently discussed issues amongst both researchers and bioethicists working in the field. In contrast, there has been very limited research (or even calls for research) into how legal frameworks would need to adapt for CS4H (Vayena 2016). This seems, however, important, as the legal frameworks set the boundaries of how ethical oversight frameworks can be shaped in practice (Hoffman 2015). Interestingly, we observed a similar contradiction in the perceived importance through the rankings between the “Dissemination” and “Access to Literature” factors. A discussion of this, as well as further discussions of the other—less high-ranked—factors can be found in Supplemental File 2: Supplemental Figures, Tables, and Text).
Conclusion: a Future Direction for Citizen Science for Health
Health-related citizen science is a practice with much potential to improve the real-world impact that biomedical, health, and public health research can have on both patients and society at large. The goal of this work was to explore the perceived particularities that set health-related citizen science apart from citizen science done in other domains. The survey described in this paper aimed to create a better understanding of these particularities by collecting the views of a wide range of actors and stakeholders that are engaged with both citizen science more broadly and health-related citizen science in particular. In addition, we tried to acquire insights about enabling conditions for health-related citizen science to thrive.
Based on the survey discussed herein, two large topics emerge, both of which set health-related citizen science apart but also need further development to help grow this practice. On the one hand, we find a strong need for health-related citizen science to deliver a balanced ROI to all stakeholders involved, but most immediately to patients and citizens, as well as researchers. On the other hand, health-related citizen science projects need to operate in adequate ethical frameworks. Historically, the regulatory ethics bodies in biomedical health research were developed under the assumption of a strong divide between patients and researchers. In the public health domain, this divide is a less poignant issue, although not absent. As health-related citizen science is poised to blur these boundaries, there is a growing need to adapt oversight mechanisms to these changes.
To deliver on the promises of health-related citizen science, it will be necessary to develop a more coherent community of practice that includes a more diverse and balanced set of stakeholders beyond citizen science practitioners and researchers. These stakeholders can learn, communicate, raise awareness about, and lobby for the implementation of health-related citizen science examples that can address these current barriers. Due to the demographic sample that this work achieved, the findings represent the perspectives of researchers more than those of other stakeholders, suggesting that future work will have to investigate those other stakeholders’ views in more depth, in particular citizens and patients, ethicists and regulators.
Data Accessibility Statement
The survey data and code used for the data analyses are openly available on Zenodo at https://doi.org/10.5281/zenodo.10944208
The released dataset does not include the free text questions to further minimise the risk of participant re-identification.
Supplemental Files
The Supplemental Files for this article can be found as follows:
Ethics and consent
This study was approved by the ethics committee of the University of Twente (approval no. 210928).
Acknowledgements
We want to thank the attendants of the 2020 ECSA conference workshop, where the survey was originally conceived, as well as the 60 plus members of the ECSA Working Group on CS4H for their early input, their ongoing comments on earlier drafts of the survey, and their efforts in distribution. We particularly want to thank Mic Starbuck, patient advocate for the Chest, Heart and Stroke Foundation Scotland, who has been a member of the survey taskforce of the Working Group and who contributed to the early stages of the survey, until his health would impede him to continue his work and we lost contact. We would like to thank the University of Twente students Baris Imre, Thijs Bianchi, Jelise Schokker and Rosaline Voorend who made the first effort to analyse the raw data. Our appreciation goes to all respondents who volunteered their time to fill out our survey. We would also like to thank the two anonymous reviewers and the CSTP section editor for their elaborate comments. Their more distanced look allowed us to clarify and improve the paper.
Funding Information
This project relied on in-kind contributions and was furthermore partially supported by existing funding to individual authors: The contributions of GR and SW were enabled by the TOPFIT Citizenlab project that was supported by the Regio Deal Twente; BGT was supported by a long-term fellowship of Fondation Bettencourt-Schuler, IB was supported by the European Union’s Horizon 2020 research and innovation programme (CoAct, under grant agreement no. 873048), JM received funding from the European Union’s Horizon 2020 Research and Innovation program under Grant Agreement n. 101006386.
Competing Interests
The authors have no competing interests to declare.
Author Contributions
The original idea and performance of the 2020 pilot survey was by GR, LdB, SW, MdG. GR, BGT, AA, JvL and Mic Starbuck (see acknowledgements) formed the taskforce as part of the ECSA Working Group CS4H to further elaborate and conduct the survey. Translations of the survey were provided by EC and IB (French), EC, EGT, SM and IB (Spanish), BGT (German), JvL and GR (Dutch) and JM (Portuguese), all of them but EC also members of the Working Group CSforHealth. JvL took care of the technical hosting of the survey. BI, as lead of a group of students of University of Twente, did a first quantitative analysis, which was then refined and completed by BGT. Interpretation of the results was done by BGT, GR, AA and JvL. BGT, GR and AA contributed equally to the writing of the paper, MdG, LdB, SW, JM, SM and IB provided input. All authors approved the final version of the manuscript. Throughout the process, GR acted as coordinator.
