Introduction
In Italy, the agricultural sector employs about 500,000 migrant workers, nearly half of its workforce. At least 180,000 face exploitation, often living in makeshift settlements or “ghettos” far from urban centers [1, 2]. In Puglia, one of the country’s major agricultural regions, over 60% live in unsafe, rundown structures lacking essential utilities such as water, electricity, and sanitation [3–5]. These conditions, together with systemic exploitation by illegal labor intermediaries (caporali), exacerbate their vulnerability [6, 7]. Despite Italy’s universal healthcare system, many migrants encounter linguistic, cultural, and bureaucratic barriers, as well as irregular legal status [1, 3, 4, 7]. Most migrants are subject to strong seasonal migration, moving according to harvest periods, and this negatively affects the continuity of care. Since 2017, Doctors with Africa University College for Aspiring Missionary Doctors (CUAMM) has addressed these issues through its “Supreme” project. By deploying mobile clinics across 12 informal settlements, CUAMM provides free healthcare and social‑health orientation to some of the region’s most marginalized populations. Recognized by the World Health Organization (WHO) as a best practice in migrant health, this model is often the only access point for care, fostering trust and bridging critical gaps [8, 9].
This study investigates the health needs of migrant agricultural workers in Puglia, assesses the effectiveness of mobile clinics, and identifies systemic barriers to accessing care. It focuses on common conditions (musculoskeletal disorders, respiratory infections, and dermatological issues), considers follow‑up visits as an indicator of trust, and examines the role of social factors such as housing, legal status, and access to primary care. The findings offer actionable insights to guide targeted interventions, enhance healthcare delivery, and advocate for policy changes to ensure equitable, continuous care for this vulnerable population.
Methods
This study analyzed healthcare visits conducted between 2017 and 2023 by volunteers from Doctors with Africa CUAMM in 12 informal settlements inhabited by foreign agricultural workers in the Puglia countryside, as showed in Figure 1. Visits from 2024 were excluded owing to ongoing data collection and continuous updates to the database.
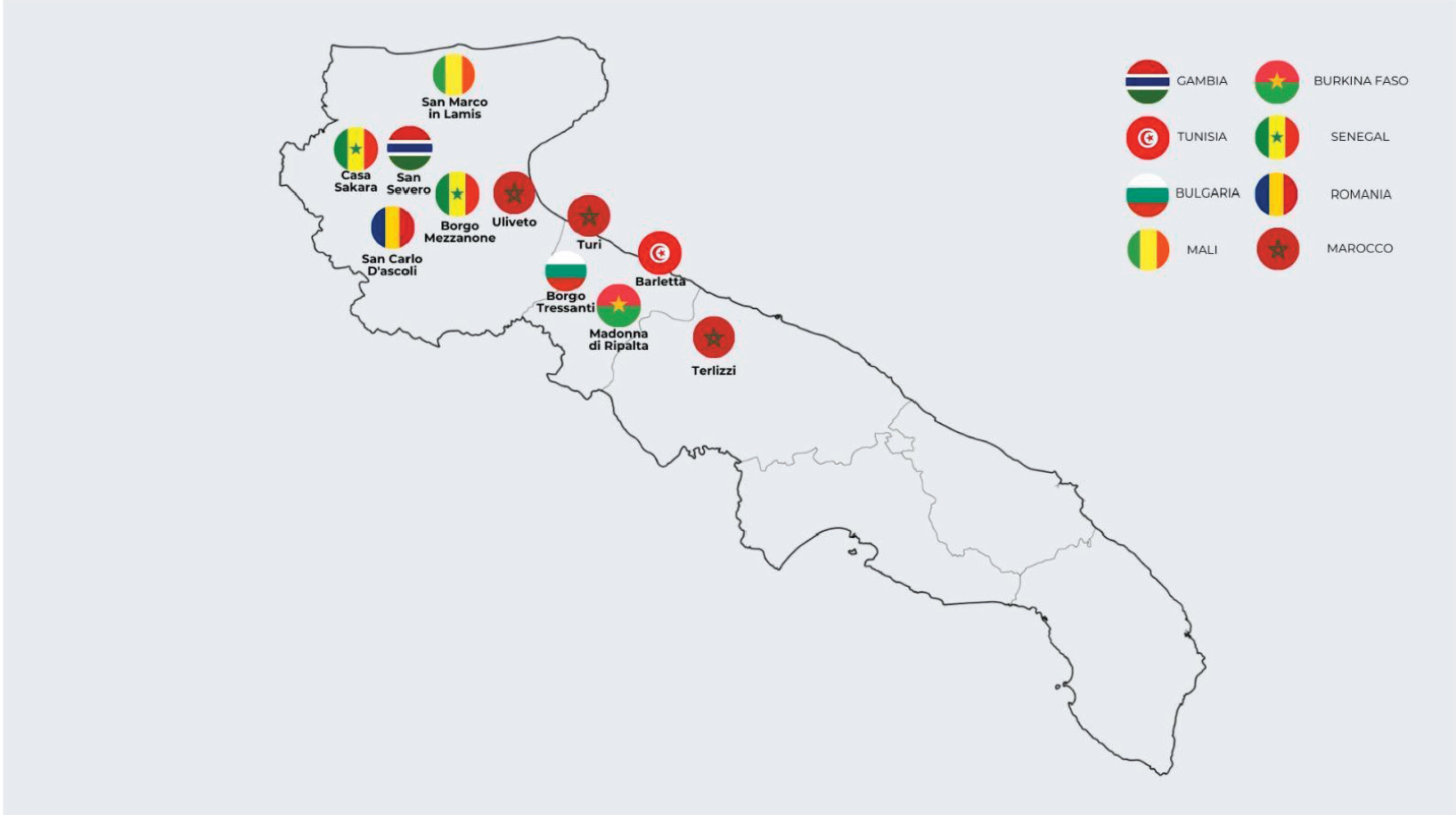
Figure 1
Map of the informal settlements supported by Doctors with Africa CUAMM.
The informal settlements included in this study share common structural and socioeconomic characteristics. They are geographically isolated, often located far from urban centers, with no direct access to essential services such as electricity, running water, and sanitation. Housing conditions are precarious, with only a few permanent structures in masonry; the majority of dwellings consist of makeshift shelters built from sheet metal and other temporary materials.
The medical visits were carried out aboard a mobile clinic staffed by a multidisciplinary team comprising a doctor, nurse, medical resident (specializing in infectious diseases, surgery, dermatology, or other fields), cultural mediator, and social care worker. The caravan was equipped with a medical bed, a large supply of medicines for the most common pathologies, a sphygmomanometer, a pulse oximeter, a portable ultrasound, an electrocardiogram (ECG) device, a glucometer, and rapid tests for human immunodeficiency virus (HIV), severe acute respiratory syndrome coronavirus 2 (SARS CoV‑2), and hepatitis C virus (HCV). On average, 8 days of activity with a camper were carried out each month, with oscillations between 4‑ and 12‑monthly outreach, in relation to the presence of agricultural workers and the possibilities of the nongovernmental organization (NGO). Data collected during these visits—including demographic, socio‑health, anamnesis, and clinical information—were systematically recorded in a Microsoft Access database as well as in an anonymized Excel file. Descriptive analyses were performed to characterize patients at their first recorded visit. Categorical variables were summarized as absolute and percentage frequencies, while continuous variables, such as age, were described using the median, mean, and standard deviation (SD).
Subsequent analyses examined repeated visits, focusing on the frequency of visits (absolute and relative), gender distribution, diagnosed pathologies, and administered therapies.
Factors associated with voluntary follow‑up visits, used as a proxy for trust in the healthcare model, were investigated using simple and multiple logistic regression analyses. Variables were selected through a stepwise bidirectional approach to minimize the Akaike Information Criterion (AIC). Key variables, such as age at the first visit (categorized into ranges) and gender, were included in the model regardless of statistical significance to control for potential confounders. Odds ratios (ORs) and their 95% confidence intervals (CI) were calculated using Blaker’s approach.
Follow‑up visits were considered an important outcome variable, as mobile clinics often represent the only access to healthcare for this population owing to their geographic isolation and multiple structural barriers. Given the lack of alternative healthcare options, patients were encouraged to return for continued care and monitoring, particularly for chronic conditions, treatment adherence, and unresolved medical issues. The length of follow‑up varied on the basis of individual health needs, with some patients requiring multiple visits over several months or years, while others returned only for acute care episodes.
The study was conducted in accordance with the Declaration of Helsinki and national and institutional standards. All statistical analyses were conducted using the R programming language within the RStudio Integrated Development Environment (IDE).
Results
Demographic and settlement characteristics
The analysis of 2,537 first visits revealed a significant gender imbalance, with male patients comprising 95.8% of the sample and female patients only 4.2% (Table 1; Figure 2). The gender distribution varied across settlements, with women representing 26.5% in Borgo Tressanti but only 0.4% in Arena and 0% in Turi. Settlement sizes ranged from 7 patients in San Carlo d’Ascoli (0.3%) to 843 in Pista (33.2%) and 650 in Casa Sankara (25.6%) (Table 1). Patient nationalities were varied, with Senegal (27.0%), Gambia (20.6%), Morocco (13.6%), Mali (10.0%), and Nigeria (5.4%) being the most represented (Table 2). Variations by settlement were notable: for instance, Senegalese migrants dominated in Casa Sankara, while Gambian patients were primarily concentrated in Pista. Figure 3 maps the geographic origins of the migrants.
Table 1
Absolute distribution and percentage of patients at the first visit by gender and location.
| GENDER SETTLEMENT | MALE 2,430 (95.8%) | FEMALE 107 (4.2%) | TOTAL 2,537 (%) |
|---|---|---|---|
| Arena (A) | 275 (99.6%) | 1 (0.4%) | 276 (10.9%) |
| Barletta (B) | 15 (100%) | 0 (0%) | 15 (0.6%) |
| Borgo Tressanti (C) | 50 (73.5%) | 18 (26.5%) | 68 (2.7%) |
| Contrada Cicerone (D) | 167 (99.4%) | 1 (0.6%) | 168 (6.6%) |
| Madonna di Ripalta (E) | 78 (95.1%) | 4 (4.9%) | 82 (3.2%) |
| Pista (F) | 773 (91.7%) | 70 (8.3%) | 843 (33.2%) |
| San Carlo d’Ascoli (G) | 7 (100%) | 0 (0%) | 7 (0.3%) |
| Sankara (H) | 643 (98.9%) | 7 (1.1%) | 650 (25.6%) |
| Terlizzi (I) | 63 (100%) | 0 (0%) | 63 (2.5%) |
| Terraneo (J) | 90 (93.8%) | 6 (6.3%) | 96 (3.8%) |
| Turi (K) | 223 (100%) | 0 (0%) | 223 (8.8%) |
| Uliveto (L) | 46 (100%) | 0 (0%) | 46 (1.8%) |
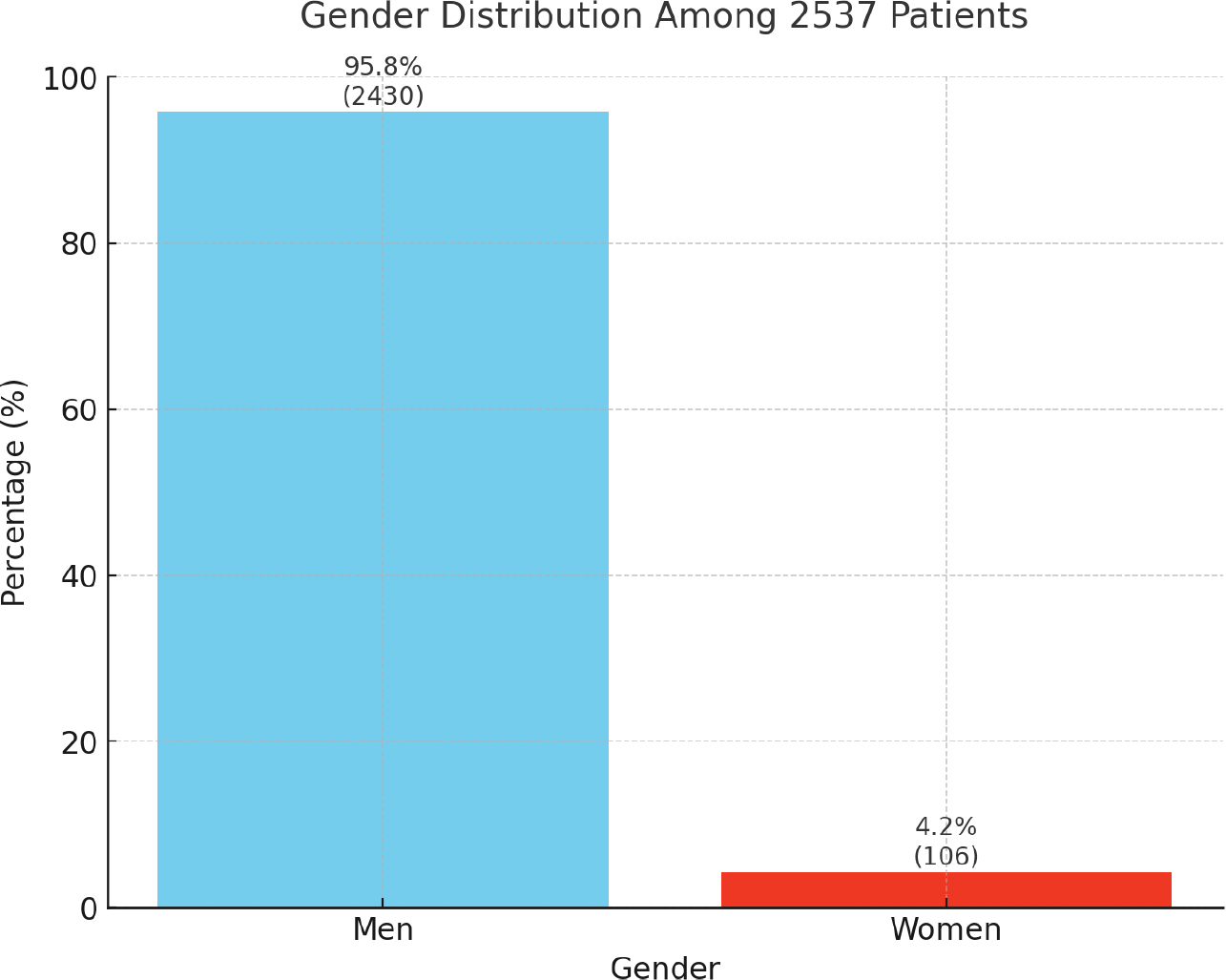
Figure 2
Gender distribution.
Table 2
Distribution of patient nationalities by settlement.
| SETTLEMENT NATIONALITY | N (%) | A | B | C | D | E | F | G | H | I | J | K | L |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Afghanistan | 14 (0.55%) | 0 | 0 | 0 | 0 | 0 | 14 | 0 | 0 | 0 | 0 | 0 | 0 |
| Algeria | 7 (0.28%) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 |
| Bangladesh | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Belgium | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Benin | 17 (0.67%) | 8 | 0 | 0 | 0 | 0 | 5 | 0 | 4 | 0 | 0 | 0 | 0 |
| Bulgaria | 29 (1.14%) | 0 | 0 | 28 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Burkina Faso | 109 (4.3%) | 1 | 0 | 0 | 2 | 62 | 8 | 2 | 3 | 0 | 31 | 0 | 0 |
| Cameroon | 8 (0.32%) | 0 | 0 | 0 | 0 | 1 | 3 | 0 | 4 | 0 | 0 | 0 | 0 |
| Chad | 4 (0.16%) | 1 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Congo | 3 (0.12%) | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ivory Coast | 86 (3.39%) | 16 | 0 | 0 | 28 | 4 | 20 | 0 | 16 | 0 | 2 | 0 | 0 |
| Ethiopia | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Gambia | 523 (20.61%) | 101 | 0 | 0 | 0 | 0 | 168 | 0 | 251 | 0 | 2 | 1 | 0 |
| Ghana | 33 (1.3%) | 2 | 0 | 0 | 1 | 0 | 21 | 0 | 2 | 0 | 7 | 0 | 0 |
| Guinea‑Bissau | 31 (1.22%) | 4 | 0 | 0 | 1 | 0 | 16 | 0 | 10 | 0 | 0 | 0 | 0 |
| Guinea‑Conakry | 110 (4.34%) | 11 | 0 | 0 | 13 | 1 | 55 | 0 | 30 | 0 | 0 | 0 | 0 |
| India | 5 (0.2%) | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Italy | 3 (0.12%) | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| Liberia | 3 (0.12%) | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Libya | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Mali | 254 (10.01%) | 42 | 0 | 0 | 103 | 4 | 54 | 1 | 44 | 0 | 5 | 1 | 0 |
| Morocco | 344 (13.56%) | 0 | 2 | 26 | 0 | 0 | 2 | 1 | 1 | 55 | 6 | 209 | 42 |
| Mauritania | 3 (0.12%) | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 |
| Mauritius | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Somalia (Mogadishu) | 1 (0.04%) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nigeria | 137 (5.4%) | 1 | 0 | 0 | 0 | 0 | 112 | 0 | 10 | 0 | 14 | 0 | 0 |
| Pakistan | 8 (0.32%) | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 | 0 |
| Poland | 9 (0.35%) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 8 | 0 | 0 |
| Punjab (India/Pakistan) | 2 (0.08%) | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Romania | 24 (0.95%) | 0 | 0 | 7 | 0 | 0 | 0 | 3 | 0 | 0 | 14 | 0 | 0 |
| Senegal | 686 (27.04%) | 85 | 0 | 0 | 15 | 1 | 315 | 0 | 263 | 0 | 3 | 4 | 0 |
| Sierra Leone | 11 (0.43%) | 2 | 0 | 0 | 0 | 0 | 5 | 0 | 4 | 0 | 0 | 0 | 0 |
| Somalia | 15 (0.59%) | 0 | 0 | 0 | 0 | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sudan | 3 (0.12%) | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Togo | 3 (0.12%) | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 |
| Tunisia | 26 (1.02%) | 0 | 12 | 5 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 2 | 1 |
| Not available | 21 (0.83%) | 2 | 0 | 1 | 0 | 0 | 8 | 0 | 4 | 2 | 1 | 0 | 3 |
[i] A = Arena; B = Barletta; C = Borgo Tressanti; D = Contrada Cicerone; E = Madonna di Ripalta; F = Pista; G = San Carlo d’Ascoli; H = Sankara; I = Terlizzi; J = Terraneo; K = Turi; L = Uliveto.
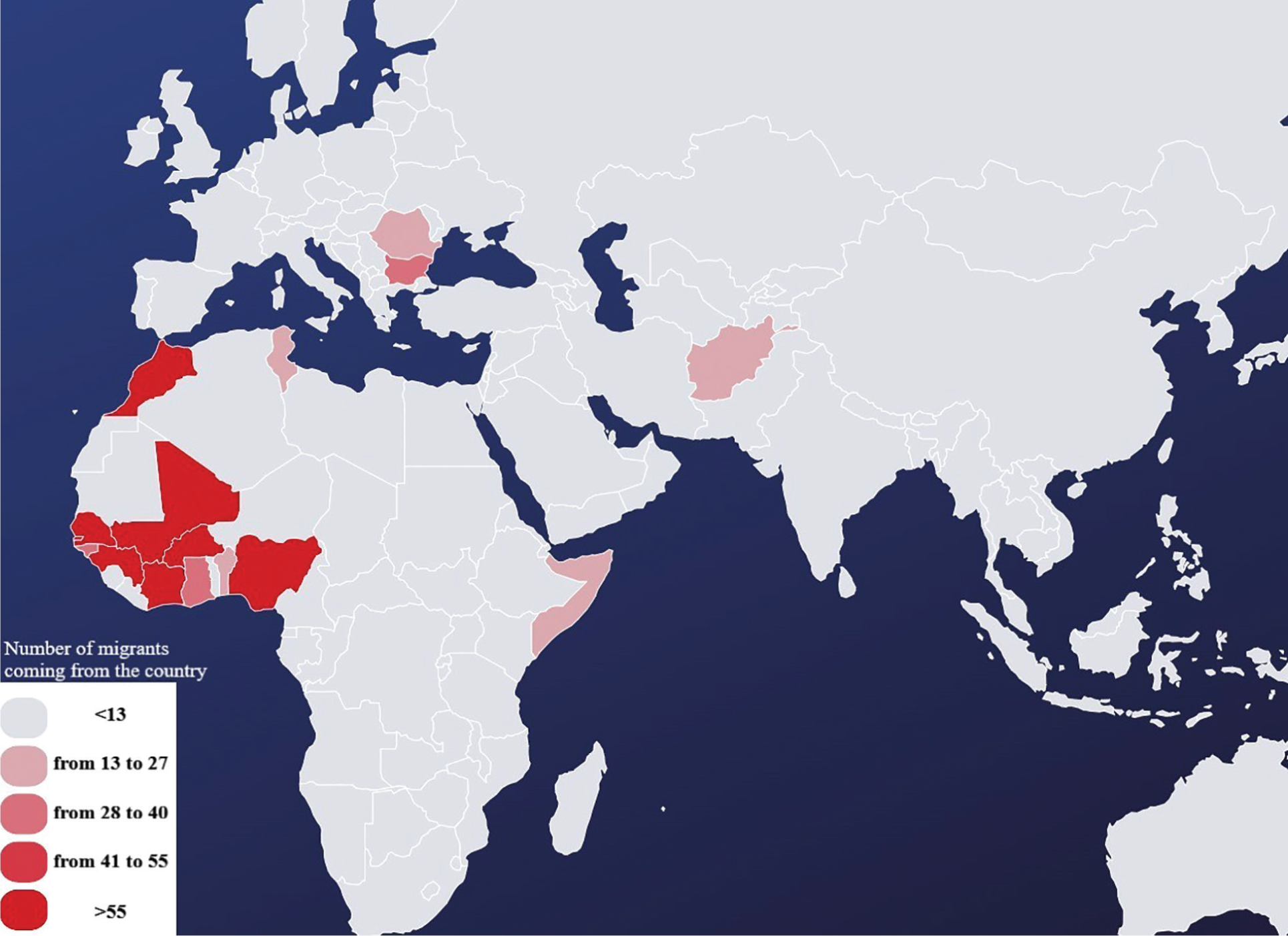
Figure 3
Countries of origins.
Socio‑Health access
More than half of the patients (52.3%) were aged 30–45 years, followed by 19–29 years (30.9%) and 46–65 years (12.5%) (Table 3). Only 17.9% of patients had residence permits, and a mere 7.3% had access to a general practitioner. Access to healthcare also varied across settlements. Long‑term data collection (2017–2023) was available for Casa Sankara and Arena, while settlements such as Barletta and Uliveto contributed data only in recent years (Table 3).
Table 3
Distribution by settlement of age at first visit, presence of residence permit, presence of GP, and year of first visit.
| AGE IN YEARS | TOTAL (%) | A | B | C | D | E | F | G | H | I | J | K | L |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–18 | 42 (1.66%) | 1 | 0 | 8 | 0 | 6 | 4 | 0 | 3 | 1 | 9 | 1 | 9 |
| 19–29 | 783 (30.86%) | 88 | 7 | 8 | 31 | 13 | 288 | 1 | 242 | 41 | 10 | 36 | 18 |
| 30–45 | 1,327 (52.31%) | 169 | 6 | 34 | 118 | 31 | 454 | 3 | 345 | 14 | 38 | 103 | 12 |
| 46–65 | 317 (12.50%) | 12 | 2 | 14 | 18 | 32 | 72 | 2 | 51 | 6 | 35 | 71 | 2 |
| Over 65 | 19 (0.75%) | 0 | 0 | 2 | 0 | 0 | 6 | 1 | 4 | 1 | 1 | 4 | 0 |
| Not available | 49 (1.93%) | 6 | 0 | 2 | 1 | 0 | 19 | 0 | 5 | 0 | 3 | 8 | 5 |
| Median | 29.7 | 29.5 | 28.9 | 35.6 | 32.6 | 40.2 | 26.9 | 45.0 | 28.9 | 26.0 | 39.8 | 36.7 | 25.5 |
| Average (SD) | 31.8 (10.4) | 30.7 (6.8) | 31.1 (8.3) | 35.6 (14.3) | 34.00 (7.8) | 39.2 (13.9) | 28.9 (8.4) | 49.5 (21.2) | 30.9 (8.7) | 29.7 (9.8) | 39.1 (14.8) | 39.5 (13.4) | 29.1 (12.6) |
| RESIDENCE PERMIT | TOTAL (%) | A | B | C | D | E | F | G | H | I | J | K | L |
| Absent | 2,083 (82.10%) | 191 | 15 | 60 | 71 | 69 | 838 | 7 | 452 | 59 | 62 | 210 | 46 |
| Present | 454 (17.90%) | 85 | 0 | 8 | 97 | 13 | 5 | 0 | 198 | 4 | 34 | 13 | 0 |
| GENERAL PRATICTIONER | TOTAL (%) | A | B | C | D | E | F | G | H | I | J | K | L |
| Absent | 2,352 (92.71%) | 258 | 15 | 66 | 160 | 82 | 733 | 7 | 614 | 63 | 89 | 221 | 44 |
| Present | 185 (7.29%) | 18 | 0 | 2 | 8 | 0 | 110 | 0 | 36 | 0 | 7 | 2 | 2 |
| YEAR OF FIRST VISIT | TOTAL (%) | A | B | C | D | E | F | G | H | I | J | K | L |
| 2017 | 97 (3.82%) | 16 | 0 | 0 | 0 | 0 | 33 | 0 | 48 | 0 | 0 | 0 | 0 |
| 2018 | 574 (22.63%) | 41 | 0 | 0 | 0 | 0 | 408 | 0 | 125 | 0 | 0 | 0 | 0 |
| 2019 | 447 (17.62%) | 26 | 0 | 0 | 0 | 0 | 334 | 0 | 87 | 0 | 0 | 0 | 0 |
| 2020 | 465 (18.33%) | 111 | 0 | 0 | 62 | 0 | 68 | 0 | 190 | 0 | 34 | 0 | 0 |
| 2021 | 243 (9.58%) | 43 | 0 | 0 | 74 | 0 | 0 | 0 | 77 | 0 | 49 | 0 | 0 |
| 2022 | 338 (13.32%) | 17 | 15 | 0 | 19 | 53 | 0 | 1 | 60 | 0 | 12 | 161 | 0 |
| 2023 | 373 (14.70%) | 22 | 0 | 68 | 13 | 29 | 0 | 6 | 63 | 63 | 1 | 62 | 46 |
[i] A = Arena; B = Barletta; C = Borgo Tressanti; D = Contrada Cicerone; E = Madonna di Ripalta; F = Pista; G = San Carlo d’Ascoli; H = Sankara; I = Terlizzi; J = Terraneo; K = Turi; L = Uliveto.
Clinical conditions
At the first visit, fatigue‑related syndromes and musculoskeletal disorders were the most frequently diagnosed conditions, affecting 27.3% of patients, followed by gastrointestinal issues (14.7%), respiratory infections (14.3%), dermatological conditions (12.1%), and cardiovascular diseases (8.2%) (Table 6). Chronic conditions such as hypertension (3.5%), diabetes (0.9%), and asthma or chronic bronchitis (1.2%) were less common. Among infectious diseases, tuberculosis (TB) (0.9%) was the most prevalent, followed by hepatitis B virus (HBV) (0.4%), hepatitis C virus (0.1%), and HIV (0.2%) (Table 4). In total, seven cases of neoplasms were identified, including in one patient suffering from osteosarcoma of the right lower limb and in one patient suffering from sarcoma of the jaw. Both patients were followed up with by the CUAMM doctors during the therapeutic process.
Table 4
Distribution by location of clinical characteristics recorded at the first visit.
| PATHOLOGY | TOTAL (%) | A | B | C | D | E | F | G | H | I | J | K | L |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetes | |||||||||||||
| Absent | 2,514 (99.09%) | 273 | 15 | 66 | 167 | 82 | 840 | 7 | 644 | 62 | 93 | 221 | 44 |
| Present | 23 (0.91%) | 3 | 0 | 2 | 1 | 0 | 3 | 0 | 6 | 1 | 3 | 2 | 2 |
| High blood pressure | |||||||||||||
| Absent | 2,448 (96.49%) | 269 | 15 | 65 | 158 | 79 | 831 | 5 | 620 | 63 | 83 | 215 | 45 |
| Present | 89 (3.51%) | 7 | 0 | 3 | 10 | 3 | 12 | 2 | 30 | 0 | 13 | 8 | 1 |
| “Fatigue” pathologies | |||||||||||||
| Absent | 2,036 (80.25%) | 229 | 15 | 56 | 134 | 64 | 624 | 5 | 531 | 52 | 84 | 206 | 36 |
| Present | 501 (19.75%) | 47 | 0 | 12 | 34 | 18 | 219 | 2 | 119 | 11 | 12 | 17 | 10 |
| Asthma or chronic bronchitis | |||||||||||||
| Absent | 2,507 (98.82%) | 273 | 15 | 67 | 168 | 82 | 836 | 7 | 636 | 63 | 96 | 220 | 44 |
| Present | 30 (1.18%) | 3 | 0 | 1 | 0 | 0 | 7 | 0 | 14 | 0 | 0 | 3 | 2 |
| Tubercolosis | |||||||||||||
| Absent | 2,515 (99.13%) | 274 | 15 | 68 | 168 | 82 | 837 | 7 | 637 | 63 | 96 | 222 | 46 |
| Present | 22 (0.87%) | 2 | 0 | 0 | 0 | 0 | 6 | 0 | 13 | 0 | 0 | 1 | 0 |
| HIV | |||||||||||||
| Absent | 2,531 (99.76%) | 273 | 15 | 68 | 167 | 81 | 843 | 7 | 649 | 63 | 96 | 223 | 46 |
| Present | 6 (0.24%) | 3 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| HBV | |||||||||||||
| Absent | 2,528 (99.65%) | 273 | 15 | 68 | 168 | 82 | 841 | 7 | 646 | 63 | 96 | 223 | 46 |
| Present | 9 (0.35%) | 3 | 0 | 0 | 0 | 0 | 2 | 0 | 4 | 0 | 0 | 0 | 0 |
| HCV | |||||||||||||
| Absent | 2,534 (99.88%) | 275 | 15 | 68 | 168 | 82 | 843 | 7 | 648 | 63 | 96 | 223 | 46 |
| Present | 3 (0.12%) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
[i] A = Arena; B = Barletta; C = Borgo Tressanti; D = Contrada Cicerone; E = Madonna di Ripalta; F = Pista; G = San Carlo d’Ascoli; H = Sankara; I = Terlizzi; J = Terraneo; K = Turi; L = Uliveto.
Visits
Over the study period, a total of 13,103 visits were conducted, with male patients accounting for 97.8% and female patients 2.2% (Table 5). The average number of visits per patient was 5.16, with the highest averages recorded in Arena (9.6 visits per patient) and Casa Sankara (8.18 visits per patient). Figure 4 illustrates the frequency of visits per patient, showing that 90% attended a maximum of 11 visits, while 42.5% had more than 2 visits. Table 6 shows the distribution of pathologies by settlement.
Table 5
Distribution of the number of visits by settlement.
| MALES N (%) 12,809 (97.8%) | FEMALE N (%) 294 (2.2%) | TOTAL N (%) 13,103 (100%) | AVERAGE NUMBER OF VISITS PER PATIENT 5.16 | |
|---|---|---|---|---|
| Arena | 2,647 (99.9%) | 3 (0.1%) | 2,650 (20.2%) | 9.6 |
| Barletta | 40 (100%) | 0 (0%) | 40 (0.3%) | 2.67 |
| Borgo Tressanti | 127 (66.1%) | 65 (33.9%) | 192 (1.5%) | 2.82 |
| Contrada Cicerone | 1,062 (99.7%) | 3 (0.3%) | 1,065 (8.1%) | 6.34 |
| Madonna di Ripalta | 410 (94%) | 26 (6%) | 436 (3.3%) | 5.32 |
| Pista | 1,517 (91.1%) | 148 (8.9%) | 1,665 (12.7%) | 1.98 |
| San Carlo d’Ascoli | 51 (100%) | 0 (0%) | 51 (0.4%) | 7.29 |
| Sankara | 5,281 (99.4%) | 34 (0.6%) | 5,315 (40.6%) | 8.18 |
| Terlizzi | 160 (100%) | 0 (0%) | 160 (1.2%) | 2.54 |
| Terraneo | 785 (98.1%) | 15 (1.9%) | 800 (6.1%) | 8.33 |
| Turi | 653 (100%) | 0 (0%) | 653 (5%) | 2.93 |
| Uliveto | 76 (100%) | 0 (0%) | 76 (0.6%) | 1.65 |
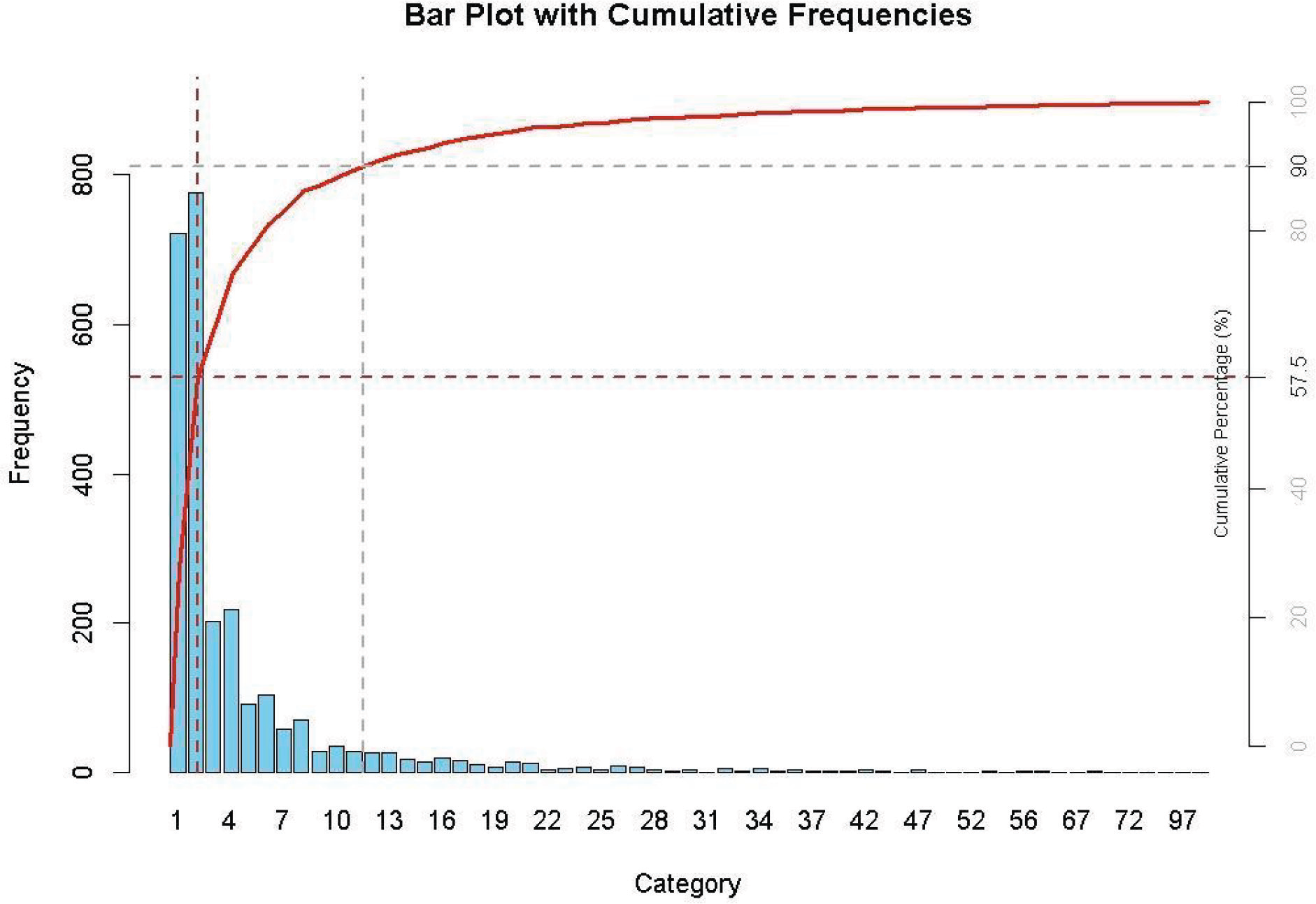
Figure 4
Pareto chart of total number of visits per patient.
Table 6
Distribution of pathologies by settlement.
| DIAGNOSIS N (%) | A 1,217 (17.9%) | B 18 (0.3%) | C 129 (1.9%) | D 461 (6.8%) | E 218 (3.2%) | F 1,170 (17.2%) | G 26 (0.4%) | H 2,710 (40%) | I 96 (1.4%) | J 331 (4.9%) | K 350 (5.2%) | L 57 (0.8%) | TOTAL 6,783 (100%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fatigue disorders (tiredness and osteoarticular disorders) | 297 (24.4%) | 5 (27.8%) | 36 (27.9%) | 125 (27.1%) | 82 (37.6%) | 334 (28.6%) | 11 (42.3%) | 775 (28.6%) | 23 (23.9%) | 66 (20.0%) | 86 (24.6%) | 16 (28.1%) | 1,856 (27.3%) |
| Gastrointestinal disorders | 180 (14.8%) | 1 (5.6%) | 11 (8.5%) | 81 (17.6%) | 23 (10.6%) | 225 (19.2%) | 0 (0%) | 412 (15.2%) | 4 (4.2%) | 14 (4.2%) | 47 (13.4%) | 2 (3.5%) | 1,000 (14.7%) |
| Airways pathologies | 158 (13%) | 2 (11.1%) | 21 (16.3%) | 52 (11.3%) | 19 (8.7%) | 207 (17.7%) | 1 (3.8%) | 421 (15.5%) | 19 (19.8%) | 21 (6.3%) | 37 (10.6%) | 9 (15.8%) | 967 (14.3%) |
| Dermatological | 174 (14.3%) | 4 (22.2%) | 8 (6.2%) | 90 (19.5%) | 22 (10.1%) | 120 (10.3%) | 1 (3.8%) | 279 (10.3%) | 25 (26%) | 41 (12.4%) | 46 (13.1%) | 13 (22.8%) | 823 (12.1%) |
| Cardiovascular | 70 (5.8%) | 2 (11.1%) | 15 (11.6%) | 44 (9.5%) | 37 (17%) | 31 (2.6%) | 10 (38.5%) | 201 (7.4%) | 0 (0%) | 119 (36%) | 24 (6.9%) | 2 (3.5%) | 555 (8.2%) |
| Dental problems | 109 (9%) | 1 (5.6%) | 7 (5.4%) | 26 (5.6%) | 5 (2.3%) | 103 (8.8%) | 0 (0%) | 186 (6.9%) | 8 (8.3%) | 9 (2.7%) | 32 (9.1%) | 4 (7%) | 490 (7.2%) |
| Traumas | 91 (7.5%) | 1 (5.6%) | 2 (1.6%) | 9 (2%) | 5 (2.3%) | 40 (3.4%) | 2 (7.7%) | 134 (4.9%) | 5 (5.2%) | 12 (3.6%) | 17 (4.9%) | 6 (10.5%) | 324 (4.8%) |
| Ophthalmological | 56 (4.6%) | 1 (5.6%) | 4 (3.1%) | 21 (4.6%) | 10 (4.6%) | 35 (3%) | 1 (3.8%) | 100 (3.7%) | 4 (4.2%) | 25 (7.6%) | 34 (9.7%) | 2 (3.5%) | 293 (4.3%) |
| Urinary tract | 31 (2.5%) | 0 (0%) | 2 (1.6%) | 3 (0.7%) | 5 (2.3%) | 31 (2.6%) | 0 (0%) | 31 (1.1%) | 0 (0%) | 4 (1.2%) | 10 (2.9%) | 0 (0%) | 117 (1.7%) |
| ENT pathologies | 20 (1.6%) | 1 (5.6%) | 2 (1.6%) | 4 (0.9%) | 5 (2.3%) | 5 (0.4%) | 0 (0%) | 42 (1.5%) | 1 (1%) | 0 (0%) | 6 (1.7%) | 0 (0%) | 86 (1.3%) |
| Diabetes and endocrinological disorders | 4 (0.3%) | 0 (0%) | 14 (10.9%) | 4 (0.9%) | 1 (0.5%) | 4 (0.3%) | 0 (0%) | 23 (0.8%) | 3 (3,1%) | 18 (5.4%) | 5 (1.4%) | 2 (3.5%) | 78 (1.2%) |
| Neuropsychiatric disorders | 16 (1%) | 0 (0%) | 5 (3.9%) | 1 (0.2%) | 1 (0.5%) | 5 (0.5%) | 0 (0%) | 31 (1.1%) | 3 (3.1%) | 2 (0.6%) | 5 (1.4%) | 1 (1.8%) | 70 (1.1%) |
| TB | 6 (0.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 6 (0.5%) | 0 (0%) | 26 (1%) | 0 (0%) | 0 (0%) | 1 (0.3%) | 0 (0%) | 39 (0.6%) |
| Rheumatological | 2 (0.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.1%) | 0 (0%) | 35 (1.3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 38 (0.6%) |
| Obstetric‑gynecological | 0 (0%) | 0 (0%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 23 (2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 24 (0.4%) |
| HIV | 3 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | 3 (1.4%) | 0 (0%) | 0 (0%) | 2 (0.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 9 (0.1%) |
| Oncological | 0 (0%) | 0 (0%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 5 (0.2%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (0.1%) |
| Hematological | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (0.3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (0.1%) |
[i] A = Arena; B = Barletta; C = Borgo Tressanti; D = Contrada Cicerone; E = Madonna di Ripalta; F = Pista; G = San Carlo d’Ascoli; H = Sankara; I = Terlizzi; J = Terraneo; K = Turi; L = Uliveto; ENT = ears, nose, and throat.
Treatments
The most frequently prescribed therapies included anti‑inflammatory drugs (33.6%), topical treatments (11.5%), supplements (10.7%), and gastroprotective agents (6.8%) (Table 7). Treatments varied by condition. For fatigue‑related syndromes, 76% of patients received anti‑inflammatory drugs. Gastroprotective agents were the primary treatment for gastrointestinal disorders (52%), while dermatological conditions were primarily addressed with topical treatments (57%).
Table 7
Therapies administered.
| THERAPIES N (%) | A 1,217 (17.9%) | B 18 (0.3%) | C 129 (1.9%) | D 461 (6.8%) | E 218 (3.2%) | F 1,170 (17.2%) | G 26 (0.4%) | H 2,710 (40%) | I 96 (1.4%) | J 331 (4.9%) | K 350 (5.2%) | L 57 (0.8%) | TOTAL 6,783 (100%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NSAIDs, painkillers and cortisone | 394 (30.9%) | 5 (27.8%) | 29 (22.5%) | 132 (28.7%) | 66 (30.3%) | 478 (40.9%) | 10 (38.4%) | 951 (35.1%) | 33 (34.3%) | 70 (21.1%) | 97 (27.7%) | 7 (12.3%) | 2272 (33.6%) |
| Topicals (creams and eye drops) | 159 (13.1%) | 2 (11.1%) | 7 (5.4%) | 70 (15.2%) | 34 (15.6%) | 122 (10.4%) | 0 (0%) | 296 (10.9%) | 17 (17.7%) | 42 (12.7%) | 21 (6%) | 12 (21.1%) | 782 (11.5%) |
| Adjuvants, supplements, and probiotics | 122 (10%) | 3 (16.7%) | 13 (10.1%) | 62 (13.4%) | 30 (13.8%) | 103 (8.8%) | 2 (7.7%) | 300 (11.1%) | 7 (7.3%) | 30 (9.1%) | 47 (13.4%) | 7 (12.3%) | 726 (10.7%) |
| Gastrointestinal | 99 (8.1%) | 1 (5.6%) | 6 (4.7%) | 44 (9.5%) | 12 (5.6%) | 137 (11.7%) | 0 (0%) | 229 (8.4%) | 3 (3.1%) | 6 (1.8%) | 30 (8.5%) | 1 (1.8%) | 568 (8.3%) |
| Antibiotics, antifungals, and antiparasitics | 102 (8.4%) | 0 (0%) | 13 (10.1%) | 25 (5.4%) | 5 (2.3%) | 136 (11.6%) | 1 (3.8%) | 189 (7.0%) | 18 (18.8%) | 10 (3.0%) | 22 (6.3%) | 8 (14.0%) | 529 (7.9%) |
| Cardiovascular (antihypertensives, diuretics, and anticoagulants) | 56 (4.5%) | 0 (0%) | 10 (7.8%) | 28 (6.1%) | 27 (12.5%) | 30 (2.6%) | 10 (38.5%) | 161 (5.9%) | 0 (0%) | 102 (30.8%) | 18 (5.2%) | 1 (1.8%) | 443 (6.5%) |
| Respiratory tract treatments | 75 (6.1%) | 2 (11.1%) | 11 (8.6%) | 15 (3.2%) | 1 (0.5%) | 80 (6.8%) | 1 (3.8%) | 193 (7.1%) | 5 (5.2%) | 13 (3.9%) | 28 (8.0%) | 4 (7.1%) | 428 (6.3%) |
| Medication | 38 (3.1%) | 0 (0%) | 1 (0.8%) | 14 (3%) | 1 (0.5%) | 14 (1.2%) | 2 (7.7%) | 61 (2.3%) | 1 (1%) | 8 (2.4%) | 13 (3.7%) | 5 (8.8%) | 158 (2.3%) |
| Antidiabetics | 1 (0.1%) | 0 (0%) | 12 (9.4%) | 1 (0.2%) | 1 (0.5%) | 2 (0.2%) | 0 (0%) | 17 (0.7%) | 2 (2.0%) | 15 (4.5%) | 3 (0.9%) | 2 (3.6%) | 56 (1.0%) |
| Neurological | 0 (0%) | 0 (0%) | 1 (0.8%) | 1 (0.2%) | 0 (0%) | 3 (0.3%) | 0 (0%) | 3 (0.1%) | 1 (1%) | 0 (0%) | 2 (0.6%) | 0 (0%) | 11 (0.2%) |
| Health orientation and hospital care | 3 (0.3%) | 0 (0%) | 0 (0%) | 1 (0.2%) | 0 (0%) | 1 (0.1%) | 0 (0%) | 11 (0.4%) | 0 (0%) | 1 (0.3%) | 1 (0.3%) | 0 (0%) | 18 (0.2%) |
| Not available | 168 (13.8%) | 5 (27.8%) | 26 (20.2%) | 68 (14.8%) | 41 (18.8%) | 64 (5.5%) | 0 (0%) | 299 (11%) | 9 (9.4%) | 34 (10.3%) | 68 (19.4%) | 10 (17.5%) | 792 (11.7%) |
[i] A = Arena; B = Barletta; C = Borgo Tressanti; D = Contrada Cicerone; E = Madonna di Ripalta; F = Pista; G = San Carlo d’Ascoli; H = Sankara; I = Terlizzi; J = Terraneo; K = Turi; L = Uliveto; NSAIDs = nonsteroidal anti‑inflammatory drugs.
Follow‑Up visits
The likelihood of follow‑up visits, considered a proxy for trust in the socio‑healthcare services provided by volunteers of Doctors with Africa CUAMM, was analyzed using logistic regression (Table 8). Compared with the reference settlement, Casa Sankara, which had the highest total number of visits, the settlements Arena, Contrada Cicerone, and Terraneo showed significantly higher odds of follow‑up visits. Specifically, the increases were +22% (OR = 2.22; 95% CI: 1.12–1.34; p < 0.001), +36% (OR = 1.36; 95% CI: 1.19–1.56; p < 0.001), and +47% (OR = 1.47; 95% CI: 1.27–1.71; p < 0.001), respectively.
Table 8
Simple logistic regression (unadjusted OR) and multiple logistic regression (adjusted OR) on the probability of returning to the visit with respect to the reference settlement Casa Sankara.
| UNADJUSTED ORS | ADJUSTED OR | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P‑VALUE | OR | 95% CI | P‑VALUE | |
| Settlements | ||||||
| Sankara (H) | ref. | – | – | ref. | – | – |
| Arena (A) | 1.22 | 1.12–1.34 | <0.001 | 1.16 | 1.06–1.28 | 0.002 |
| Barletta (B) | 1.27 | 0.68–2.38 | 0.451 | 1.92 | 1.01–3.65 | 0.045 |
| Borgo Tressanti (C) | 0.51 | 0.37–0.69 | 0.018 | 0.70 | 0.49–1.01 | 0.055 |
| Contrada Cicerone (D) | 1.36 | 1.19–1.56 | <0.001 | 1.34 | 1.18–1.54 | <0.001 |
| Madonna di Ripalta (E) | 1.04 | 0.86–1.26 | 0.692 | 1.64 | 1.29–2.09 | 0.001 |
| Pista (F) | 0.45 | 0.39–0.50 | <0.001 | 0.40 | 0.36–0.46 | <0.001 |
| San Carlo d’Ascoli (G) | 1.00 | 0.58–1.74 | 0.999 | 0.96 | 0.50–1.82 | 0.897 |
| Terlizzi (I) | 0.69 | 0.50–0.96 | 0.025 | 1.02 | 0.71–1.45 | 0.932 |
| Terraneo (J) | 1.47 | 1.27–1.71 | <0.001 | 1.39 | 1.18–1.64 | 0.001 |
| Turi (K) | 0.90 | 0.77–1.06 | 0.208 | 1.41 | 1.14–1.76 | 0.002 |
| Uliveto (L) | 0.35 | 0.21–0.58 | <0.001 | 0.52 | 0.29–0.93 | 0.027 |
| Gender | ||||||
| Male | ref. | – | – | ref. | – | – |
| Female | 0.71 | 0.56–0.90 | 0.005 | 1.10 | 0.83–1.44 | 0.514 |
| Age range at first visit (years) | ||||||
| 0–18 | ref. | – | – | ref. | – | – |
| 19–29 | 0.86 | 0.60–1.23 | 0.401 | 1.00 | 0.67–1.50 | 0.987 |
| 30–45 | 0.81 | 0.57–1.17 | 0.264 | 0.93 | 0.62–1.39 | 0.729 |
| 46–64 | 0.84 | 0.58–1.21 | 0.345 | 0.87 | 0.58–1.30 | 0.492 |
| 65+ | 0.61 | 0.34–1.08 | 0.087 | 0.92 | 0.50–1.71 | 0.804 |
| Country of origin | ||||||
| Other nations | ref. | – | – | ref. | – | – |
| Romania | 2.88 | 1.80–4.6 | <0.001 | 3.09 | 1.79–5.34 | <0.001 |
| Year of first visit | ||||||
| <2022 | ref. | – | – | ref. | – | – |
| 2022–2023 | 0.76 | 0.70–0.83 | <0.001 | 0.60 | 0.52–0.70 | <0.001 |
| Diagnosis of TB | ||||||
| No | ref. | – | – | ref. | – | – |
| Yes | 0.63 | 0.49–0.81 | <0.001 | 0.63 | 0.49–0.81 | <0.001 |
[i] CI = confidence interval; OR = odds ratio
In contrast, settlements such as Borgo Tressanti, Pista, Terlizzi, and Uliveto had significantly lower odds of follow‑up visits compared with Casa Sankara. The decreases were −49% (OR = 0.51; 95% CI: 0.37–0.69; p = 0.018), −55% (OR = 0.45; 95% CI: 0.39–0.50; p < 0.001), −31% (OR = 0.69; 95% CI: 0.50–0.96; p = 0.025), and −65% (OR = 0.35; 95% CI: 0.21–0.58; p < 0.001), respectively.
When additional variables were controlled for in the multiple logistic regression model, statistical significance was maintained for Arena (+16%; OR = 1.16; p = 0.002), Contrada Cicerone (+34%; OR = 1.34; p < 0.001), Terraneo (+39%; OR = 1.39; p = 0.001), and Uliveto (− 48%; OR = 0.52; p = 0.027). However, settlements such as Borgo Tressanti (p = 0.055) and Terlizzi (p = 0.932) lost statistical significance, suggesting the influence of confounding factors.
Further analysis revealed that settlements such as Barletta (OR = 1.92; 95% CI: 1.01–3.65; p = 0.045), Madonna di Ripalta (OR = 1.64; 95% CI: 1.29–2.09; p = 0.001), and Turi (OR = 1.41; 95% CI: 1.14–1.76; p = 0.002) had significantly higher odds of follow‑up visits compared with Casa Sankara. Regarding gender, female patients were significantly less likely to attend follow‑up visits compared with male patients (p = 0.005).
For a better understanding, see Figure 1, where you will find a map of the informal settlements covered by the analysis. The most widespread nationality of migrants living in each settlement is indicated.
Discussion
This study aims to highlight the health needs and social conditions of migrant agricultural workers in Puglia’s informal settlements, often overlooked by institutions. By analyzing 13,103 visits from 2,537 patients, the research emphasizes critical health and socio‑health issues, offering valuable insights for targeted interventions. Addressing these needs is not only a healthcare matter but also a step toward social inclusion and justice. The predominance of male patients (95.8%) reflects both demographic trends and cultural barriers limiting women’s healthcare access. Migrant men dominate sectors such as agriculture, construction, and logistics, while women are typically employed in domestic or care work in urban areas. The central Mediterranean migration route, one of the most dangerous, discourages families from sending women owing to the higher risks of violence and exploitation [10]. Even when women seek healthcare, their follow‑up rates are lower, possibly owing to discomfort, fear of judgment, or the prioritization of family needs over their own health.
Most patients (85%) come from sub‑Saharan African countries such as Senegal, Gambia, and Mali, regions marked by poverty, instability, and limited opportunities that drive migration through dangerous routes such as Libya and the Mediterranean [10]. Only 18% of patients had residence permits, often owing to exploitation practices such as document confiscation by labor intermediaries (caporali). This perpetuates exclusion from healthcare, as fear of deportation discourages migrants from seeking medical help [11, 12].
Despite Italy’s universal healthcare system, only 7% of patients had a general practitioner. This is due to low awareness of healthcare rights and difficulties in obtaining the Temporarily Present Foreigner (STP) Code, which is necessary for accessing basic services. Migrants’ limited health literacy and marginalization further exacerbate this gap [13, 14].
The study highlights the burden of work‑related health issues. Fatigue syndromes and musculoskeletal pain made up over 27% of visits, reflecting harsh working conditions rather than age‑related issues. Injuries and trauma (5% of visits) align with literature on workplace hazards faced by migrants [6, 15, 16]. Poor hygiene and overcrowding contributed to frequent respiratory infections (14.3%), dermatological issues (12.1%), and dental problems (7.2%). Additionally, indoor use of charcoal and waste‑burning increased respiratory risks.
Infectious diseases such as hepatitis B and C, tuberculosis, and HIV were found at low rates, consistent with existing data on migrant populations [17–19]. However, given the high‑risk conditions in informal settlements and the limited availability of diagnostic resources, underreporting cannot be excluded. Previous CUAMM studies and external sources have reported higher prevalence rates in similar contexts, suggesting that systematic screening efforts might reveal a greater disease burden than observed in our dataset [20–22].
Periodic checks made it possible to diagnose seven cases of neoplasms, which would have come to the attention of public health workers at a late stage. The young age of migrants helps to explain the low prevalence of chronic diseases such as hypertension and diabetes.
The high prescription rates of anti‑inflammatory drugs (33.6%) reflect work‑related conditions, while supplements and gastroprotective agents address issues tied to poor nutrition, stress, and heavy nonsteroidal anti‑inflammatory drug (NSAID) use. Despite limited resources, the high follow‑up rate (average of 5.6 visits per patient) shows trust in CUAMM’s mobile clinics, especially in settlements such as Arena and Casa Sankara, where collaboration with local communities boosted engagement [23]. One key finding is the need to incorporate health and migration training in medical education. As the World Health Organization (WHO) recommends, healthcare professionals should be equipped to address the complex needs of migrant populations, including cultural dynamics and language barriers and building trust with vulnerable groups [24]. Without this training, providers risk perpetuating gaps in access and care quality for migrants [24–26]. Another fundamental objective would be to guarantee that migrants are taken into care even after their stay in the ghettos has ended, when they are no longer intercepted by CUAMM doctors and cultural mediators.
Study limitations include the heterogeneity of settlements and reliance on clinical diagnoses, which may have missed conditions requiring advanced diagnostics, such as diabetes, tuberculosis, and cancers. Furthermore, it was not possible to carry out systematic mental health screening, despite the literature [27, 28] indicating that migrants suffer more often from mental disorders than the host population. The lack of structured mental health data represents a gap that will be addressed in future healthcare interventions. Specifically, upcoming medical visits will integrate a targeted mental health assessment program to better evaluate psychological distress and psychiatric conditions among migrant workers.
Conclusion
This study offers a comprehensive look at the health needs of migrant workers in Puglia, highlighting work‑ and living‑related health issues and barriers to accessing healthcare. It emphasizes the crucial role of CUAMM’s mobile clinics, which have become essential for isolated populations, offering primary care, referrals, and socio‑health support. To improve healthcare access, our experience suggests:
Equitable access to healthcare: Implement information campaigns on healthcare rights and ensure the assignment of general practitioners. Address barriers such as low health literacy and language differences, which disproportionately affect migrants [13, 14, 29].
Cultural competence: Train healthcare staff to address migrants’ needs, provide interpreters and cultural mediators, and develop protocols for more effective management of migrant health. Studies show that these measures significantly improve health outcomes [30–34].
Incorporating health and migration training into medical education: Healthcare curricula should include modules on health and migration, as recommended by the WHO [24]. This training will enable healthcare providers to understand the unique needs of migrant populations and reduce systemic barriers to care.
Integrated approach with institutions and partners: Strengthen collaboration between central (e.g., regional) and local institutions, including health services and administrative bodies, for a coordinated, sustainable response. Partnerships with NGOs are crucial to align actions with regional programming and offer comprehensive support to vulnerable populations. Coordinating resources and expertise can enhance the effectiveness of interventions.
Role of universities: Universities play a key role in addressing health challenges through operational research and education. Research should provide evidence‑based solutions for migrant health, while universities also equip future medical professionals with the necessary skills to manage migration‑related health issues. This dual role is vital for long‑term improvements in healthcare systems and social equity.
In conclusion, mobile clinics have proven effective in bridging gaps in healthcare access for marginalized populations, reducing logistical barriers, and creating a trusted, welcoming environment. This model should be integrated into traditional healthcare systems to extend its reach and sustainability. Finally, addressing labor exploitation is essential for improving migrant health. Better working conditions and housing would reduce health risks and promote social inclusion, facilitating continuous care access. Socio‑healthcare services must be truly integrated, fostering equality and justice for all, leaving no one behind.
Acknowledgments
A special thank you goes to the volunteers of Doctors with Africa CUAMM, whose selfless dedication and willingness to donate their time embody the highest form of generosity and humanity. We would like to express our heartfelt gratitude to the Puglia Region and the territorial health authorities (ASLs) of Bari and Foggia for their collaborative and supportive approach to safeguarding the health of migrants. Their commitment has been instrumental in fostering accessible and inclusive healthcare services. Heartfelt thanks goes to the Galeno Foundation, which believed in this research proposal, supporting it with the Cantamessa prize. We extend our deepest appreciation to Lucia Raho, the project lead of the mobile clinic, and to Dina Diurno, the cultural mediator, for their invaluable contributions. Finally, to all the migrants living in the ghettos, we honor your resilience and courage. We pledge never to take a step back in defending your right to health. We will not stop serving until each of you has the opportunity to live in dignity, with fair and just living conditions.
Conflict of Interest
The research project was carried out by volunteer doctors enlisted by the NGO Doctors with Africa for the migrant assistance service. The data collection was carried out in parallel with the clinical activities, and the healthcare activities were possible thanks to donations from private citizens and the support of the Puglia Region. Publication costs are instead supported by the University of Bari. None of the authors have any conflicts of interest nor any financial or family ties to pharmaceutical companies or medical device suppliers.
