Table 1
Characteristics of design team members (n = 20).
| Primary occupation | n (%) |
| ED nurse | 3 (15%) |
| ED Physician | 3 (15%) |
| Implementation scientist | 3 (15%) |
| Departmental administrator | 2 (10%) |
| Internal medicine physician | 2 (10%) |
| Clinical officer | 2 (10%) |
| Master’s student | 2 (10%) |
| Cardiologist | 1 (5%) |
| Social scientist | 1 (5%) |
| Ministry of health representative | 1 (5%) |
| Nationality | |
| Tanzania | 12 (60%) |
| United States | 8 (40%) |
| Gender | |
| Male | 12 (60%) |
| Female | 8 (40%) |
Table 2
Results of audit of care processes among AMI patients in the KCMC ED, 2022 (N = 75).
| CARE PROCESS | n | (%) |
|---|---|---|
| Documented diagnosis of AMI | 12 | (16) |
| Treated with aspirin | 8 | (11) |
| Survived to 30 days | 47 | (67) |
Table 3
Primary barriers to evidence-based AMI care in the KCMC ED identified from prior qualitative work [7] (publication pending).
| BARRIER | INFORMANT |
|---|---|
| Patients have limited understanding of AMI | Patients, providers, administrators |
| Providers fail to consider the diagnosis of AMI | Providers, administrators |
| Providers have insufficient training in AMI care | Providers, administrators, patients |
| Lack of designated leader(s) for improvement efforts | Providers, administrators |
Table 4
Topical expert recommendations for refinements to a quality improvement intervention for AMI care in Tanzania.
| INTERVENTION COMPONENT | REFINEMENT(S) | TOPICAL EXPERT(S) |
|---|---|---|
| Triage reminder cards | (1) Affix to a cable for easy attachment to stretchers; (2) Post list of AMI symptoms in the triage area to aid nurses in recognition of possible AMI cases | ED nurses |
| Pocket cards | Minor refinements to wording | Cardiologists, ED physicians |
| Online training modules | Minor refinements to wording | Cardiologists, implementation scientists |
| Champions | (1) Create certificates of appreciation for staff who provide excellent care; (2) Assign responsibility for ensuring adequate supply of aspirin in the ED to the nurse champion | ED nurses, ED physicians, implementation scientists |
| Patient educational pamphlets | (1) Increase font and add color; (2) Minor refinements to wording; (3) Project digital versions ofpamphlets on the screens in the waiting room | Patients, ED nurses, ED physicians |
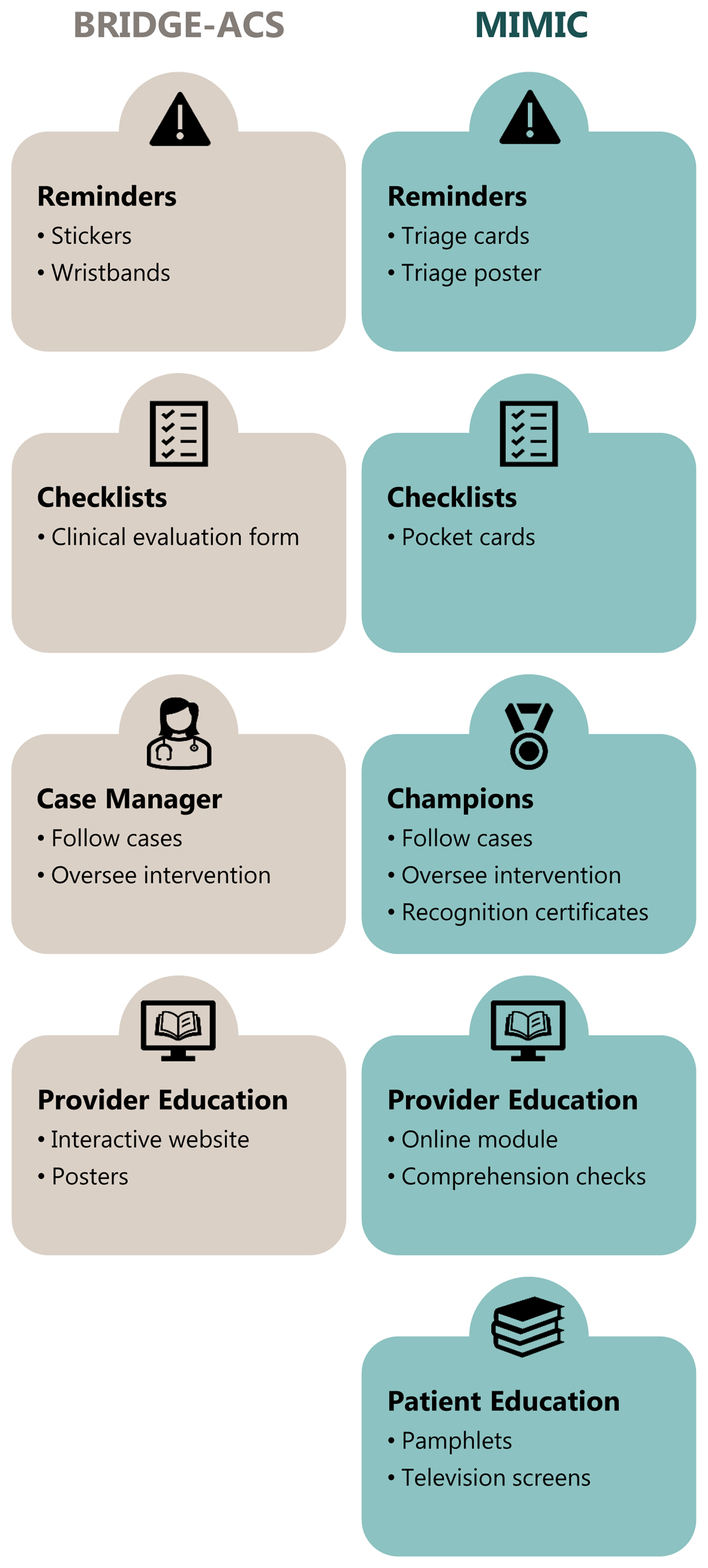
Figure 1
Adaptation of the BRIDGE-ACS intervention to the MIMIC intervention to improve AMI care in Tanzania.
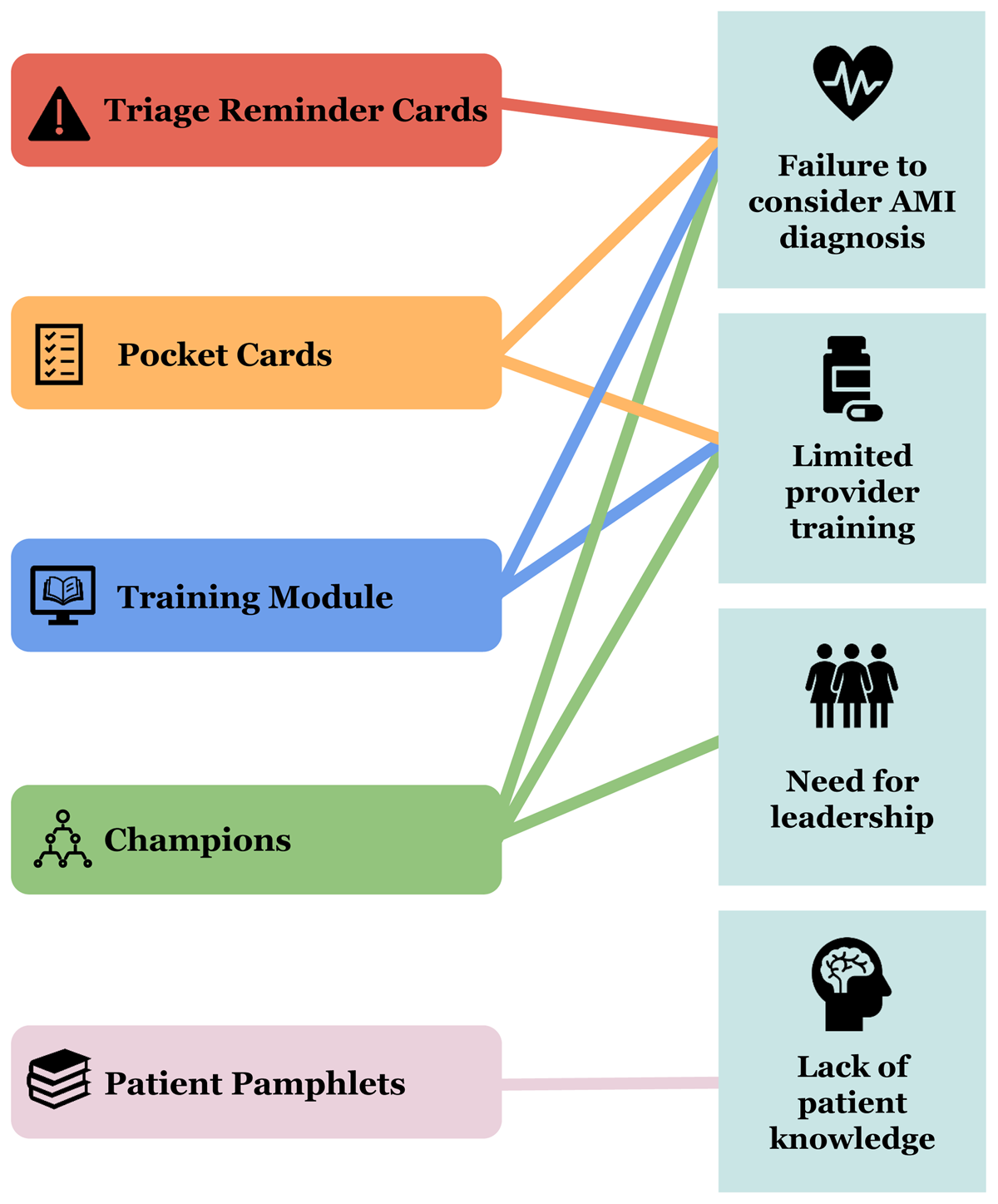
Figure 2
Mapping the MIMIC intervention to the barriers targeted by each intervention component.

Figure 3
Use of the ADAPT-ITT framework to develop a quality improvement intervention for myocardial infarction care in Tanzania.
Table 5
Summary of key findings from adaptation of an intervention to improve AMI care in Tanzania using the ADAPT-ITT framework.
| ADAPT-ITT STEP | OUR APPROACH | KEY FINDINGS |
|---|---|---|
| 1. Assessment | (a) Review previously published data describing AMI care at KCMC, (b) Audit ED care for 75 recent AMI cases, (c) Review results of provider attitudes survey, (d) Qualitative data from in-depth interviews with providers, patients, and administrators. | (a) Diagnostic workups for AMI are not routine at KCMC; (b) Most patients with AMI do not receive aspirin in the ED; (c) Providers are strongly interested in a quality improvement intervention; (d) Provider training and patient education are barriers to care. |
| 2. Decision | (a) Review systematic review of AMI quality improvement studies, (b) Conduct literature search of quality improvements strategies for AMI, (c) Convene Design Team to select an intervention that is appropriate for the local context. | Selection of the BRIDGE-ACS for adaptation to the Tanzanian context. |
| 3. Adaptation | Iterative Design Team meetings to review components of the original intervention and tailor them to the local context. | (a) Use of triage cards instead of patient wristbands; (b) transforming checklists to pocket cards; (c) use of champions instead of case managers; (d) addition of a patient educational pamphlet. |
| 4. Production | Production of draft materials for Design Team and topical expert review. Production, Topical Experts, and Integration occurred iteratively. | Minor refinements to wording of training module, pocket card, and educational pamphlet. |
| 5. Topical Experts | Input from implementation scientists, cardiologists, KCMC staff, and 5 recent AMI patients. | (a) Additional champion responsibilities created, including awarding congratulatory certificates and ensuring adequate supply of aspirin; (b) Electronic displays of educational pamphlet in the ED waiting room; (c) Additional minor refinements to educational pamphlet |
| 6. Integration | Iteratively integrated feedback from topical experts and the design team to further refine all intervention components. | Finalization of the MIMIC intervention |
| 7. Training | ED staff were trained by members of the Design Team during three staff-wide meetings. Additional training meetings held with designated champions. | Training completed in August 2023 |
| 8. Testing | Pilot trial of the MIMIC intervention to be conducted in the KCMC ED to assess acceptability, fidelity, and preliminary effect on care processes. | Results pending |
