Table 1
Characteristics of units and staff informants.
| HDUs | ICUs | |
|---|---|---|
| Unit characteristics | ||
| n | 4 | 4 |
| District hospital n (%) | 3 (75%) | 0 |
| Central hospital n (%) | 1 (25%) | 4 (100%) |
| Total beds n | 14 | 20 |
| Beds per unit median (range) | 4 (2 to 4) | 4 (4 to 8) |
| Patient types admitted | ||
| Medical adult n (%) | 4 (100%) | 4 (100%) |
| Medical pediatric n (%) | 4 (100%) | 4 (100%) |
| Surgical adult n (%) | 3 (75%) | 4 (100%) |
| Trauma adult n (%) | 3 (75%) | 3 (75%) |
| Trauma pediatric n (%) | 3 (75%) | 3 (75%) |
| Obstetrics n (%) | 3 (75%) | 4 (100%) |
| Gynecological n (%) | 3 (75%) | 4 (100%) |
| Staff informant characteristics | ||
| n | 11* | 12 |
| Nurse n (%) | 6 (55%) | 7 (58%) |
| Clinical officer n (%) | 5 (45%) | 2 (17%) |
| Doctor n (%) | 0 | 3 (25%) |
| Days per week working on unit median (IQR) | 5.0 (4.0 to 5.0) | 5.0 (5.0 to 5.0) |
[i] IQR: Interquartile range.
*One HDU had only two informants.
Table 2
Staff.
| HDUs (N = 4) | ICUs (N = 4) | |
|---|---|---|
| Units with available specialists and allied health professionals | ||
| Social work n (%) | 1 (25%) | 0 |
| Radiology results interpreted by radiologist n (%) | 1 (25%) | 2 (50%) |
| Security n (%) | 2 (50%) | 3 (75%) |
| Spiritual support n (%) | 1 (25%) | 1 (25%) |
| Dietician n (%) | 3 (75%) | 3 (75%) |
| Respiratory therapist n (%) | 1 (25%) | 4 (100%) |
| Physical therapy n (%) | 4 (100%) | 4 (100%) |
| Clinical engineering n (%) | 4 (100%) | 4 (100%) |
| Staff pool | ||
| Non-rotating nurses median (range) | 5.0 (4 to 10) | 13.5 (4 to 21) |
| Rotating nurses median (range) | 1.5 (0 to 5) | 1.0 (0 to 3) |
| Non-rotating advanced practice providers* median (range) | 0.5 (0 to 1) | 6.0 (1 to 10) |
| Rotating advanced practice providers median (range) | 3.5 (0 to 6) | 0 (0 to 0) |
| Non-rotating doctors without specialty training median (range) | 0 (0 to 1) | 0 (0 to 3) |
| Rotating doctors without specialty training median (range) | 2.0 (0 to 3) | 0 (0 to 3) |
| Non-rotating physicians specializing in critical care median (range) | 0 (0 to 0) | 1.0 (0 to 2) |
| Rotating physicians specializing in critical care median (range) | 0 (0 to 0) | 0 (0 to 0) |
| Non-rotating physicians with other specialization median (range) | 0 (0 to 0) | 0 (0 to 0) |
| Rotating physicians with other specialization median (range) | 0 (0 to 3) | 0 (0 to 3) |
| Coverage | ||
| Units with nurses available 24 hours/day n (%) | 4 (100%) | 4 (100%) |
| Units with providers physically present in unit 24 hours/day n (%) | 4 (100%) | 4 (100%) |
| Number of beds per nurse during the daytime median (range) | 2.5 (1.0 to 4.0) | 1.6 (0.8 to 2.7) |
| Number of beds per nurse overnight median (range) | 3.0 (2. 0 to 4.0) | 2.3 (1.0 to 4.0) |
| Agreement with reported staffing numbers for nurses and number of nurses working at time of visit n (%) | 3 (75%) | 1 (25%) |
[i] Non-rotating: dedicated staff working only in the critical care unit.
* Advanced practice providers include clinical officers and anesthetists.
Table 3
Critical care signal functions.
| HDUs (N = 4) | ICUs (N = 4) | |
|---|---|---|
| Airway and breathing | ||
| Bag-valve-mask ventilation n (%) | 3 (75%) | 4 (100%) |
| Surgical airway n (%) | 1 (25%) | 3 (75%) |
| Placement of supraglottic airway n (%) | 0 | 2 (50%) |
| Endotracheal intubation n (%) | 2 (50%) | 4 (100%) |
| Non-invasive ventilation n (%) | 0 | 4 (100%) |
| Invasive mechanical ventilation n (%) | 0 | 4 (100%) |
| Cardiac and circulation | ||
| Administer aspirin for ischemia n (%) | 4 (100%) | 2 (50%) |
| Perform external defibrillation and/or cardioversion n (%) | 0 | 4 (100%) |
| Administer adrenaline n (%) | 3 (75%) | 3 (75%) |
| Administer intravenous vasopressors n (%) | 1 (25%) | 3 (75%) |
| Administer inotropes n (%) | 2 (50%) | 3 (75%) |
| Administer anti-arrhythmics n (%) | 0 | 1 (25%) |
| Administer thrombolytics n (%) | 0 | 1 (25%) |
| Procedures | ||
| Place peripheral intravenous cannula n (%) | 4 (100%) | 4 (100%) |
| Establish central venous access n (%) | 1 (25%) | 2 (50%) |
| Establish intraosseous access n (%) | 0 | 0 |
| Perform venous cutdown n (%) | 0 | 0 |
| Perform paracentesis n (%) | 4 (100%) | 2 (50%) |
| Perform lumbar puncture n (%) | 4 (100%) | 4 (100%) |
| Placement of chest tube n (%) | 3 (75%) | 3 (75%) |
| Needle decompression of pneumothorax n (%) | 2 (50%) | 2 (50%) |
| Perform pericardiocentesis n (%) | 0 | 0 |
| Supportive care | ||
| Administer enteral nutrition n (%) | 4 (100%) | 4 (100%) |
| Frequently (at least every four hours) check electrolytes and adjust management based on results n (%) | 1 (25%) | 1 (25%) |
| Regularly (at least every four hours) reposition patients to prevent pressure ulcers n (%) | 4 (100%) | 4 (100%) |
| Administer stress ulcer prophylaxis n (%) | 0 | 3 (75%) |
| Administer DVT prophylaxis n (%) | 2 (50%) | 3 (75%) |
| Provide physical restraints n (%) | 4 (100%) | 4 (100%) |
| Manage extreme temperatures n (%) | 4 (100%) | 4 (100%) |
| De-escalate care (e.g., stop treatments or remove life support) for patients with poor prognoses based on the expressed goals and wishes of the patient or their families n (%) | 0 | 1 (25%) |
[i] DVT: deep vein thrombosis.
Table 4
Mechanical ventilation in ICUs.
| ICUs (N = 4) | |
|---|---|
| Functional ventilators per unit median (range) | 3.0 (2 to 8) |
| Vents per 1,000,000 population in catchment area median (range) | 0.9 (0.4 to 1.3) |
| Maintain head of bed in semi-recumbent position (30-45 degrees) to reduce aspiration and ventilator associated pneumonia n (%) | 4 (100%) |
| Administer and maintain neuromuscular blockade n (%) | 3 (75%) |
| Written policy for who can or cannot be intubated and/or placed on mechanical ventilation n (%) | 0 |
| Written policy for withdrawal of mechanical ventilation n (%) | 0 |
| ABCDEF bundle* | |
| Assess, prevent, and manage pain | |
| Assess pain in mechanically ventilated patients at least twice a day n (%) | 3 (75%) |
| Administer intravenous opioids n (%) | 4 (100%) |
| Spontaneous awakening trials and spontaneous breathing trials | |
| Perform daily spontaneous breathing trials n (%) | 3 (75%) |
| Perform daily spontaneous awakening trials n (%) | 3 (75%) |
| Analgesia and sedation | |
| Assess agitation/sedation in mechanically ventilated patients at least twice a day n (%) | 3 (75%) |
| Administer appropriate therapeutics for agitation n (%) | 4 (100%) |
| Administer intravenous sedatives n (%) | 4 (100%) |
| Delirium: Assess, prevent, and manage | |
| Assess delirium in mechanically ventilated patients at least twice a day n (%) | 1 (25%) |
| Early mobility and exercise | |
| Perform early mobilization for mechanically ventilated patients n (%) | 4 (100%) |
| Family engagement and empowerment | |
| Communicate with patient and/or families, including sharing poor prognoses n (%) | 4 (100%) |
[i] *The Society of Critical Care Medicine’s ABCDEF bundle includes: assess, prevent, and manage pain; perform spontaneous awakening trials and spontaneous breathing trials; delirium monitoring and management; early mobility and exercise; and family engagement [26].
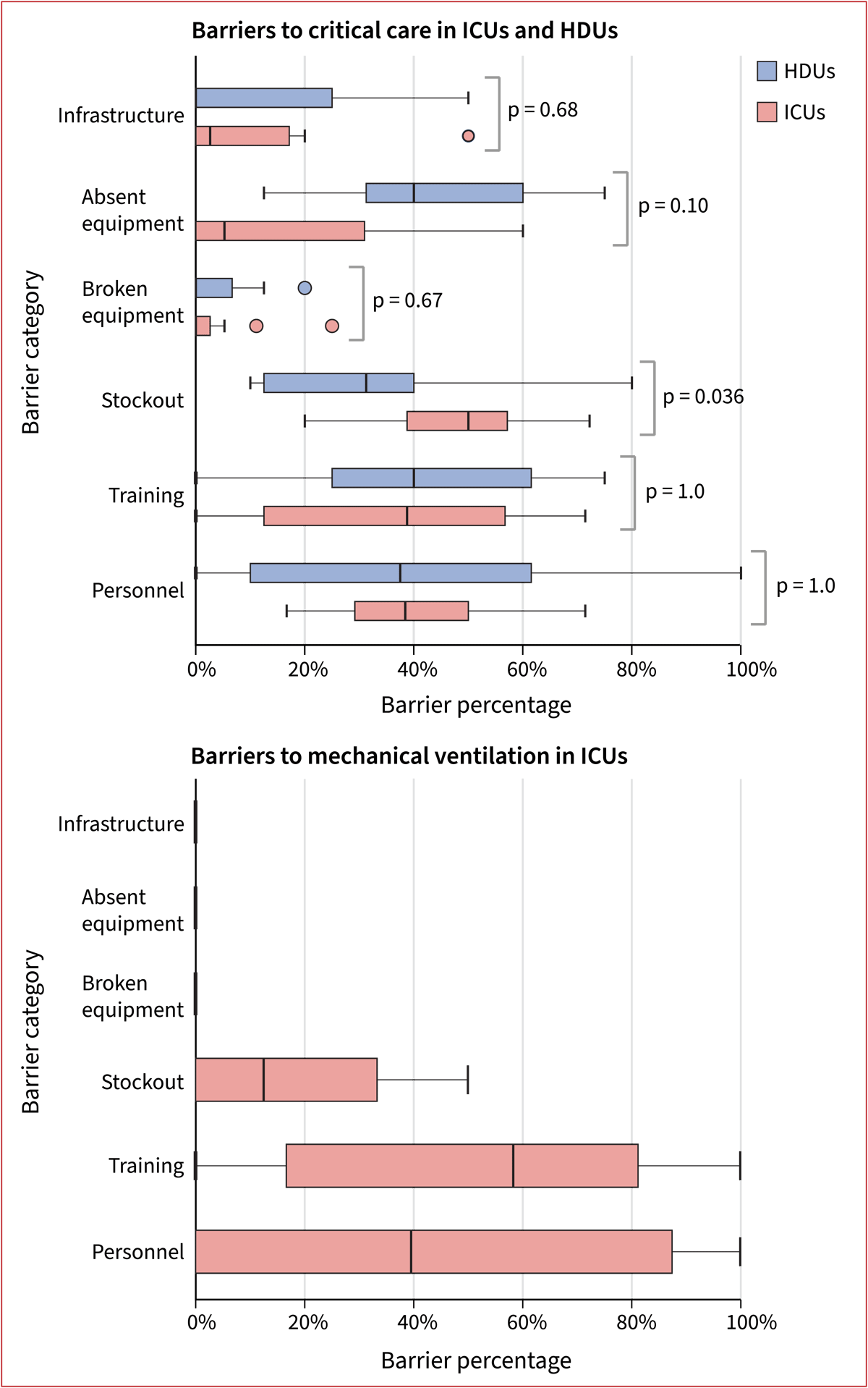
Figure 1
Barriers in critical care units: Box plots of participant level data showing relative frequencies of the six most common barrier categories in HDUs (n = 11). and ICUs (n = 12) for signal functions from Table 3 (top panel) and Table 4 (bottom panel). Estimates for each participant were calculated taking the number of times each barrier was identified by the participant divided by the number of times the participant was probed for barriers (i.e., number of times participant responded generally unavailable or somewhat available). Reported p-values are for Fisher’s exact test.
