Figure 1
Key Aims of Memorandum of Understanding between MOH and VCU.
Table 1
Activities Supporting Trauma & EMS Capacity in Rwanda.
| THEMES AND PROJECTS | ACTIVITIES | FUNDING | SUCCESSES | CHALLENGES |
|---|---|---|---|---|
| Shared Mental Model | ||||
| Leadership | Immersion in EMS, emergency medicine, trauma care, cardiac emergency care, critical care, hospital admin at VCU, state EMS systems at Virginia Department of Health Office of EMS, EMS field organization at Richmond Ambulance Authority | VCU-Crone Scholars Program; Philanthropy; VCU SOM | 7 Leaders from EMS, EM, Injury Policy, MOH; 15 weeks; presentations at VCU, Virginia EMS Symposium, EMS World Expo | Retention of these leaders in Rwanda long enough to develop and implement their shared vision-> continued mentorship and support through ongoing collaboration |
| Advocacy | First Rwanda National Trauma Symposium | NIH NCI P20; VCU SOM | over 100 participants; results published | Potential to be one-off without ongoing momentum and support-> regular meetings to be led by RBC in partnership with stakeholders |
| Clinical Service Delivery | ||||
| Prehospital and Emergency Training Courses | 4 Prehospital/Emergency Courses through train-the-trainers program for trauma, medical, pediatric, and obstetric/neonatal emergencies; Educator course for Instructor core | Rotary Foundation Global Grant | 25 Instructors; > 600 trained doctors, nurses, anesthetists, midwives from provincial and district hospitals; 4 manuscripts submitted; EMS Manual for LMICs in progress | Wide scale-up and periodic refresher training needs further funding-> to be incorporated into annual SAMU outreach budget |
| Standardization of EMS Care through Protocols and Checklists | 42 protocols and checklists created, implemented as national prehospital standard for SAMU | NIH Fogarty R21 | Checklist implementation being evaluated for 6 index conditions currently | Regular QI processes to maintain quality-> support through ongoing collaboration |
| Systems and Infrastructure | ||||
| QI and Research Capacity | Short mentored research program – 4 teams; Masters’ degrees support for nurses, anesthetists, doctors from SAMU and CHUK | NIH Fogarty R21; VCU SOM | Presentations at African Congress on Emergency Medicine and College of Surgeons of East, Central and Southern Africa; 11 staff completing Masters’ degrees | Regular research projects by SAMU -> support through ongoing collaboration |
| Data Infrastructure – Prehospital Registry | REDCap prehospital registry 2013–2018,
Google dashboard 2018-present | Harvard Postgraduate Fellowship/AAS Global Surgery Fellowship | >15,000 prehospital records captured | Ongoing use and maintenance -> led by SAMU staff |
| Data Infrastructure – Multi-Institutional Hospital-Based Trauma Registry | WHO Trauma registry adopted, customized, and implemented across 4 Referral hospitals in Rwanda | NIH NCI P20 | >5000 trauma patient records captured in initial 12 months | Ongoing use and maintenance -> led by RBC and hospital staff with ongoing support from WHO |
| Emergency Communication Systems and Innovation | Private-Academic-Government collaboration with Rwanda Build; Concept design for Rwanda912 mobile health platform for emergency communications and coordination selected top 5 finalists at Toyota Mobility Ideathon and Smart Kigali Competition in 2018 | VCU SOM; NIH Fogarty R21; Toyota Finalist Award; Smart Kigali Finalist | Formal Engagement from MOH; Application submitted to NIH for software development and implementation research | Funding to develop and implement -> in progress |
[i] AAS – Association for Academic Surgery, EM – Emergency Medicine, EMS – Emergency Medical Services, MOH – Ministry of Health of Rwanda, NIH – National Institutions of Health, NCI – National Cancer Institute, QI – Quality Improvement, VCU SOM – Virginia Commonwealth University School of Medicine.
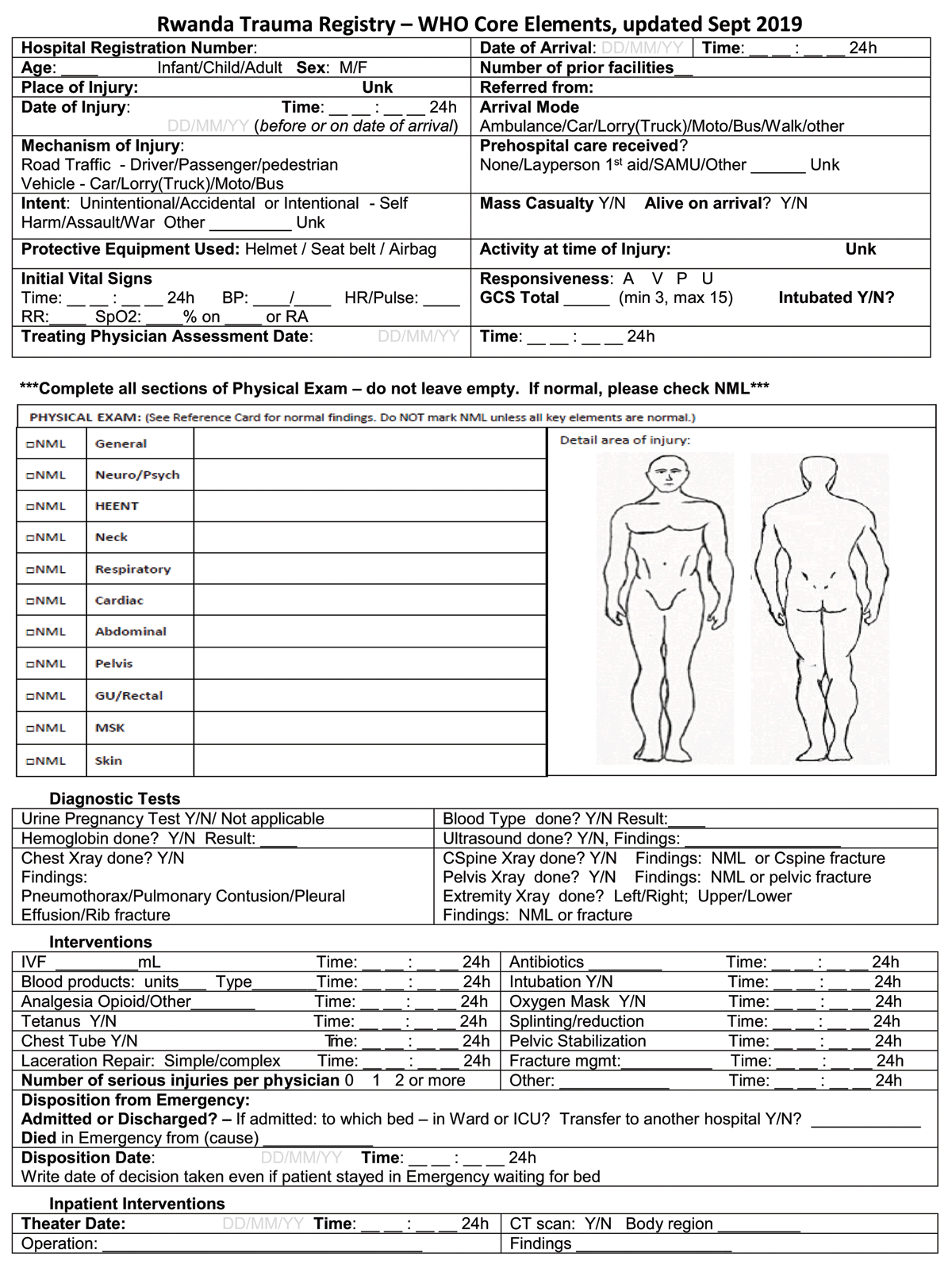
Figure 2
Rwanda Trauma Registry Form.
